National Patient Safety Goals | The Joint Commission
6 hours ago Strategy 3: Nurse Bedside Shift Report. Research shows that when patients are engaged in their health care, it can lead to measurable improvements in safety and quality. To promote stronger engagement, Agency for Healthcare Research and Quality developed the Guide to Patient and Family Engagement in Hospital Quality and Safety, a tested, evidence-based resource to help … >> Go To The Portal
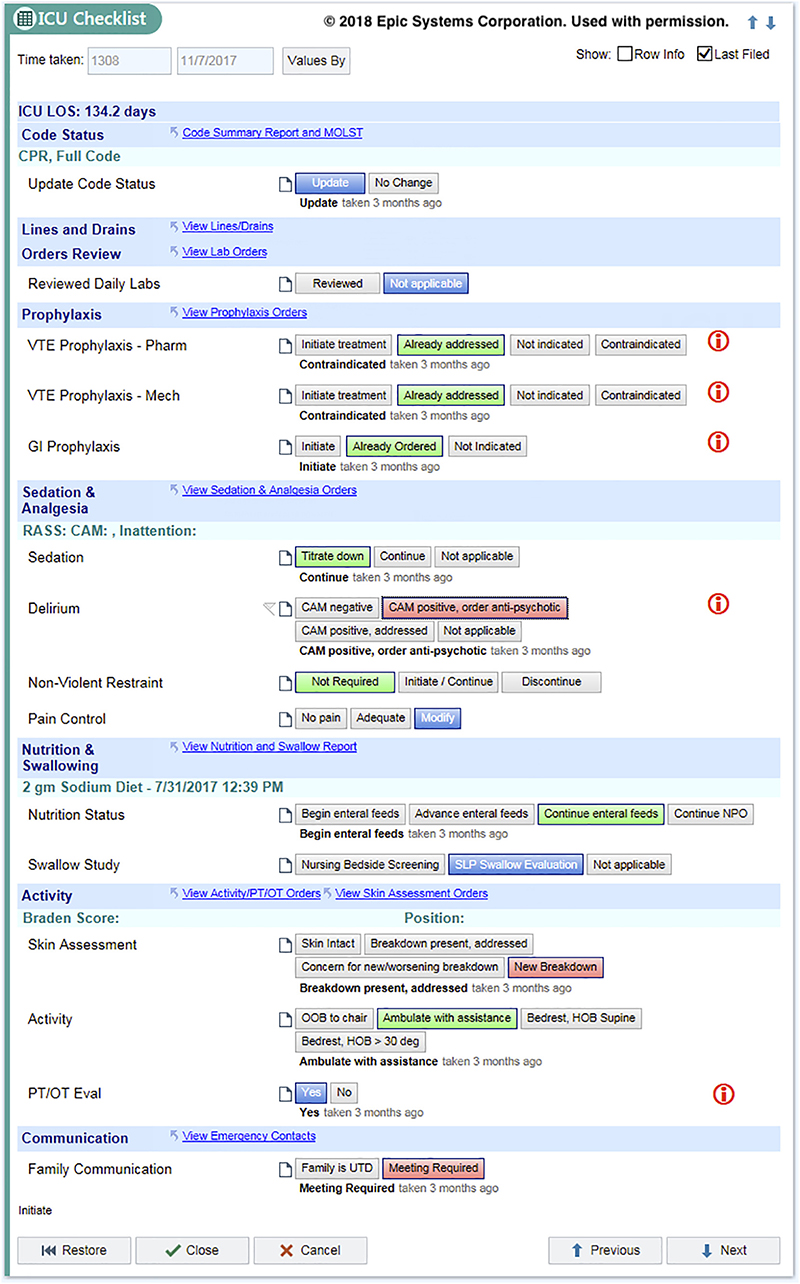
The goal of a bedside report is to improve in the continuity of care, support the exchange of relevant patient information, and promote patient safety (Bigani & Correia, 2018). According to a study conducted by AHRQ, nearly 53% healthcare providers state
Full Answer
Where can I find more information about national patient safety goals?
© 2021, The Joint Commission ⎻The National Patient Safety Goals for each program and more information are available on The Joint Commission website at www.jointcommission.org ⎻Questions can be sent to the Standards Interpretation Group at 630-792-5900 or via the Standards Online Question Form
What is the goal of the nurse bedside shift report?
Strategy 3 states: “The goal of the Nurse Bedside Shift Report strategy is to help ensure the safe handoff of care between nurses by involving the patient and family. The patient defines who their family is and who can take part in bedside shift report.” 7
How do you write a bedside report on a patient?
