Patient Fall Incident Report Example - signNow
30 hours ago To prevent patient injury and decrease falls nurses need to communicate with CNA’s at the beginning of their shift and give reports on high fall risk patients and the proper utilization of bed and chair alarm. Also, nurses must assess risks and act accordingly. Most falls occur in the patient’s room while attempting to… >> Go To The Portal
Full Answer
How are Falls recorded in a nursing report?
Generally, mishaps such as falls are recorded in an incident report. After the fall, a nurse and a medical provider will likely perform an examination of the patient and document their findings.
How do I generate an incident report for a fall?
Generate an incident report for every fall that occurs. The incident report will need to contain, at a minimum: The fact that the incident being reported was a fall. The patient in whom the fall occurred. The date the fall occurred. The unit the patient was assigned to at the time of the fall.
What is the incidence of falls in hospital?
Medical-Surgical: 3.92 falls/1,000 patient days. Medical: 4.54 falls/1,000 patient days. Rehabilitation: 7.15 falls/1,000 patient days. For more information, see Lake ET, Shang J, Klaus S, et al. Patient falls: association with hospital magnet status and nursing unit staffing. Res Nurs Health 2010;33:413-25.
Why is it important to report patient/resident falls?
It is important that all healthcare organizations take a closer look at what they are doing to report, investigate and analyze patient/resident falls. A proactive approach can lead to a reduction in falls along with a reduction in serious injuries.
How do you document a patient falling?
Start by asking the patient why they think the fall occurred and assess associated symptoms, and then check the patient's vital signs, cranial nerve, signs of skin trauma, consciousness and cognitive changes, and any other pain or points of tenderness that could have resulted from the fall.
What to assess after a patient falls?
After the Fall Check the patient's breathing, pulse, and blood pressure. If the patient is unconscious, not breathing, or does not have a pulse, call a hospital emergency code and start CPR. Check for injury, such as cuts, scrapes, bruises, and broken bones.
How do you measure patient falls?
How To Calculate Fall RateCount the number of falls in the month.Figure out how many beds were occupied each day.Add up the total occupied beds each day for the month (patient bed days).Divide the number of falls by the number of patient bed days for the month.More items...
What is the most common patient activity result in falls?
The most common activity performed at the time of the fall was ambulation (35/183; 19%). Of those who fell during ambulation, the most frequent destinations were: bed to bathroom (37%), bedside commode to bed (11%), and bed to bedside commode (6%).
What is post fall assessment?
A post-fall clinical assessment protocol guides staff in the assessment of patients for potential injury after a fall occurs.
What do nurses do if a patient falls?
It includes the following eight steps:Evaluate and monitor resident for 72 hours after the fall.Investigate fall circumstances.Record circumstances, resident outcome and staff response.FAX Alert to primary care provider.Implement immediate intervention within first 24 hours.Complete falls assessment.More items...
Why is it important to report falls?
Reporting fall incidents provides evidence for accrediting surveyors that the organisation is compliant with requirements of national standards. Health services should aim for minimisation of both falls (particularly repeat falls) and harm from falls.
What are the 3 types of falls?
Falls can be classified into three types:Physiological (anticipated). Most in-hospital falls belong to this category. ... Physiological (unanticipated). ... Accidental.
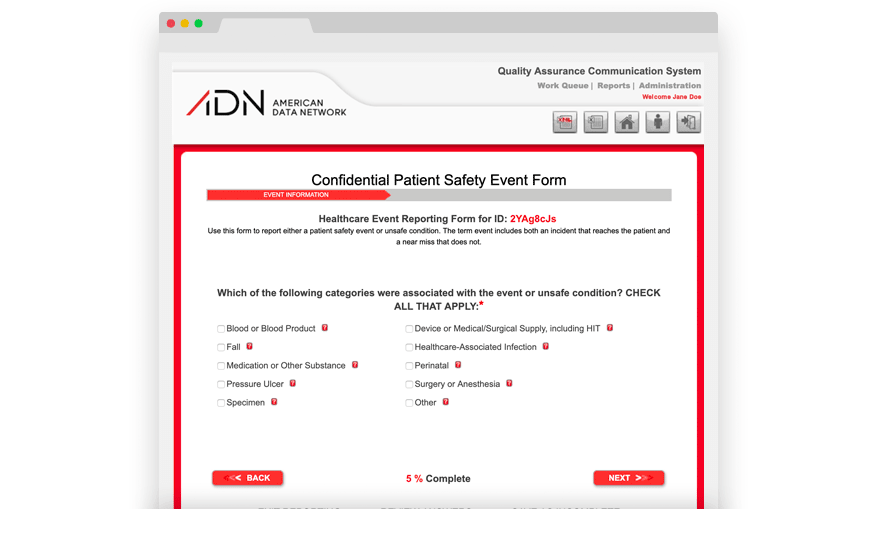
How do hospitals collect data on patient falls?
