Nursing Care Plan for: Ineffective Breathing Pattern, …
19 hours ago Nursing Care Plan for Dyspnea 5. Dyspnea Nursing Diagnosis: Activity intolerance related to imbalance between oxygen supply and demand as evidenced by fatigue, overwhelming lack of energy, verbalization of tiredness, generalized weakness, and shortness of breath upon exertion. Desired Outcome: The patient will demonstration active participation ... >> Go To The Portal
Patient will identify/demonstrate behaviors to achieve airway clearance. Patient will display/maintain a patent airway with breath sounds clearing; absence of dyspnea, cyanosis, as evidenced by keeping a patent airway and effectively clearing secretions. Nursing Assessment and Rationales
Full Answer
What does it mean when a nurse reports dyspnea to a doctor?
c. When you report a patient’s dyspnea rating to the physician responsible for the patient, the physician orders an intervention to relieve dyspnea (pharmacologic or non-pharmacologic). Nurses’ perception of physician response.
How can nurses provide feedback on dyspnea and pain assessment?
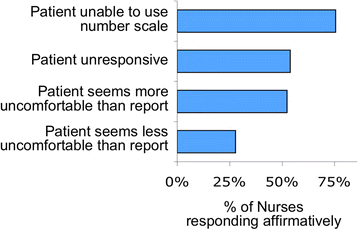
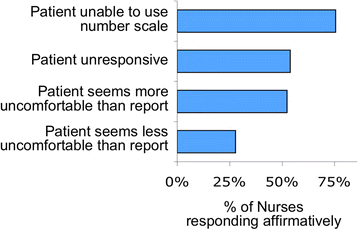
We obtained feedback from nurses using a three-part assessment of practice: 1) a series of recorded focus group interviews with nurses, 2) a time-motion observation of nurses performing routine dyspnea and pain assessment, and 3) a randomized, anonymous on-line survey based, in part, on issues raised in focus groups. Results
How important is routine dyspnea assessment in improving patient centered care?
A strong majority of nurses responded that routine assessment of dyspnea is ‘important’ or ‘very important’ in improving patient centered care (78%) (Fig. 4, Additional file 9: Figures S6; Additional file 10: Figure S7; Additional file 11: Figure S8; Additional file 12: Figure S9; Additional file 13: Figure S10; Additional file 14: Figure S11).
Should nurses use the 0–10 scale for rating dyspnea?
Many nurses feel that rating dyspnea using the 0–10 scale is easy for alert and oriented patients; in some cases, they reported in the focus groups that “rating of dyspnea was easier than rating pain” and “it’s easier for them to understand than the pain scale. ” One nurse explained that she could rely on patients’ self-rating of their dyspnea:
What is the nursing care plan for dyspnea?
Nursing Care Plan for Dyspnea 1 Assess and record respirations, including the rate and depth at least every 4 hours. Auscultate breath sounds at least every 4 hours. To detect adventitious or abnormal breath sounds that may need immediate management. Assist in patient positioning for maximum breathing.
What are some nursing diagnosis for shortness of breath?
Shortness of Breath Nursing Care Plan 5 Nursing Diagnosis: Fatigue related to labored breathing, respiratory distress, and hypoxia, secondary to pneumonia, as evidenced by dyspnea, increased pulse rate, increased respiratory rate, and restlessness.
How do you assess for dyspnea?
Initial Assessment of Patients with Dyspnea Assess airway patency and listen to the lungs. Observe breathing pattern, including use of accessory muscles. Monitor cardiac rhythm. Measure vital signs and pulse oximetry.
What would be the best expected outcome for the nursing diagnosis ineffective breathing pattern?
Desired Outcome: The patient will achieve effective breathing pattern as evidenced by respiratory rates between 12 to 20 breaths per minutes, oxygen saturation between 88 to 92%, and verbalize ease of breathing. Assess the patient's vital signs and characteristics of respirations at least every 4 hours.
Is dyspnea the same as shortness of breath?
