Reporting Patient Incidents: A Best Practices Guide - i-Sight
27 hours ago · What to Include In a Patient Incident Report . A patient incident report should include the basic information about the incident: the who, what, where, when and how. You should also add recommendations on how to address the problem to reduce the risk of future incidents. Every facility has different needs, but your incident report form could include: >> Go To The Portal
Incident reporting needs may vary by organization, but this basic information is generally required: Patient name, date of birth, and hospital ID number Names of any other affected individuals (e.g., staff or visitors)
What should be included in a patient incident report?
A patient incident report should include the basic information about the incident: the who, what, where, when and how. You should also add recommendations on how to address the problem to reduce the risk of future incidents. Every facility has different needs, but your incident report form could include:
Do you need to file an incident report?
When a situation is significant—resulting in an injury to a person or damage to property—it’s obvious that an incident report is required. But many times, seemingly minor incidents go undocumented, exposing facilities and staff to risk.
What information do I need to record after an incident?
If the incident involved any personal injury or damage to any property, you must record the information. If an injury has transpired, register any facility name, and address where a person sought treatment.
Who is responsible for filing incident reports in a hospital?
The busiest hospital personnel, nurses, and doctors are mainly responsible for filing incident reports. Due to their busy and often overworked schedule, they sometimes fail to report incidents.
What information should be documented in an incident log?
The incident log documents all details about an event, including date, time, what happened, who was involved and who witnessed the event. You should fill out the incident log immediately after an incident.
What should be included in an incident report nursing?
What Information Do You Put in an Incident Report?Detailed description of the event with events listed chronologically.Witnesses or injured party statements.Injuries sustained by the person(s) as a result of the incident or the outcome.Actions taken immediately after the incident occurred.Treatments administered.More items...•
Which three pieces of information should an incident report include?
It should include:the names and positions of the people involved.the names of any witnesses.the exact location and/or address of the incident.the exact time and date of the occurrence.a detailed and clear description of what exactly happened.a description of the injuries.
What are the five elements of good incident report?
The key tasks to mention in the workflow includes notification of the incident, identification of responsible, interviews, investigation and analysis, conclusion, sharing learnings and implementation.
What should be included in an incident report for healthcare?
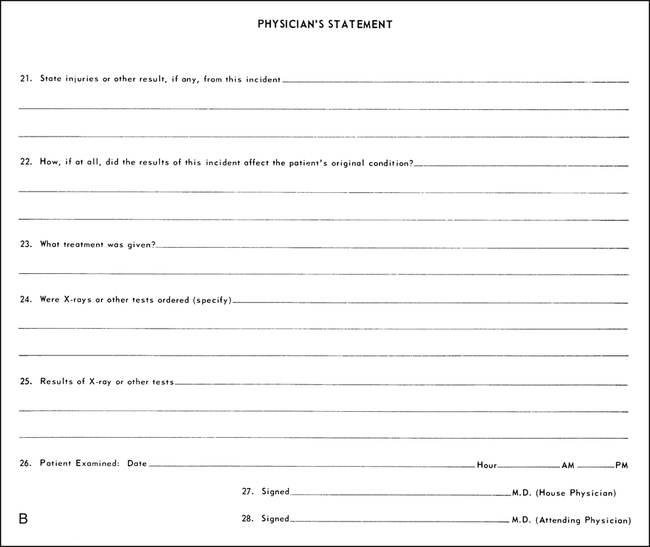
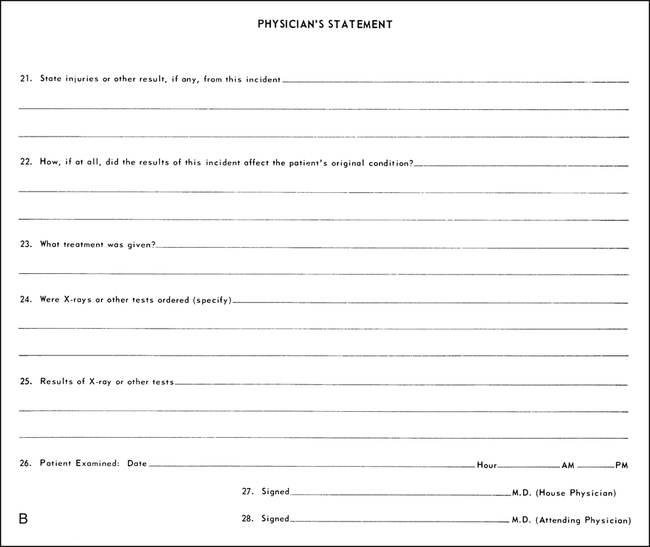
Information required on an incident reporting formPatient name and hospital number/date of birth.Date and time of incident.Location of incident.Brief, factual description of incident.Name and contact details of any witnesses.Harm caused, if any.Action taken at the time.More items...