Some hospitals have electronic incident reporting systems that will make it easier to count the number of falls that have occurred on your unit or in your hospital. ). This will take you to the document Guidelines for Data Collection on the American Nurses Association's National Quality Forum Endorsed Measures.
What are the 5 P's of fall prevention?
The 5 P's of Fall PreventionPain* Is your resident experiencing pain? ... Personal Needs. Does your resident need assist with personal care? ... Position* Is your resident in a comfortable position? ... Placement. Are all your resident's essential items within easy reach? ... Prevent Falls. Always provide person-centered care!
How do you assess elderly after a fall?
8 Things the Doctors Should Check After a FallAn assessment for underlying new illness. ... A blood pressure and pulse reading when sitting, and when standing. ... Blood tests. ... Medications review. ... Gait and balance. ... Vitamin D level. ... Evaluation for underlying heart conditions or neurological conditions.More items...
What are 3 common risk factors associated with patient falls?
Common risk factors for fallsthe fear of falling.limitations in mobility and undertaking the activities of daily living.impaired walking patterns (gait)impaired balance.visual impairment.reduced muscle strength.poor reaction times.More items...•
What is the most common incident in senior living?
Patient falls are the most frequently reported incident in most senior living and community based care settings, according to the Centers for Disease Control and Prevention.
Does falling once double the chance of falling again?
It has also been found that falling once doubles a patient’s chance of falling again. Most falls are caused by a combination of risk factors and the more risk factors, the greater the chances of falling. Given the knowledge that your patient population is at risk for falls, what are you doing as an organization to analyze your incident reports on ...
What are physiological falls?
Anticipated physiological falls are associated with patients that are confused, elderly with dementia or Alzheimer’s. For this population to minimize falls, bed alarms can be utilized but if the bed alarm is constantly going off then a bedside sitter needs to be available to sit with the patient because a nurse with high nurse patient ratio cannot always get to the room whenever a bed alarm rings. Accidental falls are associated with patient being tethered to Tubing’s, walking with IV pole, or tripping over cluttered room. For these patients, hourly rounding is best because every hour if a nursing team member goes in to check on the patient many falls can be reduced. Unanticipated physiological and behavioral falls are not preventable because in these situations any outcome is…
What should a nurse check before discharge?
According to Ruggiero, Smith, Copeland, and Boxer, before discharge, the nurse should check medications to “identify discrepancies, such as medication omission, duplication, change in frequency, change in dose, adjustments, new medications not accompanied by a prescription, or omission of core measures.” This is referred to as a discharge time out. If the nurse is not confident about medications, the nurse can ask a pharmacist to help. This discharge time out ensures that patients are discharged to home with the correct medications list (Ruggiero, Smith, Copeland, & Boxer, 2015). Success will be determined if the patient uses handrails and grab bars as needed, use an assistive device such as a walker correctly, clutter and spills from the floors, and correctly transfer while using safe transfer procedures. These procedures will keep the patient safe and prevent the patient from falling (Ackley & Ladwig,…
Where is a fall report sent?
Once the patient has been evaluated and once the report has been compiled, it is generally sent to the hospital’s or the nursing home’s risk management department. The circumstances surrounding the fall are reviewed with the goal of determining what could prevent something like that from happening again. In most cases, medical professionals are ...
Why are hospitals required to record falls?
Hospitals are required by law to create a safe environment for their patients and family members visiting the hospital facilities. If a patient slips and falls, most hospitals and nursing homes require their staff to document the fall and notify family members or caregivers. The mechanism for recording and reporting a patient fall will vary ...
What are the different types of falls?
In most medical settings, falls are categorized as: 1 Accidental Falls: These are falls that happen among patients who have very low risk of falling, but they fall because of the environment they are in. They may fall out of bed or slip on a wet floor. 2 Anticipated Physiological Falls: These are the most frequent types of falls. They’re usually caused by an underlying condition affecting the patient. A patient may have a problem walking, their gait may be abnormal, they may be battling with dementia, or they may be on medication that is affecting their balance or their perception. 3 Unanticipated Physiological Falls: These are falls with patients who appear to be low risk for falls, however, they suffer a unexpected negative event. They may faint, they may have a seizure, or they may have a heart attack or a stroke. 4 Behavioral Falls: These are falls that happen because a patient becomes unruly or acts out for one reason or another. These includes instances where patients fall on purpose.
What states require licensed healthcare facilities to report falls to the NQF?
The National Quality Forum includes falls that result in death or serious injury as reportable events. States such as Minnesota require licensed healthcare facilities to report falls to the NQF.
What percentage of hospitalized patients fall?