Shortness of breath — known medically as dyspnea — is often described as an intense tightening in the chest, air hunger, difficulty breathing, breathlessness or a feeling of suffocation.
How do you write a nursing care plan?
To create a plan of care, nurses should follow the nursing process: Assessment. Diagnosis. Outcomes/Planning....Assess the patient. ... Identify and list nursing diagnoses. ... Set goals for (and ideally with) the patient. ... Implement nursing interventions. ... Evaluate progress and change the care plan as needed.
What are the signs and symptoms of dyspnea?
What are the symptoms of dyspnea?heart palpitations.weight loss.crackling in the lungs.wheezing.night sweats.swollen feet and ankles.labored breathing when lying flat.high fever.More items...
What is dyspnoea?
Sudden shortness of breath, or breathing difficulty (dyspnoea), is the most common reason for visiting a hospital accident and emergency department.
What is a dyspnea scale?
A dyspnea scale is a way to describe shortness of breath you feel during exercise. The scale may be used during exercise at pulmonary rehabilitation or at home.
How do you write a nursing diagnosis?
A nursing diagnosis has typically three components: (1) the problem and its definition, (2) the etiology, and (3) the defining characteristics or risk factors (for risk diagnosis). BUILDING BLOCKS OF A DIAGNOSTIC STATEMENT. Components of an NDx may include problem, etiology, risk factors, and defining characteristics.
What is the nursing diagnosis for respiratory distress?
The diagnosis of ARDS is made based on the following criteria: acute onset, bilateral lung infiltrates on chest radiography of a non-cardiac origin, and a PaO/FiO ratio of less than 300 mmHg.
Is dyspnea a symptom of asthma?
Dyspnea is a symptom of asthma. Environmental pollutants such as chemicals, fumes, dust, and smoke can make it more difficult for people with dyspnea to breathe. People with asthma may find that exposure to allergens such as pollen or mold may trigger episodes of dyspnea.
How often should you record your respiratory rate?
Assess and record respiratory rate and depth at least every 4 hours. The average rate of respiration for adults is 10 to 20 breaths per minute. It is important to take action when there is an alteration in the pattern of breathing to detect early signs of respiratory compromise.
Why is continuous assessment necessary?
Continuous assessment is necessary in order to know possible problems that may have lead to Ineffective Breathing Pattern as well as name any concerns that may occur during nursing care.
What is Cheyne Stokes respiration?
Cheyne-Stokes respiration signifies bilateral dysfunction in the deep cerebral or diencephalon related with brain injury or metabolic abnormalities. Apneusis and ataxic breathing are related with failure of the respiratory centers in the pons and medulla. Rates and Depths of Respiration. Apnea.
What is respiratory failure?
Respiratory failure may be correlated with variations in respiratory rate, abdominal, and thoracic pattern.
How many breaths per minute is Cheyne Stokes?
Respirations fall below 12 breaths per minute depending on the age of patient. Cheyne-Stokes respiration. Progressively deeper and sometimes faster breathing, followed by a gradual decrease that results in apnea. The pattern repeats, with each cycle usually taking 30 seconds to 2 minutes.
Can anxiety cause shortness of breath?
Sometimes anxiety can cause dyspnea, so watch the patient for “air hunger” which is a sign that the cause of shortness of breath is physical. Assess for use of accessory muscle. Work of breathing increases greatly as lung compliance decreases. Monitor for diaphragmatic muscle fatigue or weakness (paradoxical motion).
What is ineffective airway clearance?
Ineffective Airway Clearance is a common NANDA nursing diagnosis for pneumonia nursing care plans. This diagnosis is related to excessive secretions and ineffective cough or nonproductive coughing. Inflammation and increased secretions in pneumonia make it difficult to maintain a patent airway.
What happens if you leave pneumonia untreated?
If left untreated, pneumonia could complicate to hypoxemia, respiratory failure, pleural effusion, empyema, lung abscess, and bacteremia. Nursing care plan (NCP) and care management for patients with pneumonia start with an assessment of the patient’ medical history, performing respiratory assessment every four (4) hours, physical examination, ...
