What To Do When Headache Treatments Don't Work
26 hours ago · Compared with patients who never presented for migraine or headache care, those who sought care before the previous 12 months were significantly more likely to be older (mean age of 43.8 years vs ... >> Go To The Portal
Should I talk to my doctor about my headache symptoms?
People who have a headache that does not respond to typical treatment methods, such as resting and taking OTC pain relievers, may want to consider discussing other treatment options with their doctor. A variety of medical treatments and lifestyle changes can help people manage their symptoms and prevent headaches in the future.
Do you suffer headaches needlessly?
This means that there are lots of people needlessly suffering headache pain, says Lipton, professor of neurology, epidemiology, and social medicine at Albert Einstein College of Medicine in New York. "We see patients who have suffered for years and years," he says.
Can nothing help your headaches?
When faced with patients who say nothing helps their headaches, they say: Keep trying. "Even for the most difficult-to-treat patients, 90% -- and up -- are very substantially better after a period of good specialty care," researcher Richard B. Lipton, MD, tells WebMD.
Should I go to the ER for a headache?
Remember, an ER doctor isn’t a headache specialist. Their focus will be to rule out serious health issues that cause head pain, like meningitis or a stroke. They may suggest some imaging tests, such as a CT scan that takes a picture of the inside of your head.

When should you report a headache?
See a GP if: your headache keeps coming back. painkillers do not help and your headache gets worse. you have a bad throbbing pain at the front or side of your head – it could be a migraine or, more rarely, a cluster headache. you feel sick, vomit and find light or noise painful.
Can a person have a migraine headache without any history of having them?
Silent migraines vary in how much they impact day-to-day life. Some people may experience them rarely, in short duration, and with few symptoms. Others experience them daily with severe symptoms. Since silent migraines don't cause pain, you may experience aura symptoms without realizing you're having a migraine.
What happens if you dont treat a headache?
If left untreated, your headache pain will become moderate to severe. Pain can shift from one side of your head to the other, or it can affect the front of your head, the back of your head or feel like it's affecting your whole head.
What kind of headache do you get with COVID?
It is presenting mostly as a whole-head, severe-pressure pain. It's different than migraine, which by definition is unilateral throbbing with sensitivity to light or sound, or nausea. COVID headaches present more as a whole-head pressure.
Are silent migraines serious?
Silent migraines can impact a person's quality of life, especially if they are severe or occur frequently. Even though silent migraines do not cause pain, the other symptoms may be debilitating. Medications and lifestyle changes can help manage symptoms.
What does a silent migraine look like?
Silent migraine symptoms Moderate to severe aura symptoms, such as noticing strange smells, having numbness or tingling in the arms and neck, trouble hearing, weakness in arms, and loss of speech. Sensitivity to bright lights and/or loud noises. Sensitivity to particular smells. Nausea and vomiting.
What are the 4 types of headaches?
There are several hundred types of headaches, but there are four very common types: sinus, tension, migraine, and cluster. Headaches are always classified as either primary or secondary.
Can migraine leads to death?
Migraine headaches are unlikely to cause death or brain damage directly. However, there may be an increased risk of cardiovascular events with migraine and an increased risk of stroke in people who have migraine with aura.
When should you go to the hospital for a headache?
If the sudden onset of a headache prevents you from performing daily tasks, is significantly debilitating, or is accompanied by the following symptoms, you should seek emergency treatment near you: Difficulty walking. Fever. Neurological symptoms including weakness, numbing, slurred speech and blurred vision.
Are headaches a symptom of long COVID?
Long COVID headaches may be more frequent in those patients who have a history of headaches. COVID can also cause a new persistent headache that has not been experienced prior to your COVID illness, but which lasts for some time afterwards, and can be felt on a daily basis.
Is headache a post Covid symptoms?
Patients commonly report headaches as a symptom following COVID-19. There are many types, with different symptoms and locations. Most headaches are not dangerous nor cause damage to the brain. There are medication and non-medication options that often help.
How do you get rid of a headache from COVID?
Some medications that may relieve the symptoms include :ibuprofen (Advil)naproxen (Aleve)aspirin.acetaminophen (Tylenol)combination headache medications, such as those containing aspirin, caffeine, and acetaminophen.
How to treat migraine headaches?
If you have serious headache pain due to a chronic condition like migraine, your doctor might recommend prescription drugs to help prevent or reduce migraine pain. If you have high blood pressure, take medication as prescribed to help lower it. Follow a low-sodium diet to keep your blood pressure from spiking.
How many types of headaches are there?
There are 36 different types of common headaches. However, sometimes headache pain is a sign that something is wrong. Read on to learn the signs and symptoms that will help you know when to worry about a headache.
What does it mean when you have headaches in the third trimester?
Headaches in the third trimester of pregnancy can be a symptom of preeclampsia. This health complication causes high blood pressure. It can lead to liver and kidney damage, brain injury, and other serious problems. Preeclampsia usually begins after week 20 of pregnancy.
What causes pain in the head?
muscle or joint pain. pain that begins after coughing, sneezing, or any type of exertion. constant pain in the same area of your head. seizures. night sweats. unexplained weight loss. tenderness or a painful area on your head. swelling on your face or head.
