How to Document a Patient Assessment (SOAP) | Geeky …
35 hours ago Vitals taken, O2 @ 4LPM via nasal canula, manual immobilization, c-collar, backboard, patient’s condition improved following treatment (identify which treatment) S. A MPLE REPORT (S) - PT. states his chief complaint is a substernal chest pain lasting 2 hours. PT. states he was sitting at home watching the game as this pain came on acutely. >> Go To The Portal
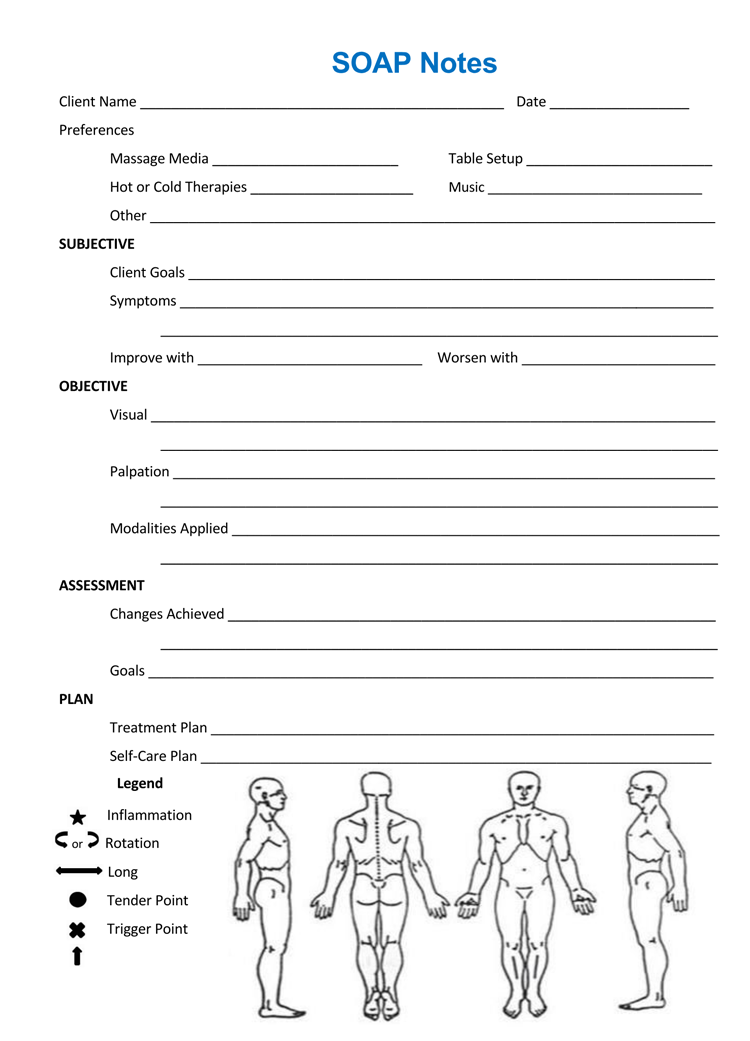
SOAP note
The SOAP note (an acronym for subjective, objective, assessment, and plan) is a method of documentation employed by health care providers to write out notes in a patient's chart, along with other common formats, such as the admission note.
