Fisdap Patient Care Report And Soap Narratives
6 hours ago Fisdap Patient Care Report And Soap Narratives SAMPLE BRIEF NARRATIVE REPORT April 28th, 2019 - SAMPLE BRIEF NARRATIVE REPORT August 2 0000 Ms Laura ... April 21st, 2019 - Transcribed Partial Patient Care Report PCR NARRATIVE 74 y o male Pt has Hx of cardiac diabetes morbidly obese Arrived before FD at residence to fine pt >> Go To The Portal
How do you write a patient care report for a narrative?
How to Write an Effective ePCR NarrativeBe concise but detailed. Be descriptive in explaining exactly what happened and include the decision-making process that led to the action. ... Present the facts in clear, objective language. ... Eliminate incorrect grammar and other avoidable mistakes. ... Be consistent and thorough.
How do you make a narrative chart?
CHART narratives also follow a visual layout based on the letters in the acronym. Starting with the chief Complaint, the History of the present illness, along with the patient's past medical history, are outlined. Assessment findings are then documented, along with Rx (prescriptions) that the patient is prescribed.
What is the soap method in EMS?
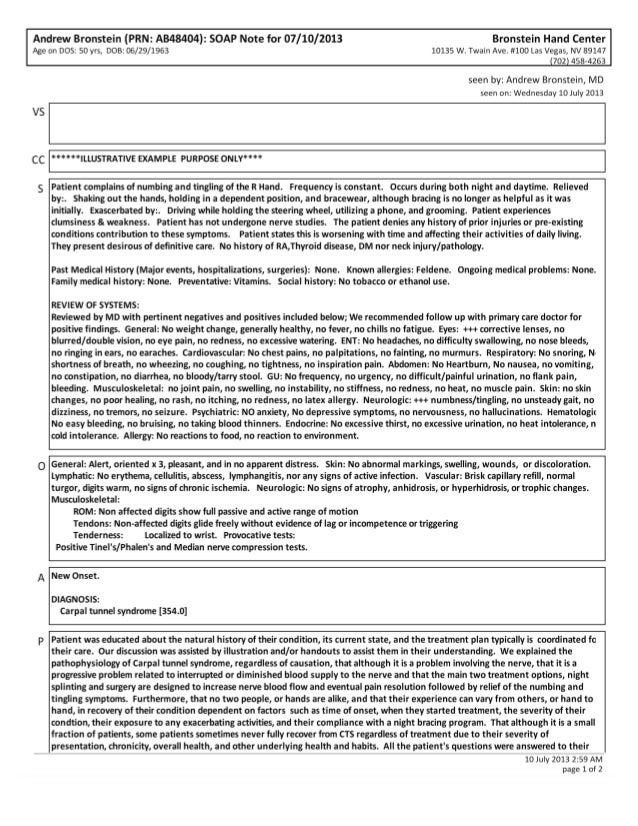
The Subjective, Objective, Assessment and Plan (SOAP) note is an acronym representing a widely used method of documentation for healthcare providers. The SOAP note is a way for healthcare workers to document in a structured and organized way.[1][2][3]
Why should a patient care report be detailed?
Importance of Documentation The purpose of record documentation is to provide an accurate, comprehensive permanent record of each patient's condition and the treatment rendered, as well as serving as a data collection tool.
What is a narrative report?
A narrative essay tells a story. In most cases, this is a story about a personal experience you had. This type of essay, along with the descriptive essay, allows you to get personal and creative, unlike most academic writing.
How do you write a SOAP note in nursing?
0:105:59How to Make SOAP Notes Easy (NCLEX RN Review) - YouTubeYouTubeStart of suggested clipEnd of suggested clipUse the soap note as a documentation method to write out notes in the patient's chart. So stands forMoreUse the soap note as a documentation method to write out notes in the patient's chart. So stands for subjective objective assessment and plan let's take a look at each of the four components.
How do you write a soap narrative?
Tips for Effective SOAP NotesFind the appropriate time to write SOAP notes.Maintain a professional voice.Avoid overly wordy phrasing.Avoid biased overly positive or negative phrasing.Be specific and concise.Avoid overly subjective statement without evidence.Avoid pronoun confusion.Be accurate but nonjudgmental.
How do you write a patient narrative in EMS?
1:3211:38How to Write a Narrative in EMS || DCHART Made Easy ... - YouTubeYouTubeStart of suggested clipEnd of suggested clipSection some people include a lot less some people will just include the reference. And the address.MoreSection some people include a lot less some people will just include the reference. And the address. So next is the chief complaint. And this is pretty self-explanatory.
What are the 4 parts of soap?
The acronym SOAP stands for Subjective, Objective, Assessment, and Plan.
What is the purpose of the narrative section of the patient care report?
Detailed explanation of medical necessity: Your narrative should be detailed and provide a clear explanation for why the patient needed to be transported by ambulance. Include what the medical reasons were that prevented the patient from being transported by any other means.
What should a patient care report include?
What Patient Care Reports Should IncludePresenting medical condition and narrative.Past medical history.Current medications.Clinical signs and mechanism of injury.Presumptive diagnosis and treatments administered.Patient demographics.Dates and time stamps.Signatures of EMS personnel and patient.More items...•
How do you write a good patient care report?
There are seven elements (at a minimum) that we have identified as essential components to documenting a well written and complete narrative.Dispatch & Response Summary. ... Scene Summary. ... HPI/Physical Exam. ... Interventions. ... Status Change. ... Safety Summary. ... Disposition.
What was the Medic 1 response to above location?
(Location): Medic 1 responded to above location on a report of a 62 y.o. male c/o of chest pain. Upon arrival, pt presented sitting in a chair attended by first responder. Pt appeared pale and having difficulty breathing.
Does the patient respond to questions?
Patient does not respond to questions, but crew is informed by family that patient is deaf. Per family, the patient has been "sick" today and after consulting with the patient's doctor, they wish the patient to be transported to HospitalA for treatment.
What Is a Patient Care Report?
We often hear of care reports based on by medical teams or by medical authorities. Yet, we are not sure how this differs from the kind of report that is given to us by the same people. So this is the time to make it as clear as possible.
How to Write a Patient Care Report?
Where do you even begin when you write a patient care report? A lot of EMS or EMTs do know how to write one since they are trained to do so.
What is a patient care report?
A patient care report is a document made mostly by the EMS or EMTs. This documented report is done after getting the call. This consists of the information necessary for the assessment and evaluation of a patient’s care.
What should not be written in a patient care report?
What should be avoided in a patient care report is making up the information that is not true to the patient. This is why you have to be very careful and very meticulous when writing these kinds of reports. Every detail counts.
Who is in charge of reading the patient care report?
The person or the people who will be reading the report are mostly medical authorities. When you are going to be passing this kind of report, make sure that you have all the information correctly. One wrong information can cause a lot of issues and problems.
Popular Posts:
- 1. lowcountry medical group patient portal
- 2. bozeman deaconess health services patient portal
- 3. followmyhealth pih patient portal
- 4. roads merrimack nh patient portal
- 5. st lukes daily patient report of care
- 6. meadville patient portal
- 7. nc mountain medical patient, portal
- 8. southeast ob gyn patient portal
- 9. numc patient portal
- 10. eric marom patient portal