Using Patient Portals to Improve Patient Outcomes: …
34 hours ago · Most of the portal interventions used tailored alerts or educational resources tailored to the patient’s condition. Patient portal interventions lead to improvements in a wide range of psychobehavioral outcomes, such as health knowledge, self-efficacy, decision making, medication adherence, and preventive service use. >> Go To The Portal
Patient portal interventions lead to improvements in a wide range of psychobehavioral outcomes, such as health knowledge, self-efficacy, decision making, medication adherence, and preventive service use. Effects of patient portal interventions on clinical outcomes including blood pressure, glucose, cholesterol, and weight loss were mixed.
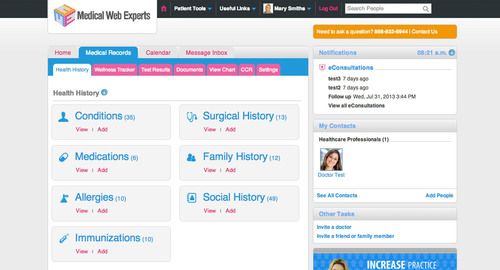
What is a patient portal?
A patient portal is a secure online application that provides patients access to their personal health information and 2-way electronic communication with their care provider using a computer or a mobile device.29Numerous studies30-32have shown that patient portals improve outcomes of preventive care and disease awareness and self-management.
What are the benefits of the care portal?
The care team is now able to keep in contact with patients more reliably and ask them direct questions when needed. Using the portal has enabled the organization to be more transparent and interactive with patients, and to proactively send patients the information they need.
How does patient portal implementation improve quality of patient care?
Patient Portal Implementation Improves Quality of Patient Care and Strengthens Preventive Care Spring 2011 Dover, Delaware About Dover Family Physicians Dover Family Physicians adopted an electronic health record (EHR) system in 2008 with a goal of improving the quality of patient care and especially strengthening preventive care services.
What are the benefits of Technology in healthcare?
Opening Up Better Lines Of Communication Between Patients And Clinicians Technology allows patients and providers to communicate more quickly and clearly.
How does patient portal improve patient care?
Better Patient-Physician Relationships Patient portals provide the ability for patients to have 24-hour access to connect with their provider by reviewing patient health information (PHI), asking and answering questions, and reviewing notes, making the patient-physician relationship closer than ever.Dec 8, 2017
How has technology improved patient care outcomes?
We conclude that health information technology improves patient's safety by reducing medication errors, reducing adverse drug reactions, and improving compliance to practice guidelines. There should be no doubt that health information technology is an important tool for improving healthcare quality and safety.
How do patient portals contribute to patient centered care?
Further, portals help providers educate their patients and prepare them for future care encounters. When patients have access to their health data, they are better informed, and have the potential to generate deep and meaningful conversations regarding patient wellness during doctor's appointments.May 13, 2016
How has technology improved safety in healthcare?
Technological innovations can enhance patient safety by automating tasks, introducing medication alerts, clinical reminders, improved diagnostic and consultation reports, facilitating information sharing, improving clinical decision-making, intercepting potential errors, reducing variation in practice, and managing ...Dec 9, 2020
How does technology improve nursing care?
How Does Technology Affect Nursing?Monitoring. Portable monitors give nurses the freedom to check on patients quickly, even when occupied with other tasks. ... Medications. ... Health Records. ... Beds. ... Reduced Errors. ... Communication. ... Telehealth.
What are the benefits and challenges of using patient portals?
What are the Top Pros and Cons of Adopting Patient Portals?Pro: Better communication with chronically ill patients.Con: Healthcare data security concerns.Pro: More complete and accurate patient information.Con: Difficult patient buy-in.Pro: Increased patient ownership of their own care.Feb 17, 2016
How do patient portals affect nursing?
Takeaways: Patient portals facilitate patient engagement in healthcare decisions, improve communication, and streamline care. Less than one-third of patients access patient portals to view their medical data. Nurses can improve patient portal use by explaining the benefits and providing education.Dec 20, 2021
Do patients like patient portals?
Eight studies reported that patients or their caregivers want more portal education, training, or support. Two studies found that their participants want human connection as they learn about the portal and how to use it, as well as when they encounter issues.Jan 25, 2021
How to get the most value from an EHR?
To get the most value from an EHR, practices will need to invest time in training and preparation. Some customization of the system will likely be needed based on how the practice functions and the individual work styles of the various providers.
When did Dover Family Physicians adopt EHR?
Dover Family Physicians adopted an electronic health record (EHR) system in 2008 with a goal of improving the quality of patient care and especially strengthening preventive care services. The practice has focused on ways to use the EHR to engage patients and their family members in their health and healthcare through a patient portal implementation. The practice, located in Dover, Delaware, has four physicians and two physician assistants, and provides primary care to more than 800 patients weekly.
What are the limitations of EHR?
The limitations of the EHR and the patient portal have presented challenges, such as the inability to send clinical summaries to patients via the portal. The practice can only move ahead with certain aspects of patient and family engagement as quickly as the system is upgraded.
How long does it take for a nurse to respond to a patient?
The practice established standards for response times of within 4 hours for more urgent questions to 2 days for prescription refills
Why is portal important?
The portal has proven to offer a much better means of communication. The care team is now able to keep in contact with patients more reliably and ask them direct questions when needed. Using the portal has enabled the organization to be more transparent and interactive with patients, and to proactively send patients the information they need.
What is the FQHC portal?
The FQHC sees improved communication between patients and providers, and views every instance when a patient emails a provider, nurse, or health coach as an opportunity to take a step towards better health. Patients find the portal to be useful and convenient, as it provides direct access to their health care and information as they need it. The portal supports the organizations philosophy of person-centered and respectful care, and perceives a resulting increase in responsibility and ownership among patients. Now that patients have a greater familiarity and comfort level with technology, the organization is planning to use telemedicine to offer virtual appointments to some patients.