Full Answer
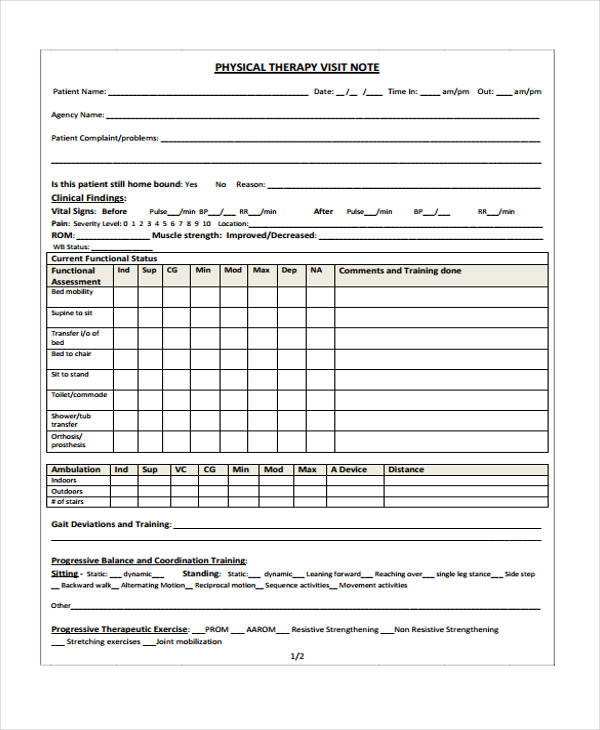
How to document a patient assessment (soap)?
How to Document a Patient Assessment (SOAP) 1 Subjective. The subjective section of your documentation should include how... 2 Objective. This section needs to include your objective observations,... 3 Assessment. The assessment section is where you write your thoughts on the salient issues and... 4 Plan. The final section is the plan,...
What are the benefits of SOAP notes for healthcare providers?
By providing a helpful template for therapists and healthcare providers, SOAP notes can reduce admin time while improving communication between all parties involved in a patient’s care.
Can soap improve documentation in acute surgical receiving?
A quality improvement project using a problem based post take ward round proforma based on the SOAP acronym to improve documentation in acute surgical receiving. Ann Med Surg (Lond).
Why is it important to have a soap in a hospital?
It is essential as proof that the patient is being treated regularly and effectively by different people. SOAP is actually an acronym and it stands for: S ubjective – This basically refers to everything the patient has to say about the issue, concern, problem and intervention procedures.
What are soap reports?
Today, the SOAP note – an acronym for Subjective, Objective, Assessment, and Plan – is the most common method of documentation used by providers to input notes into patients' medical records. They allow providers to record and share information in a universal, systematic and easy-to-read format.
How do you write a soap report?
Tips for Effective SOAP NotesFind the appropriate time to write SOAP notes.Maintain a professional voice.Avoid overly wordy phrasing.Avoid biased overly positive or negative phrasing.Be specific and concise.Avoid overly subjective statement without evidence.Avoid pronoun confusion.Be accurate but nonjudgmental.
What should be included in a SOAP note assessment?
SOAP notes include a statement about relevant client behaviors or status (Subjective), observable, quantifiable, and measurable data (Objective), analysis of the information given by the client (Assessment), and an outline of the next course of action (Planning).
What does SOAP stand for?
Subjective, Objective, Assessment, and PlanHowever, all SOAP notes should include Subjective, Objective, Assessment, and Plan sections, hence the acronym SOAP. A SOAP note should convey information from a session that the writer feels is relevant for other healthcare professionals to provide appropriate treatment.
What are the 4 parts of soap?
The acronym SOAP stands for Subjective, Objective, Assessment, and Plan.
What are the four parts of a SOAP note?
The 4 headings of a SOAP note are Subjective, Objective, Assessment and Plan. Each heading is described below. This is the first heading of the SOAP note....ObjectiveVital signs.Physical exam findings.Laboratory data.Imaging results.Other diagnostic data.Recognition and review of the documentation of other clinicians.
How do you write a clinical SOAP note?
The Plan section of your SOAP notes should contain information on:The treatment administered in today's session and your rationale for administering it.The client's immediate response to the treatment.When the patient is scheduled to return.Any instructions you gave the client.More items...•
How do you write a SOAP note for nursing?
0:105:59How to Make SOAP Notes Easy (NCLEX RN Review) - YouTubeYouTubeStart of suggested clipEnd of suggested clipSo stands for subjective objective assessment and plan let's take a look at each of the fourMoreSo stands for subjective objective assessment and plan let's take a look at each of the four components. So you can understand this neat and organized way of note-taking.
What do you write in the objective of a SOAP note?
