How to Read a Diabetes Lab Report | ADW Diabetes
19 hours ago · If you live with diabetes, you are probably familiar with getting poked and prodded for blood constantly. But more than just testing one’s blood sugar, people with diabetes require regular laboratory tests to monitor everything from one’s hba1c to Vitamin D levels (people with diabetes tend to run low), to even the amount of protein in one’s urine. This article will outline the most important regular lab tests that people with … >> Go To The Portal
Home glucose testing should be done by the patient to monitor diabetes values regularly. Abnormalities should be reported to the doctor as needed. If blood sugar numbers are under 70 mg/dl or over 200mg/dl for 2 consecutive days, report values to your doctor.
| Result* | A1C Test | Glucose Tolerance Test |
|---|---|---|
| Diabetes | 6.5% or above | 200 mg/dL or above |
| Prediabetes | 5.7 – 6.4% | 140 – 199 mg/dL |
| Normal | Below 5.7% | 140 mg/dL or below |
How to read a diabetes lab report?
How to Read a Diabetes Lab Report. People with diabetes should see their main doctor, whether it be an internist, primary care physician or endocrinologist to obtain their 3-month blood work. Most ordered blood work is routine information for the physician, but it may be meaningless to you.
What do lab tests tell you about diabetes?
Laboratory tests are done to keep track of your health and refine your diabetes self-management plan. These tests are used to determine your blood sugar control, cardiovascular well-being, and kidney function. No matter what type of lab test you are reading, all the reports have some standard features.
What should a nurse assess a patient with diabetes mellitus?
The nurse should assess the following for patients with Diabetes Mellitus: Assess the patient’s history. Assess physical condition. Assess the body mass index and visual acuity of the patient. Perform examination of foot, skin, nervous system and mouth. Laboratory examinations.
What is the test guide for diabetes?
This test guide discusses the use and interpretation of laboratory tests for diagnosing diabetes and monitoring glycemic control. This Test Guide discusses the use of laboratory tests ( Table 1) for diagnosing diabetes mellitus and monitoring glycemic control in individuals with diabetes.
How do you know if you have diabetic neuropathy?
Pain, numbness and tingling are common symptoms. Diagnosis is based on your individual symptoms coupled with a physical exam. If you have diabetes type 2, yearly foot examinations are a must for you.
What percentage of diabetics have nephropathy?
Diabetes And Nephrology. It is estimated that about 50% of patients with insulin-dependent diabetes mellitus develop diabetic nephropathy – a general term that means deteriorating functioning of the kidneys. Genetic factors have been suggested as risk markers for development of nephropathy in diabetes.
What is neuropathy in diabetes?
Diabetes Neuropathy, a nerve disorder, can be of three types – sensory neuropathy, motor neuropathy or autonomic neuropathy . Over time, people with uncontrolled diabetes may develop damage to the nerves around the body, though incidents are also higher in diabetics who are overweight, have high blood pressure, and those who are over the age of 50. The longer you live with diabetes, the greater your risk of developing neuropathies.
What does it mean when your blood glucose is higher than 70?
Blood glucose levels lower than 70 mg/dL indicate hypoglycemia and require immediate attention. Maintain a glucose test results chart to keep track of your blood sugar levels.
What is the normal HBA1C level for type 2 diabetes?
In adults with type 2 diabetes, it’s a good idea to test HbA1c levels at: If you are managing your diabetes type 2 through diet and lifestyle, or through a combination of both, along with a drug that doesn’t lead to hypoglycemia, aim for HbA1c level of 48 mmol/mol (6.5%). If you are on diabetes drugs associated with hypoglycemia, ...
What age do you need to be to get a diabetes test?
Depending on your health, age and medical history, you may require other screening tests. If you are over the age of 60 and have been living with diabetes type 2 for a while, you may also need additional screening for mental health problems, gum diseases and cancer.
Should diabetics have a glucose test kit?
Every Diabetes Type 2 patient should have easy access to a blood glucose testing kit and must strive to get educated about how to make use of the results. This is true even for patients with type 2 diabetes who are on non-insulin diabetes treatments.
What type of diabetes do you have to have to get blood sugar tested?
You’ll need to get your blood sugar tested to find out for sure if you have prediabetes or type 1, type 2, or gestational diabetes. Testing is simple, and results are usually available quickly.
What does it mean when your doctor says you have type 1 diabetes?
If your doctor thinks you have type 1 diabetes, your blood may also tested for autoantibodies (substances that indicate your body is attacking itself) that are often present in type 1 diabetes but not in type 2 diabetes. You may have your urine tested for ketones (produced when your body burns fat for energy), which also indicate type 1 diabetes ...