How many no returns per month for a federally qualified health center?
A large Federally Qualified Health Center (FQHC) faced challenges communicating with their patients, resulting in as many as 200 no-returns per month. This loss of contact resulted in lost revenue and wasted staff time, and had the potential to diminish patient health through lack of follow-up.
Why are portals important?
Portals acted as buffers between a patient’s desire for 24-hour access and physicians’ desires for a work-life balance. And while ED visits and hospitalizations are one measure of wellness, it is not clear whether portals improve patient health; to the extent that the foster improved communication, they provide a benefit. ...
How many Medicare beneficiaries use portals?
Portals are not free of problems. Only about 30% of Medicare beneficiaries use them despite nearly 90% of their physicians providing them. As with many healthcare disparities, age, income, and in this instance broadband access, limit portal use.
What is meaningful use?
Meaningful use refers to not just having electronic health records (EHR), but using them in a useful way for patients. And while getting the various EHRs to talk to one another seems not to have been considered meaningful, EHRs have implemented patient portals – a means for patients to e-communicate with their physicians ...
How effective are patient portals?
Patient portal use has also been found to be effective in improving psychological outcomes, such as decision making and self-efficacy, and behavioral outcomes , such as medication adherence and cancer screening. It’s clear that patient portals for healthcare have many positive effects on the patient experience and health outcomes.
Why should healthcare organizations use patient portals?
Healthcare organizations should consider implementing such a solution to provide better care and empower patients to take a larger role in their own health management.
Why do we need a patient portal?
Patient portals help facilitate patient engagement and improve outcomes when fully utilized by patients and care partners. Healthcare providers who use a patient portal solution recognize its ability to engage patients in their care, facilitate stronger patient-provider communication, and increase access to their healthcare information.
Is a portal better for diabetes?
According to a group of researchers from Kaiser Permanente®, those with diabetes who use a patient portal may be better [⁴] off than those who do not. The use of a portal leads to better medication adherence and overall chronic disease management.
1. Easier Access to Doctors
When the pandemic struck, people turned to a technology already in place, but not widely used—telemedicine. Many insurance companies now consider a video consultation as an office visit and patients only have to pay their copay.
2. Better Senior Care
Senior care faces some steep challenges now and in coming years. In the United States, 10,000 baby boomers turn 65 every day. Facilities often find themselves overwhelmed and understaffed.
3. Faster Results
Put yourself in the shoes of a person waiting on results from a scan where they are checking for cancer or to see if they have a particular disease. By utilizing technology, results come back faster and information is distributed more easily between the lab and the doctor’s office or hospital.
4. Fewer Medication Errors
Errors in medication are a big issue in healthcare. The typical person has multiple doctors, including specialists. They may not always be aware of what another provider prescribed. While the pharmacy might catch some mistakes, people sometimes use multiple pharmacies to get the best rates on prescription medications.
5. Predicting Outbreaks
Utilizing data from different areas of the country and tracking numbers allows professionals to tap into AI and figure out where the next big outbreak might be. Hospitals can prepare for a potential surge in patients and make sure they have supplies on hand to treat the most common illness of the moment.
6. Easily Accessible Records
One of the biggest issues with multiple healthcare professionals working with a patient is lack of communication between offices. However, with the popularity of cloud computing, it is much easier for each new healthcare provider to access details on what’s been done before, see test results and know what medications the patient currently takes.
7. Remote Monitoring
Patients can now monitor their own health at home with devices that report to the cloud. Sometimes the device is as simple as a watch that tracks exercise or heart rate. However, there are other devices that are more intensive and can test and send blood sugar levels throughout the day and even alert the patient if numbers go too high or low.
How does information technology improve patient safety?
We conclude that health information technology improves patient’s safety by reducing medication errors, reducing adverse drug reactions, and improving compliance to practice guidelines. There should be no doubt that health information technology is an important tool for improving healthcare quality and safety.
How does electronic medical record help?
There is substantial evidence that implementing an electronic medical record reduces medical errors and improves patient’s safety. Computerized physician order entry and CDS are probably one of the most beneficial health information technologies for improving patient safety.
What is a computerized physician order entry system?
Computerized physician order entry systems are usually integrated with a clinical decision support system (CDS), which acts as an error prevention tool through guiding the prescriber on the preferred drug doses, route, and frequency of administration.
What is clinical decision support?
Clinical decision support. Clinical decision support provides the health care professional with information and patient-specific information. This information is intended to enhance the decision of the healthcare provider and is rationally filtered and presented to the healthcare professional at appropriate times.
What is access to care?
Access to care may be one of the most central questions confronting health-care leaders today. Consumers want convenient, easy access to care; in a survey conducted by my company ( via Healthcare Dive ), 51% of consumers surveyed said convenience and access to care were the most important factor in their decision-making. Their desire for convenience may contribute to the growth of non-traditional care models like telehealth. And providers are finally getting on board; one 2019 survey ( via Healthcare Dive) found that physician adoption increased 340% between 2015 and 2018. In 2015, 5% of providers surveyed used telemedicine, increasing to 22% by the end of 2018. Leading health systems are starting to anticipate the demands of their consumers.
What is AI in healthcare?
Artificial intelligence (AI) is one of the most promising technologies in health-care. For example, providers may be able to use predictive analytics to anticipate what their patients will need instead of merely reacting as new concerns arise.
Is AI good for cancer?
In June 2019, IBM Watson Health announced studies that show progress in the use of AI to improve clinical decision-making and treatment in cancer care. According to one report, machine learning researchers even believe that by 2053, AI could out-perform human surgeons.