Objective means that it is measurable and observable. In this section, you will report anything you and the client did; scores for screenings, evaluations, and assessments; and anything you observed. The O section is for facts and data.
What is SOAP used for in nursing?
Nurses and other healthcare providers use the SOAP note as a documentation method to write out notes in the patient's chart. SOAP stands for subjective, objective, assessment, and plan. Let's take a look at each of the four components so you can understand this neat and organized way of note-taking.
What is SOAP mental health?
SOAP is an acronym that stands for Subjective, Objective, Assessment, Plan. Let's unpack each section of the note.
What is a soap note?
A SOAP note is a documentation method used by medical practitioners to assess a patient’s condition. It is commonly used by doctors, nurses, pharmacists, therapists, and other healthcare practitioners to gather and share patient information. SOAP notes are designed to improve the quality and continuity of patient care by enhancing communication ...
What are the Four Parts of a SOAP Note?
The four parts of a SOAP note are the same as its abbreviation. All four parts are designed to help improve evaluations and standardize documentation:
What is the best software to collect SOAP notes?
Healthcare professionals can use iAuditor, the world’s #1 inspection software, to digitally gather SOAP notes and improve the quality and continuity of patient care. Collect photo evidence for a more informative and descriptive patient record.
Can iAuditor save patient records?
Easily share your findings with other healthcare clinicians and avoid losing track of patient records by securely saving it in the cloud using iAuditor
Can you download soap note templates?
To help you get started we have created SOAP note templates you can download and customize for free.
What is the opening statement for HPI?
The HPI begins with a simple one line opening statement including the patient's age, sex and reason for the visit. Example: 47-year old female presenting with abdominal pain. This is the section where the patient can elaborate on their chief complaint. An acronym often used to organize the HPI is termed “OLDCARTS”:
What is the Creative Commons 4.0 license?
This book is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits use, duplication, adaptation, distribution, and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, a link is provided to the Creative Commons license, and any changes made are indicated.
What is the difference between a sign and a symptom?
Symptoms are the patient's subjective description and should be documented under the subjective heading, while a sign is an objective finding related to the associated symptom reported by the patient. An example of this is a patient stating he has “stomach pain,” which is a symptom, documented under the subjective heading. Versus “abdominal tenderness to palpation,” an objective sign documented under the objective heading.
What does Headss stand for in medical history?
Social History: An acronym that may be used here is HEADSS which stands for Home and Environment; Education, Employment, Eating; Activities; Drugs; Sexuality; and Suicide/Depression.
What is a CC in medical terms?
The CC or presenting problem is reported by the patient. This can be a symptom, condition, previous diagnosis or another short statement that describes why the patient is presenting today. The CC is similar to the title of a paper, allowing the reader to get a sense of what the rest of the document will entail.
What is NCBI bookshelf?
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
What is a comprehensive soap note?
A comprehensive SOAP note has to take into account all subjective and objective information, and accurately assess it to create the patient-specific assessment and plan.
Why do nurses write soap notes?
It is very beneficial to write down notes to keep track of and record the progress of treatments of patients.
What is a soap note?
SOAP notes are a type of documentation which, when used, help generate an organized and standard method for documenting any patient data. Any type of health professionals can use a SOAP note template – nurse practitioners, nurses, counselors, physicians, and of course, doctors. Using these kinds of notes allows the main health care provider ...
Why are soap notes still used?
SOAP notes have been around for some time now and because of their efficiency and functionality, they are still being used now. The very first SOAP note template was created and developed by a brilliant doctor named Lawrence Weed way back in the 1960s. It was done at the University of Vermont as an element of the POMR (Problem-Oriented Medical Record). During those times, objective documentation did not exist so physicians had the tendency to make decisions about treating patients without scientific basis.
What is a soap note template?
A SOAP note template comes in a very structured format though it is only one of the numerous formats health or medical professionals can use. A SOAP note template by a nurse practitioner or any other person who works with the patient enters it into the patient’s medical records in order to update them.
Why do you write a note after a patient is treated?