How much glucose should I drink to test my blood sugar?
You’ll drink a liquid that contains glucose, and then 1 hour later your blood will be drawn to check your blood sugar level. A normal result is 140 mg/dL or lower. If your level is higher than 140 mg/dL, you’ll need to take a glucose tolerance test.
How long does it take to get blood sugar checked?
Then you’ll drink the liquid and have your blood sugar level checked 1 hour, 2 hours, and possibly 3 hours afterward. At 2 hours, a blood sugar level of 140 mg/dL or lower is considered normal, ...
How early can you test for gestational diabetes?
Gestational diabetes is diagnosed using blood tests. You’ll probably be tested between 24 and 28 weeks of pregnancy. If your risk is higher for getting gestational diabetes (due to having more risk factors), your doctor may test you earlier. Blood sugar that’s higher than normal early in your pregnancy may indicate you have type 1 ...
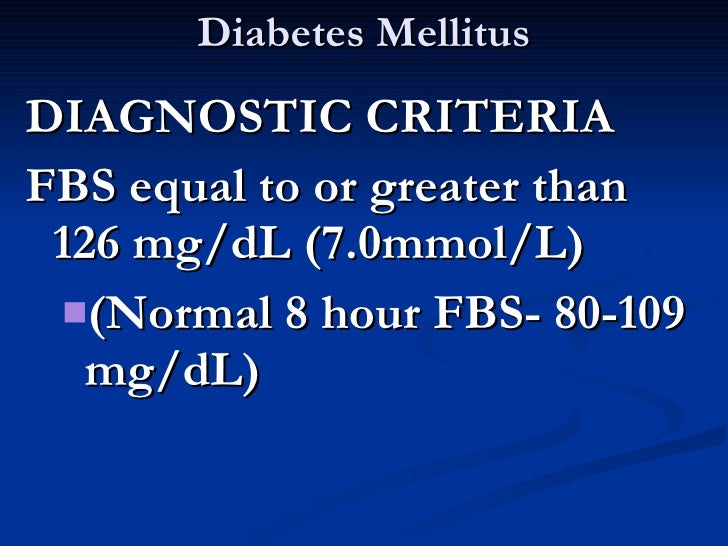
What is the normal blood sugar level after fasting?
This measures your blood sugar after an overnight fast (not eating). A fasting blood sugar level of 99 mg/dL or lower is normal, 100 to 125 mg/dL indicates you have prediabetes, and 126 mg/dL or higher indicates you have diabetes.
What is the normal A1C level?
A1C Test. The A1C test measures your average blood sugar level over the past 2 or 3 months. An A1C below 5.7% is normal, between 5.7 and 6.4% indicates you have prediabetes, and 6.5% or higher indicates you have diabetes.
What is the role of the laboratory in diabetes?
The laboratory has an essential role in the diagnosis and management of diabetes mellitus. The laboratory indicators for the diagnosis and management of diabetes are listed in Table 3:
What is the simplest indicator of the adequacy of carbohydrate metabolism of a patient?
The simplest indicator of the adequacy of carbohydrate metabolism of a patient is the blood glucose concentration. However glucose is rapidly metabolized in the body. Therefore, the glucose concentration reflects the immediate status of carbohydrate metabolism, and does not allow a retrospective or prospective evaluation of glucose metabolism.
How do proteins react with glucose?
Proteins react spontaneously in blood with glucose to form glycated derivatives. This reaction occurs slowly under physiological conditions and without the involvement of enzymes. The extent of glycation of proteins is controlled by the concentration of glucose in blood and by the number of reactive amino groups present in the protein that are accessible to glucose for reaction. All proteins with reactive sites can be glycated and the concentration of the glycated proteins that can be measured in blood is a marker for the fluctuation of blood glucose concentrations during a certain period. From a clinical diagnostic point glycated proteins with a longer life time in blood are of interest, since they reflect the exposure of these proteins to glucose for longer periods
What is the OGTT test?
The OGTT is a provocation test to examine the efficiency of the body to metabolise glucose. The OGTT provides information on latent diabetes states. The OGTT distinguishes metabolically healthy individuals from people with impaired glucose tolerance and those with diabetes. The OGTT is more sensitive than FPG for the diagnosis of diabetes. Nevertheless the final diagnosis of diabetes should not be based on a single 2 h post-load glucose >11,1 mmol/L (>2,00 g/L) but should be confirmed in subsequent days (FPG and/or casual glucose estimation).
How many people will have diabetes by 2025?