What are the symptoms of preeclampsia?
symptoms of preeclampsia. Get urgent medical treatment if you are pregnant and have symptoms such as: headache. stomach pain.
What are the symptoms of a concussion?
Get immediate medical help if you have symptoms of a concussion after a fall or a blow to the head. These include: headache. dizziness.
How to know if you have heatstroke?
If you overheat in warm weather or during excess exercise, you may have heatstroke. If you suspect heatstroke, move into the shade or an air-conditioned space. Cool down by drinking cool water, putting on wet clothes, or getting into cool water. Look for these warning signs of heatstroke: headache. dizziness.
What percentage of people with cluster headaches have facial pain?
Among participants with cluster headaches, 15 percent had facial pain; of them, 31 percent had pain mostly in the face. Those with rare forms of headaches also had facial pain. In fact, 45 percent of the 20 people with paroxysmal hemicrania (severe attacks on one side of the head) experienced facial pain. Facial pain impacted 21 percent of the 42 ...
Why does my face hurt when I have a headache?
Yury Khelemsky, an interventional pain specialist focusing on head and neck pain at the Icahn School of Medicine at Mount Sinai in New York, said facial pain is often a result of sensitization of nerves that occurs in people with headaches. It can be caused by trigeminal neuralgia, a condition impacting nerves in the face.
How long does facial pain last?
The researchers noted six people with constant facial pain on one side of the head and attacks lasting 10 to 30 minutes several times a day. This syndrome has been observed before and is called constant unilateral facial pain with added attacks.
Can you have a headache without a headache?
People can have headaches without having pain in the skull, and only experience facial pain. Most often, facial pain triggers headaches. As such, treating it can relieve both ailments. There’s no specific type of headache that makes facial pain seem worse, he added.
Is facial pain a headache?
Facial pain isn’t well recognized as a headache symptom. Some people with it may think it’s something else and wind up waiting longer for proper diagnosis and treatment, said Dr. Arne May, a neurology professor at the University of Hamburg in Germany.
Do cluster headaches cause facial pain?
People with cluster headaches were more likely to have facial pain compared to people with migraine . Having a headache may not all be in your head. A new study in the journal Neurology finds that up to 10 percent of people with headaches also experience facial pain.
Does the upper part of the spine cause headaches?
The upper part of the spine can affect the head and face, or act as a trigger for facial pain and headaches. People are not aware that a lot of head and face pain actually indicate an issue in the neck. “Treating headache and facial pain without addressing the underlying neck issues often misses the mark,” Khelemsky said.
When do headaches return?
The symptoms vary from person to person, but they usually follow the same pattern as the preexisting primary headache. Rebound headaches usually develop in the morning, after waking. Although pain relievers can reduce headache pain, the relief is temporary. It often returns once the medication wears off.
How long does a headache last?
Headache pain can range from mild to severe and may last for several hours. Although resting and taking over-the-counter (OTC) ...
How often do rebound headaches occur?
Rebound headaches tend to occur on a recurring basis. The International Headache Society (IHS) describe a rebound headache as one that occurs on 15 or more days per month in people with a preexisting primary headache disorder and a history of medication overuse.
What does it mean when your headache is red?
a headache accompanied by neck stiffness. a migraine headache that has persisted for several days. the onset of new symptoms, such as vision loss, confusion, or fever. The American Migraine Foundation provide guidelines on headache “red flags,” which indicate when a person should see a doctor.
What is a cervicogenic headache?
Cervicogenic headaches are secondary headaches that result from structural problems in the head, neck, and spine. These structural issues may be due to: Typically, people with cervicogenic headaches experience pain that begins in the neck and back of the head and spreads to the front of the head.
What is the best medication for migraines?
prescription migraine medications, such as triptans, ergotamine, beta-blockers, or calcitonin gene-related peptide antagonists. Botulinum toxin, or Botox, injections offer a safe and effective treatment for people who have chronic migraine headaches that do not respond to traditional medication.
What are the symptoms of migraines?
Other symptoms of migraine include: sensitivity to light and sound. nausea and vomiting. fatigue.
What to do if you have a headache?
If you continue to experience chronic headache pain, your doctor may be able to help. Make an appointment to speak with them about preventative medicines. Ask your healthcare provider alternative treatment options for headaches and migraines , like antidepressants for headaches caused by chronic tension.
Why do headaches last so long?
There are many reasons why a headache can last a while, from hormonal changes to more serious underlying conditions. While it can be alarming for a headache to last a long time — so long that you may not be able to sleep it off — most headaches aren’t life threatening. But it’s no fun when a lingering headache affects your ability to do ...
How long can you take pain medicine?
You shouldn’t take medicine for pain for more than 15 days out of every month, and prescription pain medications shouldn’t be used for more than 10 days out of every month. Your doctor or pharmacist can guide you regarding medication ingredients and potential side effects.
How long does it take for a headache to start?
They start with a feeling of general illness that takes hold one or two days before the headache begins. Some people experience aura, or bright, flashing vision changes, before the pain begins. Then, there’s the headache itself, with symptoms that may include: throbbing pain on either side (or both sides) of your head.
