SOAP Report Format - Official Miami Dade College Homepage
6 hours ago · The Subjective section of your soap note is about what the patient is experiencing and how they are handling their concerns. Some common examples may include chest pain, decreased appetite, and shortness of breath. You can also talk to a family member or spouse to get any necessary information. >> Go To The Portal
In many facilities, the major problem or problems that have brought the patient to you for treatment are stated prior to actually beginning the SOAP Note itself. This is usually stated as the Problem or Diagnosis. The Problem part of the note can be stated as the patient's chief concern.
Full Answer
How do you List A patient’s complaint on a SOAP note?
See what their Chief Complaint (CC) is and list that at the top of your SOAP note. The CC will help other medical professionals see what the patient’s condition is so they know what to expect from the rest of the note.
How to document a patient assessment (soap)?
How to Document a Patient Assessment (SOAP) 1 Subjective. The subjective section of your documentation should include how... 2 Objective. This section needs to include your objective observations,... 3 Assessment. The assessment section is where you write your thoughts on the salient issues and... 4 Plan. The final section is the plan,...
What are soap report skills and why do you need them?
Strong SOAP report skills can help you communicate accurately and concisely with a healthcare professional so they can decide the best possible way to provide treatment while considering many other patients. Like any other skill taught on wilderness medicine courses, giving a SOAP note needs to be practiced.
Can soap improve documentation in acute surgical receiving?
A quality improvement project using a problem based post take ward round proforma based on the SOAP acronym to improve documentation in acute surgical receiving. Ann Med Surg (Lond).
What should be included in a SOAP note assessment?
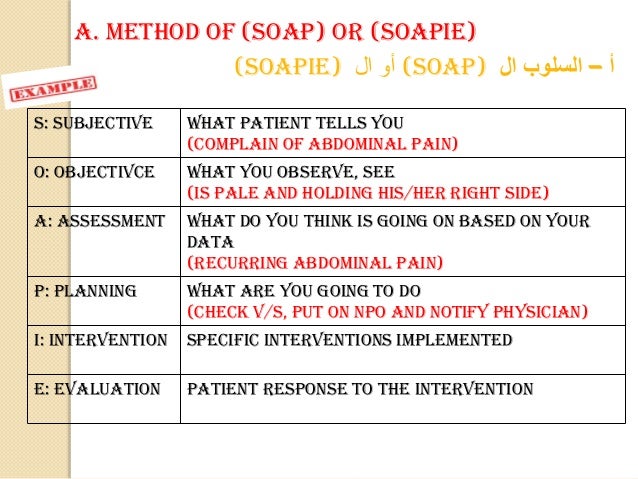
SOAP notes include a statement about relevant client behaviors or status (Subjective), observable, quantifiable, and measurable data (Objective), analysis of the information given by the client (Assessment), and an outline of the next course of action (Planning).
How do you write a follow up SOAP note?
Document what the patient tells you. The subjective section refers to what the patient tells you. ... Document your observations of patient vital signs. This next section concerns observations made by the clinician. ... Document your assessment results. ... Document your treatment plan.
How do you write a good soap report?
Tips for Effective SOAP NotesFind the appropriate time to write SOAP notes.Maintain a professional voice.Avoid overly wordy phrasing.Avoid biased overly positive or negative phrasing.Be specific and concise.Avoid overly subjective statement without evidence.Avoid pronoun confusion.Be accurate but nonjudgmental.
How do you document patient general appearance?
AppearanceAge: Does the patient appear to be his stated age, or does he look older or younger?Physical condition: Does he look healthy? ... Dress: Is he dressed appropriately for the season? ... Personal hygiene: Is he clean and well groomed, or unshaven and unkempt, with dirty skin, hair or nails?More items...•
How do you write a good mental health progress note?
Mental Health Progress Notes Templates. ... Don't Rely on Subjective Statements. ... Avoid Excessive Detail. ... Know When to Include or Exclude Information. ... Don't Forget to Include Client Strengths. ... Save Paper, Time, and Hassle by Documenting Electronically.
How do you write a progress note for a client?
Progress Notes entries must be:Objective - Consider the facts, having in mind how it will affect the Care Plan of the client involved. ... Concise - Use fewer words to convey the message.Relevant - Get to the point quickly.Well written - Sentence structure, spelling, and legible handwriting is important.
What are 3 guidelines to follow when writing SOAP notes?
However, all SOAP notes should include Subjective, Objective, Assessment, and Plan sections, hence the acronym SOAP.
What is the O in SOAP notes?
The O can stand for either “objective” or “observations.” This section of the note covers objective data that you observe during the examination or...
How do you write a good SOAP note?
A good SOAP note should be concise, professional in tone, and specific. Avoid anything that sounds judgmental or overly positive or negative toward...
Who uses SOAP notes?
A variety of healthcare professionals use SOAP notes to help them assess their patients. This can include doctors, counselors, physical therapists,...
The Basics
Subjective
- This component of your SOAP note includes information about the event/injury provided by the patient or bystanders, what you see that gives you a sense of the situation, and the summary/story of what happened.
Objective
- The second component of your SOAP Note includes objective findings and observations of the patient’s current state. Make note of the position you found your patient in, or that you were in, following the MOI. Then, provide details about pertinent findings, or pertinent negatives, found during your patient exam.
Assessment
- The third component of your SOAP report is the assessment, which is where you convey the problem listto the healthcare professional. By using your wilderness medicine education you to associate signs/symptoms to possible ailments, you can deduce your patient’s most pressing issues.
Plan
- This is where you outline your beginning treatment plan. You should convey to the caretaker on the phone what treatment you’ve begun taking, as well as possible steps you plan to take. While your wilderness medicine training gives you the tools to create an educated treatment plan, be sure to follow whatever steps the emergency responders on the phone recommend. This will be …
Final Thoughts
- The COVID-19 pandemic has no boundaries, so now’s the time to assess how to transition your wilderness medicine skills from the backcountry to the frontcountryso you can provide much needed support for our medical services. Strong SOAP report skills can help you communicate accurately and concisely with a healthcare professional so they can decide the best possible wa…