The mean percentage prevalence varies between ethnic groups (American Indians, Hispanics, and others). Between 1995 and 2025 there is predicted to be a 35 % increase in the world-wide prevalence of diabetes. The rising number of people with diabetes will occur mainly in populations of developing countries, leading to more than 300 million people with diabetes globally by 2025. Presently as many as 50 % of people with diabetes are undiagnosed. Since therapeutic intervention can reduce complications of the disease, there is a need to detect diabetes early in its course. The risk of developing Type 2 diabetes increases with age, obesity, and lack of physical activity.
What is diabetes mellitus?
Diabetes mellitus is a group of diseases characterized by an elevated blood glucose level (hyperglycaemia) resulting from defects in insulin secretion, in insulin action, or both. Diabetes mellitus is not a pathogenic entity but a group of aetiologically different metabolic defects. Common symptoms of diabetes are lethargy from marked hyperglycaemia, polyuria, polydipsia, weight loss, blurred vision and susceptibility to certain infections. Severe hyperglycaemia may lead to hyperosmolar syndrome and insulin deficiency to life-threatening ketoacidosis. Chronic hyperglycaemia causes long-term damage, dysfunction and failures of various cells, tissues and organs. Long-term complications of diabetes are:
Can a diabetic maintain blood glucose levels?
Individuals with diabetes should maintain blood glucose levels as close to normal as is safely possible. People with Type 1 diabetes (and others using insulin therapy) can only achieve this goal by self-monitoring of blood glucose.
What is the pathophysiology of diabetes mellitus?
Pathophysiology of Diabetes Mellitus Type 2. Type 2 diabetes mellitus has major problems of insulin resistance and impaired insulin secretion. Insulin could not bind with the special receptors so insulin becomes less effective at stimulating glucose uptake and at regulating the glucose release.
Why is the classification system of diabetes mellitus unique?
The classification system of diabetes mellitus is unique because research findings suggest many differences among individuals within each category, and patients can even move from one category to another, except for patients with type 1 diabetes.
What happens if you leave diabetes mellitus untreated?
If diabetes mellitus is left untreated, several complications may arise from the disease. Hypoglycemia. Hypoglycemia occurs when the blood glucose falls to less than 50 to 60 mg/dL because of too much insulin or oral hypoglycemic agents, too little food, or excessive physical activity. Diabetic Ketoacidosis.
How to lower blood glucose levels?
Exercise. Exercise lowers blood glucose levels by increasing the uptake of glucose by body muscles and by improving insulin utilization. A person with diabetes should exercise at the same time and for the same amount each day or regularly. A slow, gradual increase in the exercise period is encouraged.
What is the cause of diabetes mellitus?
Type 1 diabetes mellitus is characterized by destruction of the pancreatic beta cel ls. A common underlying factor in the development of type 1 diabetes is a genetic susceptibility. Destruction of beta cells leads to a decrease in insulin production, unchecked glucose production by the liver and fasting hyperglycemia.
Why is insulin needed in type 1 diabetes?
In type 1 diabetes, exogenous insulin must be administered for life because the body loses the ability to produce insulin. Insulin in type 2 diabetes. In type 2 diabetes, insulin may be necessary on a long-term basis to control glucose levels if meal planning and oral agents are ineffective.
How many people will have diabetes by 2030?
By 2030, the number of cases is expected to increase more than 30 million . Diabetes is especially prevalent in the elderly; 50% of people older than 65 years old have some degree of glucose intolerance. People who are 65 years and older account for 40% of people with diabetes.
Case Presentation
A.B. is a retired 69-year-old man with a 5-year history of type 2 diabetes. Although he was diagnosed in 1997, he had symptoms indicating hyperglycemia for 2 years before diagnosis.
Discussion
A.B. presented with uncontrolled type 2 diabetes and a complex set of comorbidities, all of which needed treatment. The first task of the NP who provided his care was to select the most pressing health care issues and prioritize his medical care to address them. Although A.B.
Summary
Advanced practice nurses are ideally suited to play an integral role in the education and medical management of people with diabetes. 15 The combination of clinical skills and expertise in teaching and counseling enhances the delivery of care in a manner that is both cost-reducing and effective.
Popular Posts:
- 1. patient portal pueblo radiology
- 2. patient portal eorh and ovmc
- 3. patient portal mvhs
- 4. dr rathert patient portal
- 5. lake health district patient portal
- 6. can you see blood type on patient portal
- 7. tgen patient portal
- 8. patient portal dr. zelfand
- 9. labcop patient login
- 10. can medical clinics in texas report patient controlled substance n