Reporting Patient Safety Events | PSNet
2 hours ago · A patient incident report, according to Berxi, is “an electronic or paper document that provides a detailed, written account of the chain of events leading up to and following an unforeseen circumstance in a healthcare setting.”. Reports are typically completed by nurses or other licensed personnel. >> Go To The Portal
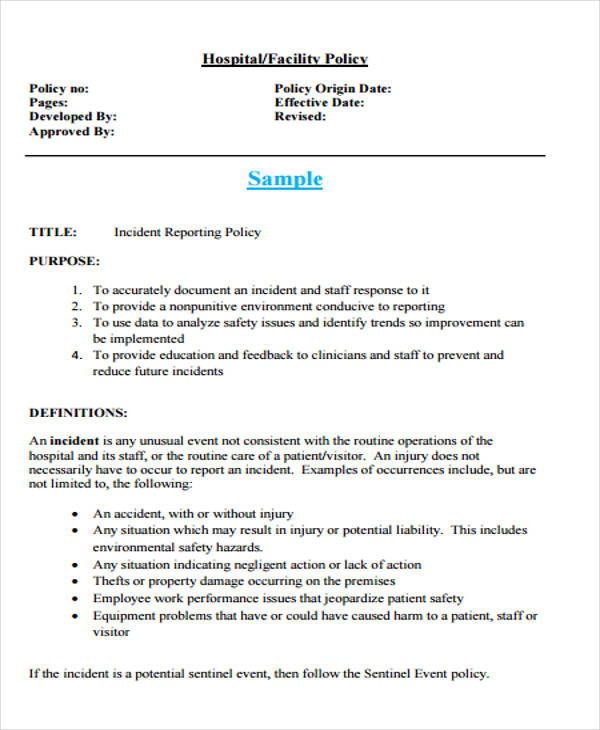
A patient incident report is a form that provides a detailed account of an incident that takes place in a healthcare setting, such as a hospital. Generally, a nurse will complete this report, which might outline the events leading up to a fall or a different kind of threat to a patient’s safety.
Full Answer
What is a patient incident?
As defined by Berxi, a patient incident report is “a detailed, written description of the chain of events leading up to and following an unforeseen scenario in a healthcare context,” which can be either computerized or paper-based. Nurses or other qualified professionals are often responsible for completing reports.
What is a hospital incident report?
The man has not been identified. Medical staff at the hospital told investigators that the man's injuries were not consistent with a traffic accident. The incident report indicates that the man was injured by a gunshot. However, the official cause of death ...
How to write a good accident or incident report?
- The type of incident that took place
- Where the incident happened
- The date, day and time of the incident
- Names of the people involved
- Injuries that were obtained
- Medical treatment that may have been required
- Equipment that was involved
- Events leading up to the incident that could have contributed to it taking place
How do I get an incident report?
Please bring the following to your appointment:
- Appointment confirmation code from Eventbrite.
- Completed Request Forms DPS-96-C
- Payment in the amount of $16.00 per incident requested. Check or Money Order payable to “Treasurer-State of CT”.
- Cash payments must be the exact dollar amount. Change cannot be provided.
What is AHRQ common format?
What is the Patient Safety and Quality Improvement Act?
How is event reporting used in health care?
What is patient safety event reporting?
What is PSNet perspective?
Why are event reports limited?
What is structured mechanism?
See more
About this website

How do you write an incident report on a patient?
What to Include In a Patient Incident ReportDate, time and location of the incident.Name and address of the facility where the incident occurred.Names of the patient and any other affected individuals.Names and roles of witnesses.Incident type and details, written in a chronological format.More items...•
What is patient safety reporting?
Patient Safety Reporting (PSR) gives military treatment facility personnel the ability to anonymously report medical events that impact the safety of patients.
What incidents should be reported in healthcare?
Incident reporting best practices in healthcareA patient makes a complaint.A medication error occurs.A medical device malfunctions.Anyone—patient, staff member, or visitor—is injured or involved in a situation with the potential for injury.