Research shows that up to 50 percent of hospitalized individuals run the risk of falling. Of those who do fall, 50 percent suffer injury. The injuries sustained from hospital falls range ...
How old was the nursing home resident when she fell?
According to reports, a 93-year-old resident fell at the hospital. The nursing home aides assisted her, but no accident reports were written. A few days later, it was noticed that the 93-year-old nursing home resident had extensive bruising on her body. She was taken to the hospital and a few days later died.
Why do medical providers break the standard of care?
In these cases, a medical provider may have broken or violated the appropriate standard of care, because they failed to address conditions that led to a fall or failed to take the necessary precautions to prevent a fall from occurring.
What is fall prevention?
Fall prevention is a National Patient Safety Goal for both hospitals and long-term care facilities. The Joint Commission highlighted the importance of preventing falls in a 2009 Sentinel Event Alert. As noted above, falls with injury are a serious reportable event for The Joint Commission and are considered a "never event" by CMS. The most recent data from AHRQ's National Scorecard on rates of Healthcare Associated Complications (HACs) indicates that fall rates at US hospitals declined by approximately 15% between 2010 and 2015.
What are the components of fall prevention?
They include: Multidisciplinary (rather than solely nursing) responsibility for intervention. Staff and patient education (if provided by health professionals and structured rather than ad hoc).
How does fall prevention work?
Prevention efforts begin with assessing individual patients' risk for falls. There are several existing clinical prediction rules for identifying high-risk patients, but none has been shown to be significantly more accurate than others. Most falls occur in elderly patients, especially those who are experiencing delirium, are prescribed psychoactive medications such as benzodiazepines, or have baseline difficulties with strength, mobility, or balance. However, non elderly patients who are acutely ill are also at risk for falls.
How many hospitalized patients fall each year?
Epidemiologic studies have found that falls occur at a rate of 3–5 per 1000 bed-days, and the Agency for Healthcare Research and Quality estimates that 700,000 to 1 million hospitalized patients fall each year. Patients in long-term care facilities are also at very high risk of falls.
Is a fall considered a serious injury?
Death or serious injury resulting from a fall while being cared for in a health care facility is considered a never event, and the Centers for Medicare and Medicaid Services do not reimburse hospitals for additional costs associated with patient falls. Falls that do not result in injury can be serious as well.
Is there a one size fits all fall prevention program?
There are two overarching considerations in planning a fall prevention program. First, fall prevention measures must be individualized—there is no " one size fits all" method to preventing falls.
When to include falls in a patient report?
Include falls when a patient lands on a surface where you wouldn't expect to find a patient. All unassisted and assisted falls are to be included whether they result from physiological reasons (fainting) or environmental reasons (slippery floor). Also report patients that roll off a low bed onto a mat as a fall.
How long should you count falls?
What should be counted? In measuring fall rates, you will need to count the number of falls and the number of occupied bed days on your unit over a given period of time, such as 1 month or 3 months. To count falls properly, people in your hospital or hospital unit need to agree on what counts as a "fall.".
How does risk factor assessment make a difference?
For risk factor assessment to make a difference, all risk factors identified on the risk factor assessment need to be addressed in the care plans, and the care plans need to be acted on. This requires critical thinking on the part of staff and a tailored approach to each patient based on the individual patient's risk factors. Ensure that the care plans address all areas of risk.
Why do hospital staff feel pressure to underreport borderline cases?
Also, staff may feel pressure to underreport borderline cases because of concern that their unit will compare poorly with other units. Therefore, when a uniform definition of fall is shared throughout the hospital, it needs to be coupled with a culture of trust in which reporting falls is encouraged.
Is there a disadvantage to injurious falls?
The disadvantage is that if there are relatively few injurious falls compared with total falls, it will be hard to tell whether your fall prevention program is making a difference with respect to injuries. Thus, we recommend that both total and injurious fall rates be computed and tracked.
What Should I Do if a Nursing Patient Falls?
Today’s discussion involves what a nurse should do if a patient falls while in their care. We will be talking about the four steps that nurses should take in response to a fall. Our discussion will also focus on what happens if a nurse does not follow the correct procedure.
Four Steps in Response to a Fall
The first thing a nurse should do after a patient falls is to assess the patient.
What Happens If a Nurse Does Not Follow Correct Procedure After a Patient Falls?
Failing to properly treat and document a patient after a fall can result in disciplinary actions with the NC Board of Nursing taken against your license.

Popular Posts:
- 1. univ of penn patient portal.
- 2. calvert memorial hospital patient portal
- 3. regional cardiac & vascular associates patient portal
- 4. westshore family medicine muskegon patient portal
- 5. my uc health patient portal
- 6. augusta university patient information
- 7. rockwood patient portal pin
- 8. concorde patient portal
- 9. allergy patient portal
- 10. wph patient portal