What makes a good incident report?
Effective Incident Reports identify the facts and observations. They avoid inclusion of personal biases; they do not draw conclusions/predictions, or place blame. Effective Incident Reports use specific, descriptive language and identified the action(s) taken by staff as a result of the unusual incident.
Which of the below information should be there in incident report?
An incident report may include the following information: The circumstances surrounding the incident. Date, time, and location of the incident. The details on witnesses and victims, if any.
How do you document an incident?
State the specific date, day, time, and location of the incident. In addition to stating your presence and the presence of the person(s) involved directly in the event, state the names of any and all witnesses to the incident.
What should be documented in the safety event report for this patient?
Filling Out an Effective Incident Report Include the full names of those involved and any witnesses, as well as any information you have about how, or if, they were affected. Add other relevant details, such as your immediate response—calling for help, for example, and notifying the patient's physician.
What data should be contained in an incident report?
8 Items to Include in Incident ReportsThe time and date the incident occurred. ... Where the incident occurred. ... A concise but complete description of the incident. ... A description of the damages that resulted. ... The names and contact information of all involved parties and witnesses. ... Pictures of the area and any property damage.More items...•
Why is incident reporting important?
Improving patient safety is the ultimate goal of incident reporting. From enhancing safety standards to reducing medical errors, incident reporting helps create a sustainable environment for your patients. Eventually, when your hospital offers high-quality patient care, it will build a brand of goodwill.
How long does it take to file an incident report?
Usually, nurses or other hospital staff file the report within 24 to 48 hours after the incident occurred. The outcomes improve by recording incidents while the memories of the event are still fresh.
What is an incident in healthcare?
An incident is an unfavourable event that affects patient or staff safety. The typical healthcare incidents are related to physical injuries, medical errors, equipment failure, administration, patient care, or others. In short, anything that endangers a patient’s or staff’s safety is called an incident in the medical system.
Why is reporting important in healthcare?
Reporting can also make healthcare operations more economically effective. By gathering and analyzing incident data daily, hospitals’ can keep themselves out of legal troubles. A comprehensive medical error study compared 17 Southeastern Asian countries’ medical and examined how poor reporting increases the financial burden on healthcare facilities.
What is clinical risk management?
Clinical risk management, a subset of healthcare risk management, uses incident reports as essential data points. Risk management aims to ensure the hospital administrators know their institution performance and identify addressable issues that increase their exposure.
What are near miss incidents?
#2 Near Miss Incidents 1 A nurse notices the bedrail is not up when the patient is asleep and fixes it 2 A checklist call caught an incorrect medicine dispensation before administration. 3 A patient attempts to leave the facility before discharge, but the security guard stopped him and brought him back to the ward.
What is clinical incident?
A clinical incident is an unpleasant and unplanned event that causes or can cause physical harm to a patient. These incidents are harmful in nature; they can severely harm a person or damage the property. For example—
When is an incident report required?
When a situation is significant—resulting in an injury to a person or damage to property —it’s obvious that an incident report is required. But many times, seemingly minor incidents go undocumented, exposing facilities and staff to risk. Let’s discuss three hypothetical situations.
How to write an incident report?
In determining what to include in an incident report and which details can be omitted, concentrate on the facts.#N#Describe what you saw when you arrived on the scene or what you heard that led you to believe an incident had taken place. Put secondhand information in quotation marks, whether it comes from a colleague, visitor, or patient, and clearly identify the source.# N#Include the full names of those involved and any witnesses, as well as any information you have about how, or if, they were affected .#N#Add other relevant details, such as your immediate response—calling for help, for example, and notifying the patient’s physician. Include any statement a patient makes that may help to clarify his state of mind, as well as his own contributory negligence.#N#It’s equally important to know what does not belong in an incident report.#N#Opinions, finger-pointing, and conjecture are not helpful additions to an incident report.#N#Do not:
Why is incident reporting important?