It should start outside of the patient's room covering the general information history what's occurred, then kind of go through a head‐to‐toe assessment of what's going on. Then you go into the room and you can finish the bedside report at the bed, looking at all of the things that you might have noted.
Who is the registered trademark of national patient safety goals?
Standards Online Question Form (National Patient Safety Goals is a registered trademark of The Joint Commission) For more information… Title PowerPoint Presentation Author Amanda Cohen Created Date 2/9/2021 1:32:21 PM

Does bedside reporting increased patient safety?
Research has shown that the implementation of bedside report has increased patient safety and patient and nurse satisfaction. An evidence-based practice change incorporating bedside report into standard nursing care was implemented and evaluated over a four-month time period on three nursing units.
What are the five National Patient Safety Goals?
This is done to make sure that each patient gets the correct medicine and treatment.Identify patients correctly.Prevent infection.Improve staff communication.Identify patient safety risks.Prevent mistakes in surgery.
What are recent examples of National Patient Safety Goals?
The Joint Commission has outlined seven patient safety goals for hospitals to focus on in 2021, including:Identify patients correctly. ... Improve staff communication. ... Use medicines safely. ... Use alarms safely. ... Prevent infection. ... Identify patient safety risks. ... Prevent mistakes in surgery.
What are the 2021 National Patient Safety Goals?
The Joint Commission's 2021 national patient safety goals for hospitals are:Improve the accuracy of patient identification.Improve staff communication.Improve the safety of medication administration.Reduce patient harm associated with clinical alarm systems.Reduce the risk of healthcare-associated infections.More items...•
How are National Patient Safety Goals determined?
Development of the Goals Following a solicitation of input from practitioners, provider organizations, purchasers, consumer groups, and other stakeholders, The Joint Commission determines the highest priority patient safety issues and how best to address them.
What are some good safety goals?
Other possible safety goals may include:Active participation in safety committees.Complete job safety analysis in each department before every major task.Perform weekly inspections.Create a plan to eliminate a particular hazard to the lowest level.Develop a written system to document and investigate accidents.More items...
What is the most important National Patient Safety Goal?
Goal 1: Improve the Accuracy of Patient Identification To address this issue, patient safety goals require the use of at least two patient identifiers when providing care, such as patient name and patient date of birth.
How often are NPSGs reviewed?
Is reviewed and if the facility meets the criteria, then it will receive an accreditation, which is renewable every three years. promote specific improvement in patient safety. NPSGs are important to the delivery of safe, high quality health care.
Which example qualifies as a sentinel event?
Examples of sentinel events from the Joint Commission include the following: Suicide during treatment or within 72 hours of discharge. Unanticipated death during care of an infant. Abduction while receiving care.
Why are the National Patient Safety Goals important?
The purpose of the National Patient Safety Goals is to improve patient safety. The goals focus on problems in health care safety and how to solve them. This is an easy-to-read document. It has been created for the public.
How many Ipsg are there?
The six International Patient Safety Goals are: Goal 1 - Identify Patients Correctly. Goal 2 - Improve Effective Communication. Goal 3 - Improve the safety of high-Alert Medications. Goal 4 - Ensure correct Site, Correct Procedure, Correct Patient Surgery.
What is the rationale for National Patient Safety Goal 6?
accurate patient medication information. Goal 6: Reduce patient harm associated with clinical alarm systems.
What is standardized approach to bedside handoff and walking rounds?
Based on recommendations from the Joint Commission, the Robert Wood Johnson Foundation, and broader research literature, a standardized approach to bedside handoff and walking rounds was implemented on an inpatient surgical oncology unit.
What is the purpose of a standardized handoff?
In 2009, the Joint Commission identified a standardized approach to handoff communication as a patient safety goal to reduce communication errors. Evidence suggests that a structured handoff report, combined with active patient participation, reduces communication errors and promotes patient safety. Research shows that bedside handoff increases ...
Why are nurses always on the same page during the report?
Nurses are always on the same page during the report because they're both looking at the same information at the same time. 12. The patient benefits from BSR too.
How many people died from BSR in 2010?
According to the Inspector General Office, Health and Human Services Department, less-than-competent hospital care contributed to the deaths of 180,000 Medicare patients in 2010. However, the real number may be higher: According to one estimate, between 210,000 and 440,000 patients who go to ...
How does BSR work?
How (and why) BSR works. By definition, BSR is the change-of-shift report between the offgoing nurse and the oncoming nurse that takes place at the bedside. This makes patients a part of the process in the delivery of their care.