What are the two types of pneumonia?
Types of Pneumonia. There are two types of pneumonia: community-acquired pneumonia (CAP), or hospital-acquired pneumonia (HAP) or also known as nosocomial pneumonia. Pneumonia may also be classified depending on its location and radiologic appearance.
What Is a Nursing Care Plan?
A nursing care plan documents the process of identifying a patient’s needs and facilitating holistic care, typically according to a five-step framework. A care plan ensures collaboration among nurses, patients, and other healthcare providers. 1 2 3 4
What Are the Components of a Care Plan?
Care plans are structured as a five-step framework: assessment, diagnosis, outcomes and planning, implementation, and evaluation. 4
Care Plan Fundamentals
In a simple but useful way, Nurse.org explains the core questions your care plan should answer: what, why, and how. 9 A nursing care plan should include:
Sample Nursing Care Plan
Despite the overall general objective, nursing care plans written by students are not the same as those created by registered nurses in clinical settings. The student version is much longer, has a greater level of detail, and is exhaustively thorough.
Wrapping Up: Writing an Effective Nursing Care Plan
To be successful, a nursing plan needs effective communication, goal-oriented tasks, accessibility and shareability, and evidence-based practice.
Definition of Pneumonia
Pneumonia is an acute inflammation of the lung parenchyma (alveolar spaces and interstitial tissue) caused by bacteria and viruses. After inflammation lung tissue becomes oedematous and its space fill with exudate, gas exchange cannot occur and non-oxygenated blood is entered into the vascular system cause hypoxia.
Impaired Gas Exchange
Collection of mucus in airway inflammation of airways and alveoli fluid-filled alveoli.
Risk for Infection
Inadequate primary defences. (decreased ciliary action, stasis of body fluids)
How to treat dyspnoea?
The distress caused by dyspnoea can be alleviated by pharmacological interventions, the most common being oxygen therapy and inhaled bronchodilators. Oxygen therapy - This is used to treat hypoxia (a low level of arterial oxygen).
What causes dyspnoea?
Acute causes of dyspnoea include asthma, myocardial infarction and pulmonary embolism. Dyspnoea may also be associated with chronic illness; for example, chronic obstructive pulmonary disease, lung cancer, heart failure and obesity. Acute and chronic dyspnoea can lead to life-threatening situations.
What does it mean when you feel breathlessness?
This is derived from the Greek word, which, when translated, means ‘difficulty in breathing’ . Patients describe dyspnoea in a number of ways; for example: ‘Like suffocating’; Tightening feeling of fear in your chest and mind’;
What is a thorough nursing assessment?
A thorough nursing assessment and measurement of systemic observations allows the nurse to gain an understanding of how patients are managing their breathlessness. Their smoking history. The information obtained from the assessment will inform the patient’s nursing care plan.
What is breathlessness?
Breathlessness is a subjective experience, which has been described as an unpleasant or uncomfortable awareness of breathing, or of the need to breathe (Gift, 1990). This article has been updated. The evidence in this article is no longer current. Click here to see an updated and expanded article.
Why is breathing through your nose uncomfortable?
Breathing through the mouth at an increased respiratory rate can result in a drying effect on the oral mucous membranes , and can be very uncomfortable. Fluids should be encouraged, along with regular mouth care.
How to reduce respiratory effort?
For some patients, a more tactile approach, with gentle rubbing of the back and stroking of an arm, can sometimes help to relax them, thus reducing the respiratory effort. Some people, however, do not find this approach helpful, therefore it is important to discuss tactile approaches with them.
Introduction
COPD is a chronic disease that affects the lungs and airways. It causes problems with breathing, making it difficult to do activities like work or exercise. The diagnosis of COPD can be challenging because symptoms come on slowly over time and are often mistaken for other conditions such as asthma, bronchitis, or pneumonia.
What is COPD?
COPD, which stands for chronic obstructive pulmonary disease, is a progressive lung disease that makes it difficult to breathe. The medical definition of COPD includes chronic bronchitis and emphysema.