An incident report invariably makes its way to risk managers and other administrators, who review it rapidly and act quickly to change any policy or procedure that appears to be a key contributing factor to the incident. The report may also alert administration that a hospital representative should talk to a patient or family to offer assistance, an explanation, or other appropriate support. That’s an important function because such communication can be the balm that soothes the initial anger—and prevents a lawsuit.
Why is it important to file incident reports?
Filing incident reports that are factually accurate is the only way to help mitigate potentially disastrous situations arising from malpractice and other lawsuits. It’s your responsibility to record unexpected events that affect patients, colleagues, or your facility, regardless of your opinion of their importance.
What is the duty of a nurse?
As a nurse, you have a duty to report any incident about which you have firsthand knowledge. Failure to do so could lead to termination. It could also expose you to liability, especially in cases of patient injury. Protect yourself and your patients by filing incident reports anytime unexpected events occur.
What happens when incident reports are filled out properly?
If the incident report has been filled out properly with just the facts, there should be no reason to be concerned about how it’s used. The danger comes only when incident reports contain secondhand information, conjecture, accusations, or proposed preventive measures that do not belong in these reports.
Why is it important to talk to a hospital representative?
That’s an important function because such communication can be the balm that soothes the initial anger —and prevents a lawsuit.
What is incident report?
An incident report is an electronic or paper document that provides a detailed, written account of the chain of events leading up to and following an unforeseen circumstance in a healthcare setting.
Why are incident reports important?
Incident reports are used to communicate important safety information to hospital administrators and keep them updated on aspects of patient care for the following purposes: Risk management. Incident report data is used to identify and eliminate potential risks necessary to prevent future mistakes.
How long does it take to complete an incident report?
To ensure the details are as accurate as possible, incident reports should be completed within 24 hours by whomever witnessed the incident. If the incident wasn’t observed (e.g., a patient slipped, fell, and got up on his own), then the first person who was notified should submit it.
What are some examples of reportable events in New York?
Examples: adverse reactions, equipment failure or misuse, medication errors.
What are the concerns of nurses?
Stressing over getting the report done or about what to include are common concerns for nurses — not to mention worrying about whether filing the report reflects badly on your performance. Mistakes happen all the time, and healthcare facilities are not immune.
A good incident report
Includes chronological dates, times, and locations for when/where the incident occurred
When should the form be submitted
Incident reports should be turned in as soon as possible after the incident so details remain fresh in your memory, however all reports should be submitted by 8:00am the morning following the incident to ensure timely processing.
How to submit an incident report
Submit information through the online incident report form . A link to the form can also be found on the Resources for RAs page on the Residence Life website.
Sample Good Incident Report
At approximately 12:35am on Thursday, September 26, 2015 Resident Assistant (RA) Peter Parker was doing rounds on second floor of Pauley-Rorem Hall when he heard loud music and yelling coming from room 231.
Sample Bad Incident Report
I was chilling in Pfeif and heard something. I knocked on the door and Joe answered. I told him he couldn't drink in his room because it was substance free. Joe shoulda known that, cuz he'd been to my floor meeting. I told Joe and the other guy in the room to dump out the beer.
What is incident report?
1. An Incident Report Must Be Accurate and Specific. When you write an incident report, you must be specific and accurate about the details, not merely descriptive. For example, instead of writing "the old patient", it is more accurate to describe him as "the 76-year old male patient".
How to organize an incident report?
How a report is organized depends on the complexity of the incident and the type of report being written. Usually, writing in chronological order is the simplest way to organize a report. However, an inspection incident report may be written by enumerating details according to findings. 5. A Good Incident Report Must Be Clear.
What is the best way to write an incident report?
It is also best to write in an active voice, which is more powerful and interesting than the passive voice. 2. A Good Incident Report Must Be Factual and Objective.
What abbreviations should be used in an incident report?
A Good Incident Report Must Only Include Proper Abbreviations. The use of abbreviations may be appropriate in certain cases, such as the use of Dr. Brown and Mr. Green, instead of writing Doctor or Mister.