What is the incident reporting process in healthcare?
Background. Incident reporting (IR) in health care has been advocated as a means to improve patient safety. The purpose of IR is to identify safety hazards and develop interventions to mitigate these hazards in order to reduce harm in health care.
What is an example of a patient safety event?
A patient safety incident occurs but does not result in patient harm – for example a blood transfusion being given to the wrong patient but the patient was unharmed because the blood was compatible. or expected treatment – for example he/she did not receive his/her medications as ordered.
What is the nurse's responsibility regarding incident reporting?
Nurses have a duty to report any error, behaviour, conduct or system issue affecting patient safety. This accountability is found in section 6.5 of the Code of Conduct. Medications and devices prescribed to patients can cause unforeseen and serious complications.
What are the 4 types of incident reports?
Common Types of Incident ReportsWorkplace. Workplace incident reports detail physical events that happen at work and affect an employee's productivity. ... Accident or First Aid. ... Safety and Security. ... Exposure Incident Report.
Who is responsible for reporting a patient safety occurrence?
3. Reporting- when a patient safety event has been identified, the event should be immediately reported. The preferred method of reporting is through the safety online system. At a minimum the event should be reported to the manager or immediate supervisor.
Why reporting is necessary for patient safety?
Reporting systems (frequently referred to as reporting and learning systems) capture patient safety concerns, hazards and/or incidents and are meant to trigger action, facilitate communication, response, learning and improvement.
Patient Safety Event Reporting - National Quality Forum
The National Quality Forum (NQF) operates under a three-part mission to improve the quality of American healthcare by: • building consensus on national priorities and goals for performance improvement and working in partnership to achieve them;
Serious Reportable Adverse Events in Health Care
Serious Reportable Adverse Events 341 quality measurement to strategies for quality improvement, providing leadership, disseminating information, and exchanging knowledge and ideas.
Reporting Patient Incidents: A Best Practices Guide | i-Sight
Each year in the United States, as many as 440,000 people die from hospital errors including injuries, accidents and infections. Many of those deaths could have been prevented if medical facilities used better documentation of incidents. Complete, timely patient incident reports provide valuable information for medical facilities.
The Importance of Reporting Patient Safety Events, or ... - Issuetrak
When an adverse event occurs in a hospital that results in a patient being harmed or put in danger, that incident is supposed to be reported. Adverse events can include a patient fall, medication or treatment errors, patient information breaches, or injuries sustained due to equipment failure.
Adverse event documentation and reporting
Page 1 of 7 SOP: Adverse event documentation and reporting Version 1, dated 4-Nov-2015 Title: Adverse event documentation and reporting Document ID: 005 Version: 1.0 Author: Clinical Research and Development Office (CRDO) – Fiona Williams Author Signature: Date: 4 November 2015 The author is signing to confirm the technical content of this document
For the general public
Record incidents directly on the NRLS via our e-form for patients and public.
For healthcare staff
Healthcare staff are encouraged where possible to record all patient safety incidents on their local risk management systems. These reports will then be routinely uploaded to the NRLS to support national learning. Healthcare staff unable to use a local risk management system can also record incidents directly on the NRLS via the e-forms below.
Before you submit your report
It is important that you acknowledge, understand and accept the following before submitting your report:
Why is it important to review patient incidents?
Reviewing incidents helps administrators know what risk factors need to be corrected within their facilities , reducing the chance of similar incidents in the future.
Why is it important to know that an incident has occurred?
Knowing that an incident has occurred can push administrators to correct factors that contributed to the incident. This reduces the risk of similar incidents in the future. Quality control. Medical facilities want to provide the best care and customer service possible.
Why choose a platform that is web-enabled for quick reporting?
You’ll never miss important details of a patient incident because you can file your report right at the scene. A platform with HIPAA-compliant forms built in makes your workflow more efficient and productive, ensuring patient incidents are dealt with properly.
Why do we use resolved patient incident reports?