How long does a migraine last?
a migraine that has lasted several days, or even weeks. any new symptoms you haven’t previously experienced along with the headache (disorientation, loss of vision or vision changes, fatigue, or fever) kidney, heart, or liver disease with a headache.
How to stop headaches from a syringe?
You may be able to prevent persistent headaches before they begin by taking a few steps every day. These include: 1 drinking plenty of water to avoid dehydration 2 exercising regularly 3 avoiding environmental triggers 4 getting needed support for your mental health 5 seeking hormonal support, particularly if you’re premenopausal or experiencing menopause 6 reducing stress
What causes a headache during pregnancy?
kidney, heart, or liver disease with a headache. a severe or ongoing headache in pregnancy, which could indicate complications like preeclampsia. HIV or another immune system disorder along with a headache.
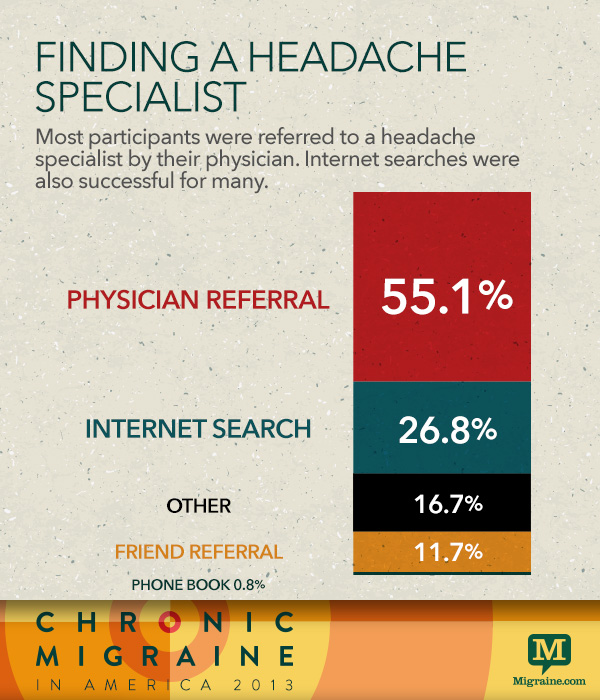
What kind of doctor can help with headaches?
Your primary care doctor is a good starting point, but headaches are complex. Neurologists and headache specialists have special training to help them figure out the type of headache you have and its causes. They can come up with a treatment plan to manage your symptoms.
How to get rid of headaches?
Stick to a sleep schedule. Too little or too much rest can trigger headaches. Get to a healthy weight. A high body mass index (BMI) can lead to more migraines. Track your headaches. Write down when you get one and what you were doing right before. Make sure to include what, if anything, helped ease your pain.
How to stop migraines?
Small tweaks in your daily routine can lower the number of headaches or migraines you have: 1 Drink plenty of water. 2 Don’t skip meals. 3 Watch your caffeine intake. 4 Limit alcohol. 5 Manage other health problems. Conditions like anxiety or high blood pressure can trigger headaches if you don’t keep them under control. 6 Watch your use of medicines. Taking OTC pain relievers too often, or at a higher dose than advised, could cause more problems. Once the drug wears off, withdrawal symptoms start. This leads to more head pain and the need for more medicine. Doctors call this a rebound headache. 7 Stick to a sleep schedule. Too little or too much rest can trigger headaches. 8 Get to a healthy weight. A high body mass index (BMI) can lead to more migraines. 9 Track your headaches. Write down when you get one and what you were doing right before. Make sure to include what, if anything, helped ease your pain.
How to treat cluster headaches?
Immediate treatment: Some drugs can put a quick end to a headache or migraine. Your doctor might have you inhale oxygen through a mask to relieve cluster headaches. Doctors might refer to this type of treatment as abortive therapy. Ibuprofen or naproxen may relieve migraines or tension headaches.
Can you get headaches after another?
If you get one headache or migraine after another and over-the-counter (OTC) pain relief doesn’t help, you do have options. Headaches are tricky. Most of the time, there isn’t a single cause. They result from many different things going on inside and around you.
Does a headache go away?
Your headaches are severe or come on quickly. Your headache never fully goes away. You take pain relievers more than twice a week. You take a higher dose of medicine than what’s advised on the label. Actions like bending over, coughing, sneezing, or having sex bring on a headache or migraine.
Can triptans help migraines?
But, for more severe migraines, prescription triptans are often recommended. Preventive treatment: Prescription drugs can stop pain before it starts. It can make what you do feel less severe. Nondrug treatments: Many natural therapies can be useful, too. Your headache specialist may suggest:
Popular Posts:
- 1. westly chapel family practic patient portal
- 2. benifis health patient portal
- 3. bayless behavioral health
- 4. garrison women's patient portal
- 5. monadnocj hospital patient portal login
- 6. gregory mann patient portal
- 7. mcwhc patient portal
- 8. patient portal piedmont medical center
- 9. dr brenda barry patient portal
- 10. monument avenue pediatrics patient portal