Do you have to include your opinion in a report?
If you must include an opinion in your report, it is best to state it with the similar description that appears on some incident report samples: "In my opinion, there were too many people in the overloaded bus. In fact, there were 80 persons inside, when a bus of this size is only allowed to carry 70 individuals."
Do you need an incident report in court?
Your incident report may be needed in court someday and you should be prepared to be questioned based on your report. So the more details you have on your report, the less you have to depend on your memory and the more credible you are.
Can an incident report be brought in as evidence?
The incident report cannot be brought in as evidence unless it's noted in the chart. So no note...no incident report. I know to me it sounds kind of crappy because it seems to protect the hospital and could cause "harm" to the pt if there is a suit...but policy is policy. This policy may cover my butt sometime.
Is an incident report considered an internal investigation?
Your incident report is considered an internal investigation document. You should never document in your nurses notes that an incident report was completed. If you do, your report may be used in court. They are only to be used internally to investigate the incident.
What information should be included in an incident report?
It should include: the names and positions of the people involved. the names of any witnesses. the exact location and/or address of the incident. the exact time and date of the occurrence. a detailed and clear description of what exactly happened.
How to write an incident report?
The incident report must be factual and complete. It should include: 1 the names and positions of the people involved 2 the names of any witnesses 3 the exact location and/or address of the incident 4 the exact time and date of the occurrence 5 a detailed and clear description of what exactly happened 6 a description of the injuries
What is the report required to be factual?
The report must be factual and be free of sarcasm, condescending statements, and judgmental remarks. The person in charge of the written reporting is expected to rely purely on facts, able to detect and avoid personal biases and opinions.
What is the best practice for filling out an incident report?
Best Practices for Filling Out Incident Report Forms. Every company must have a protocol for incident reporting. Only people of authority should be given access to this document. They can use it for documentation of unfortunate events, management of risks, and creation of safety measures as mandated by the law.
What to do if you are not sure if a report is necessary?
If you’re not sure whether a report is necessary, consider the wisdom of “better safe than sorry.”. If the incident is extreme, it may be good to immediately call the police. Finally, always check with your country's labor regulations to ensure that your company is fully compliant.
How long does it take to fill out a report?
Fill out the report form and file it within 24 hours. Include small details and all pertinent data. The supervisor should verify the information in the report. Only the person that is directly involved in the incident can fill out the form. Be thorough and avoid making corrections.
Why is it important to write a report?
Because no information must be left out, it’s crucial to start writing the report as soon as possible. The longer you wait, the more difficult it can be to accurately document the details of the incident. It’s best to do the write-up when the everyone’s memory of the incident is still fresh.
What to include in an incident report?
Incident report has all of that, PLUS it looks at what could have contributed to it and what could be fixed. In addition to all the of the above, the incident report would include: 1 What medications the patient was on (medication list) 2 Who was involved (Nurses Y and Z was caring for the patient at the time) 3 Lapses--accidental or intentional--in care (Nurse Y didn't check the BP before giving that AM Norvasc) 4 Possible contributing factors (3 antihypertensives PLUS Zyrexa? Why didn't patient call for help if he felt dizzy? Did someone even educate the patient to do this?) 5 How it could have been corrected (move patient closer to nurses' station to keep a better eye out, have MD review meds to see if he really needs 3 HTN meds)
What is medical record?
Medical record has the facts & the treatment. There is no musing about what could have caused it, no finger-pointing or assigning blame, no troubleshooting other than documenting what interventions you did (e.g., educated patient, used bed alarm, etc.).
Is incident report part of medical record?
Incident reports are NOT part of a medical record. Take your patient fall. The medical record is going to summarize the facts of what happened and the medical treatment rendered. "Patient found on floor of the room bleeding from a 2cm laceration to their left temple. Patient stated they got dizzy and fell.
Popular Posts:
- 1. how to sign up for patient portal at southern bone and joint specialists
- 2. patient portal me honorhealth
- 3. patient portal rainbow pediatrics
- 4. mdvip patient portal login
- 5. imadoctors patient portal
- 6. x ray report of pneumonia patient
- 7. patient portal milestone medical
- 8. dr stone patient portal
- 9. patient portal mind
- 10. dr rachel heinle christiana care portal patient