What Causes COPD?
Most of the time, COPD is caused by tobacco smoking (cigarette smoking). For some people, COPD runs in their families. It’s also common among people who work in dusty jobs, such as farming, construction, or manufacturing.
What Does A Good Nursing Diagnosis for COPD Entail?
To diagnose COPD in a patient, many symptoms must be present over an extended period. These include chronic cough, sputum production, shortness of breath on exertion or rest, wheezing on breathing out when lying down flat (respiratory rate > 25\bpm), and an abnormal chest x-ray or pulmonary function test.
What Are the Interventions for These Nursing diagnoses?
Nursing interventions for activity intolerance include: Providing the patient with information about their disease. This helps them to understand what they are going through and how to manage their condition better. Another intervention is providing opportunities for exercise as much as possible, especially when patients have no symptoms.
Nursing Diagnosis Impaired Gas Exchange
This may be related to the disease or other factors such as respiratory muscle fatigue, movement of mucus in airways, use of medications that are potent bronchodilators, or have adverse side effects. Minimal symptoms necessitate minimal intervention, but when present, they include:
What is a Nursing Care Plan?
A nursing care plan is a document that provides an outline for planning the interventions necessary to meet the goals of care. These plans are often written by a registered nurse (RN) or other qualified healthcare professionals.
Signs and Symptoms
Goals and Outcomes
- The following are the common goals and expected outcomes. 1. Patient maintains an effective breathing pattern, as evidenced by relaxed breathing at normal rate and depth and absence of dyspnea. 2. Patient’s respiratory rate remains within established limits. 3. Patient’s ABG levels return to and remain within established limits. 4. Patient indicate...
Nursing Assessment and Rationales
- Continuous assessment is necessary to know possible problems that may have led to Ineffective Breathing Patternand name any concerns during nursing care. 1. Assess and record respiratory rate and depth at least every 4 hours. The average rate of respiration for adults is 10 to 20 breaths per minute. It is important to take action when there is an alteration in breathing patterns to dete…
Nursing Interventions and Rationales
- The following are the therapeutic nursing interventions for ineffective breathing patterns: 1. Place patient with proper body alignment for maximum breathing pattern. A sitting position permits maximum lung excursion and chest expansion. 2. Encourage sustained deep breaths. Techniques include (1) using demonstration: highlighting slow inhalation, holding end inspiration for a few s…
Recommended Resources
- Recommended nursing diagnosis and nursing care plan books and resources. Disclosure: Included below are affiliate links from Amazon at no additional cost from you. We may earn a small commission from your purchase. For more information, check out our privacy policy. 1. Nursing Care Plans: Nursing Diagnosis and Intervention (10th Edition) An awesome book to hel…
See Also
- Other recommended site resources for this nursing care plan: 1. Nursing Care Plans (NCP): Ultimate Guide and Database Over 150+ nursing care plans for different diseases and conditions. Includes our easy-to-follow guide on how to create nursing care plans from scratch. 2. Nursing Diagnosis Guide and List: All You Need to Know to Master Diagnosing Our comprehensive guid…
References and Sources
- Recommended sources, interesting articles, and references about Ineffective Breathing Pattern to further your reading. 1. Amorim Beltrão, B., da Silva, V. M., de Araujo, T. L., & de Oliveira Lopes, M. V. (2011). Clinical indicators of ineffective breathing pattern in children with congenital heart diseases. International Journal of Nursing Terminologies and Classifications, 22(1), 4-12. 2. Cav…
Popular Posts:
- 1. advancedmd patient portal scheduling
- 2. rapid city regional, patient portal
- 3. jackson hospital patient portal
- 4. sierra nevada medical group patient portal
- 5. patient care report of a code
- 6. mhg patient portal
- 7. sand lake imaging patient portal start now
- 8. mercy health portal patient
- 9. advent health.com patient portal
- 10. https://www.bannerhealth.com/patients/mybanner-patient-portal