After you’ve administered treatment to a patient, writing a note about it would inform other physicians that you were able to competently help the patient. On the side of the patient and the family as well, you’d have concrete proof to show them in case they have any questions about the treatment.
What are some examples of factors that affect the quality of a patient?
Some examples of this would be if the patient felt better after taking certain medicines if the patient feels better or worse when in certain positions and other such factors.
Why is it important to have a patient's notes?
Having these notes would prove that there had been regular patient contact throughout the whole treatment period and the stay of the patient in the hospital.
What is a therapy soap note?
Therapy SOAP notes follow a distinct structure that allows medical and mental health professionals to organize their progress notes precisely. [1] As standardized documentation guidelines, they help practitioners assess, diagnose, and treat clients using information from their observations and interactions.
Why are soap notes important?
SOAP notes also play a valuable role in Applied Behavior Analysis, by allowing professionals to organize sessions better and communicate with a client’s other medical professionals. Legally, they may also accompany insurance claims to evidence the service being provided. [4]
What format are therapy notes in?
Laid out in the S, O, A, P format on therapy notes software, they might look like this:
Why do we write notes immediately after therapy?
This way, a practitioner’s in-session time is spent focused on patient engagement and care; writing notes immediately after helps minimize common mistakes such as forgetting details or recall bias.
What is the purpose of assessment in clinical practice?
Assessment: Practitioners use their clinical reasoning to record information here about a patient’s diagnosis or health status. A detailed Assessment section should integrate “subjective” and “objective” data in a professional interpretation of all the evidence thus far, and
Is ABA SOAP a private document?
It is important to remember that ABA SOAP notes, as psychotherapeutic documents, must be stored privately. They may form part of a client’s overall medical file other therapy notes.
Can you make a soap note on the spot?
This way, notes can be made on the spot from a tablet or smartphone.
SOAP note example for Nurse or Nurse Practitioner
John reports that he is feeling 'tired' and that he 'can't seem to get out of bed in the morning.' John is 'struggling to get to work' and says that he 'constantly finds his mind wondering to negative thoughts.' John stated that his sleep had been broken and he does not wake feeling rested.
SOAP note example for Psychotherapist
Stacey reports that she is 'feeling good' and enjoying her time away. Stacey reports she has been compliant with her medication and using her meditation app whenever she feels her anxiety.
SOAP note example for Paediatrician
Mrs. Jones states that Julia is "doing okay." Mrs. Jones said her daughter seems to be engaging with other children in her class. Mrs. Jones said Julia is still struggling to get to sleep and that "she may need to recommence the magnesium." Despite this, Mrs. Jones states she is "not too concerned about Julia's depressive symptomology.
SOAP note example for Social Worker
Martin has had several setbacks, and his condition has worsened. Martin reports that the depressive symptoms continue to worsen for him. He feels that they are 'more frequent and more intense. Depressive symptomology is chronically present.
SOAP note example for Psychiatrist
Ms. M. states that she is "doing okay." Ms. M. states that her depressive symptomatology has improved slightly; she still feels perpetually "sad." Ms. M.
SOAP note example for Therapist
"I'm tired of being overlooked for promotions. I don't know how to make them see what I can do." Frasier's chief complaint is feeling "misunderstood" by her colleagues.
SOAP note example for Counselor
David states that he continues to experience cravings for heroin. He desperately wants to drop out of his methadone program and revert to what he was doing.
What Are The Four Parts of A Soap Note?
Soap Note Example – How to Write & What Format
Use A Template For Your Notes
Popular Posts:
- 1. providence medical center patient portal
- 2. central bucks urology patient portal
- 3. a patient developes a rash on amoxicillin should a nurse stop it or report to provider first
- 4. st joseph nashua patient portal
- 5. st joseph hospital nashua nh patient portal
- 6. fort washington medical center patient portal
- 7. sign up for emory patient portal
- 8. patient portal nc
- 9. wilson stream family practice patient portal athenahealth
- 10. cgh mextmd patient portal