Using resolved patient incident reports to train new staff helps prepare them for real situations that could occur in the facility. Similarly, current staff can review old reports to learn from their own or others’ mistakes and keep more incidents from occurring. Legal evidence.
What to include in an incident report?
Every facility has different needs, but your incident report form could include: 1 Date, time and location of the incident 2 Name and address of the facility where the incident occurred 3 Names of the patient and any other affected individuals 4 Names and roles of witnesses 5 Incident type and details, written in a chronological format 6 Details and total cost of injury and/or damage 7 Name of doctor who was notified 8 Suggestions for corrective action
How long does it take to file a patient incident report?
Patient incident reports should be completed no more than 24 to 48 hours after the incident occurred.
Why is it important to document an incident?
Even if an incident seems minor or didn’t result in any harm, it is still important to document it. Whether a patient has an allergic reaction to a medication or a visitor trips over an electrical cord, these incidents provide insight into how your facility can provide a better, safer environment.
What is the number to call 911?
If you are having thoughts of harming yourself, please call the National Suicide Prevention Lifeline at 1-800-273-TALK (8255). Online: Submit a new patient safety event or concern. Online: Submit an update to your incident (You must have your incident number)
Can the Joint Commission accept medical records?
By policy, The Joint Commission cannot accept copies of medical records, photos or billing invoices and other related personal information. These documents will be shredded upon receipt. Download the form for reporting a patient safety concern by mail.
What Is Patient Incident Report?
Incidents are potentially dangerous incidents that have the potential to put patients or staff members at risk. Medical events are anything that can happen in the healthcare industry and can be caused by anything from equipment failure to injuries to poor patient care. Medical events can occur for a variety of reasons.
What Is the Purpose of the Patient Incident Report?
Patient incident reports provide information to facility officials about what happened to the patient. The information provided in the reports provides light on the steps that must be performed in order to deliver excellent patient care while also maintaining the smooth operation of your facility.
What to Include in a Patient Incident Report?
A patient incident report should include the bare minimum of information regarding the occurrence, such as who was involved, what happened, where it happened, when it happened, and how it happened. You should also include ideas on how to deal with the problem in order to lessen the likelihood of further instances occurring.
What Are the Benefits of Patient Safety Reporting?
Setting the relevant key performance indicators in your organization gets easier as a result of healthcare data analysis and analysis. You can receive the following significant advantages from filing a complaint:
Types of Incident Report
Even if an occurrence appears to be insignificant or has not resulted in any harm, it is still crucial to record it. Whether a patient has an allergic response to a drug or a visitor slips over an electrical cord, these occurrences provide valuable insight into how your facility can create a better, more secure environment for its visitors.
How to Create an Efficient Patient Incident Report
One thorough incident report should address all of the fundamental questions — who, what, where, when, and how — and provide full answers. The majority of hospitals adhere to a predetermined reporting format that is tailored to their own organizational requirements. An incident report, on the other hand, must include the following information:
FAQs
It is possible to acquire information on patient safety occurrences through the use of incident-reporting systems (IRSs). Even if they come with a significant financial cost, however, little is known regarding their usefulness.
What is an incident in healthcare?
An incident is an unfavourable event that affects patient or staff safety. The typical healthcare incidents are related to physical injuries, medical errors, equipment failure, administration, patient care, or others. In short, anything that endangers a patient’s or staff’s safety is called an incident in the medical system.
Why is incident reporting important?
Improving patient safety is the ultimate goal of incident reporting. From enhancing safety standards to reducing medical errors, incident reporting helps create a sustainable environment for your patients. Eventually, when your hospital offers high-quality patient care, it will build a brand of goodwill.
Why is reporting important in healthcare?
Reporting can also make healthcare operations more economically effective. By gathering and analyzing incident data daily, hospitals’ can keep themselves out of legal troubles. A comprehensive medical error study compared 17 Southeastern Asian countries’ medical and examined how poor reporting increases the financial burden on healthcare facilities.
What is clinical risk management?