How does BSR help nurses?
The advantages for the nurse begin with the efficiency of report, which streamlines all pertinent information and saves nursing time. BSR improves staff's teamwork by giving nurses the opportunity to work together at the bedside, ensuring accountability. Using a standardized format reduces the risk of miscommunication because it overcomes different communication styles. Better communication also helps the oncoming nurse prioritize assignments according to need. The nurse is informed about the patient earlier in the shift because report time is shortened. Nurses are always on the same page during the report because they're both looking at the same information at the same time. 12
Why is BSR important in nursing?
Because nurses are the first line of defense when it comes to patient safety, BSR is an integral part of the care plan. The nurse is accountable for the communication that occurs during the change-of-shift report.
How many breaths per minute did the nurse take in 1920?
When two nurses entered her room at 1920 for the BSR, her respiratory rate had dropped to 6 breaths/minute. One nurse stayed in the room while the other obtained and administered naloxone as per protocol. The patient quickly recovered without complications.
Why is standardized format important for nurses?
Using a standardized format reduces the risk of miscommunication because it overcomes different communication styles. Better communication also helps the oncoming nurse prioritize assignments according to need. The nurse is informed about the patient earlier in the shift because report time is shortened.
What is labeling medication in perioperative settings?
In perioperative and other procedural settings both on and off the sterile field, label medications and ✪solutions that are not immediately administered . This applies even if there is only one medication being used.
Why do we mark the site of surgery?
Site marking is done to prevent errors when there is more than one possible location for a procedure. Examples include different limbs, fingers and toes, lesions, level of the spine, and organs. In cases where bilateral structures are removed (such as tonsils or ovaries) the site does not need to be marked.
What is the Universal Protocol?
The Universal Protocol applies to all surgical and nonsurgical invasive procedures. Evidence indicates that procedures that place the patient at the most risk include those that involve general anesthesia or deep sedation, although other procedures may also affect patient safety. Hospitals can enhance safety by correctly identifying the patient, the appropriate procedure, and the correct site of the procedure.
What is clinical alarm system?
Clinical alarm systems are intended to alert caregivers of potential patient problems, but if they are not properly managed, they can compromise patient safety. This is a multifaceted problem. In some situations, individual alarm signals are difficult to detect. At the same time, many patient care areas have numerous alarm signals and the resulting noise and displayed information tends to desensitize staff and cause them to miss or ignore alarm signals or even disable them. Other issues associated with effective clinical alarm system management include too many devices with alarms, default settings that are not at an actionable level, and alarm limits that are too narrow. These issues vary greatly among hospitals and even within different units in a single hospital.
What is critical result?
Critical results of tests and diagnostic procedures fall significantly outside the normal range and may indicate a life-threatening situation. The objective is to provide the responsible licensed caregiver these results within an established time frame so that the patient can be promptly treated.
What is wrong patient error?
The intent for this goal is two-fold: first, to reliably identify the individual as the person for whom the service or treatment is intended; second, to match the service or treatment to that individual. Acceptable identifiers may be the individual’s name, an assigned identification number, telephone number, or other person-specific identifier.
Do hospitals have to verify procedures?
Hospitals should always make sure that any procedure is what the patient needs and is performed on the right person. The frequency and scope of the verification process will depend on the type and complexity of the procedure.
What is the role of a nurse in a change of shift?
The nurse notifies the physician and obtains correct and complete medication orders, thereby avoiding a potentially serious medication error. A nursing unit schedules staffing coverage to accommodate the shift change and minimize the occurrence of interruptions during change-of-shift report.
What is the basic to quality health care?
Basic to the provision of quality health care is the ability to communicate with one another and safely handoff patient care in a seamless manner so every patient can benefit from each phase of care through a well-executed handoff. This is a process that is ubiquitous but also a high-risk endeavor in many settings.
What does Nurse Green realize about morphine sulfate?
When Nurse Brown asks about this, Nurse Green realizes she gave morphine sulfate but did not document it on the MAR. Due to Nurse Brown’s question, Nurse Green realizes the omission and communicates the information and documents it in the medical record , preventing an accidental overdose of a medication.
Popular Posts:
- 1. nash obgy patient portal
- 2. fill in the patient care report medicak
- 3. valant patient portal michelle hauser
- 4. central georgia heart center patient portal
- 5. wheaton franciscan milwaukee patient portal
- 6. fossil creek family medical patient portal
- 7. texas incology patient portal
- 8. northwestern memorial physicians group patient portal
- 9. uma patient portal
- 10. colmar mri patient portal