Clinical risk management, a subset of healthcare risk management, uses incident reports as essential data points. Risk management aims to ensure the hospital administrators know their institution performance and identify addressable issues that increase their exposure.
What are near miss incidents?
#2 Near Miss Incidents 1 A nurse notices the bedrail is not up when the patient is asleep and fixes it 2 A checklist call caught an incorrect medicine dispensation before administration. 3 A patient attempts to leave the facility before discharge, but the security guard stopped him and brought him back to the ward.
How much of healthcare is wasted?
Even the World Health Organisation (WHO) has estimated that 20-40% of global healthcare spending goes waste due to poor quality of care. This poor healthcare quality leads to the death of more than 138 million patients every year. Patient safety in hospitals is in danger due to human errors and unsafe procedures.
How long does it take to file an incident report?
Usually, nurses or other hospital staff file the report within 24 to 48 hours after the incident occurred. The outcomes improve by recording incidents while the memories of the event are still fresh.
What is AHRQ common format?
AHRQ has also developed Common Formats —standardized definitions and reporting formats for patient safety events— in order to facilitate aggregation of patient safety information. Since their initial release in 2009, the Common Formats have been updated and expanded to cover a broad range of safety events.
What is the Patient Safety and Quality Improvement Act?
The legislation provides confidentiality and privilege protections for patient safety information when health care providers work with new expert entities known as Patient Safety Organizations (PSOs). Health care providers may choose to work with a PSO and specify the scope and volume of patient safety information to share with a PSO. Because health care providers can set limits on the ability of PSOs to use and share their information, this system does not follow the pattern of traditional voluntary reporting systems. However, health care providers and PSOs may aggregate patient safety event information on a voluntary basis, and AHRQ will establish a network of patient safety databases that can receive and aggregate nonidentifiable data that are submitted voluntarily. AHRQ has also developed Common Formats —standardized definitions and reporting formats for patient safety events—in order to facilitate aggregation of patient safety information. Since their initial release in 2009, the Common Formats have been updated and expanded to cover a broad range of safety events.
How is event reporting used in health care?
A 2016 article contrasted event reporting in health care with event reporting in other high-risk industries (such as aviation), pointing out that event reporting systems in health care have placed too much emphasis on collecting reports instead of learning from the events that have been reported. Event reporting systems are best used as a way of identifying issues that require further, more detailed investigation. While event reporting utilization can be a marker of a positive safety culture within an organization, organizations should resist the temptation to encourage event reporting without a concrete plan for following up on reported events. A PSNet perspective described a framework for incorporating voluntary event reports into a cohesive plan for improving safety. The framework emphasizes analysis of the events and documenting process improvements arising from event analysis, rather than encouraging event reporting for its own sake.
What is patient safety event reporting?
Patient safety event reporting systems are ubiquito us in hospitals and are a mainstay of efforts to detect patient safety events and quality problems. Incident reporting is frequently used as a general term for all voluntary patient safety event reporting systems, which rely on those involved in events to provide detailed information. Initial reports often come from the frontline personnel directly involved in an event or the actions leading up to it (e.g., the nurse, pharmacist, or physician caring for a patient when a medication error occurred), rather than management or patient safety professionals. Voluntary event reporting is therefore a passive form of surveillance for near misses or unsafe conditions, in contrast to more active methods of surveillance such as direct observation of providers or chart review using trigger tools. The Patient Safety Primer Detection of Safety Hazards provides a detailed discussion of other methods of identifying errors and latent safety problems.
What is PSNet perspective?
A PSNet perspective described a framework for incorporating voluntary event reports into a cohesive plan for improving safety. The framework emphasizes analysis of the events and documenting process improvements arising from event analysis, rather than encouraging event reporting for its own sake.
Why are event reports limited?
The spectrum of reported events is limited, in part due to the fact that physicians generally do not utilize voluntary event reporting systems.
What is structured mechanism?
A structured mechanism must be in place for reviewing reports and developing action plans. While traditional event reporting systems have been paper based, technological enhancements have allowed the development of Web-based systems and systems that can receive information from electronic medical records.