Publication of case reports: Is consent required? - PMC
7 hours ago Some members of the Forum argued that a paper containing identifiable details of a patient cannot be published without consent unless the patient is dead or the patient has given informed consent to publication. In this case, consent cannot be obtained and therefore the presumption should be that the case report should not be published. The Forum advised that the editor should consider not only the ethical and legal issues involved in … >> Go To The Portal
Do patients read consent forms?
They often do not read consent forms carefully because they assume that someone else has scrutinised the risks and benefits on their behalf. Interviews with 103 patients showed that many factors influence a decision to take part in medical research (Hastings Center Report 1996;26 (5):25-9).
Is your medical consent properly informed?
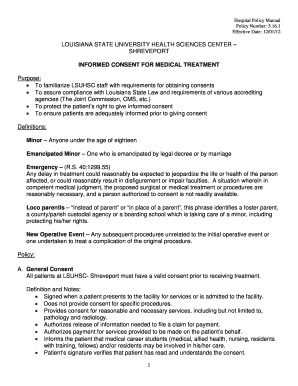
Informed consent to medical treatment is fundamental in both ethics and law. Patients have the right to receive information and ask questions about recommended treatments so that they can make well-considered decisions about care. Successful communication in the patient-physician relationship fosters trust and supports shared decision making.
What is a patient consent?
The physician provided his patient with a dense seven-page consent form, in which specific surgical risks, like tissue necrosis, were mentioned; she signed the consent form. However, the physician did not engage in any detailed discussions with his patient ...
Is informed consent possible?
Informed consent is not only required for clinical trials but is an essential prerequisite before enrolling each and every participant in any type of research involving human subjects including; diagnostic, therapeutic, interventional, bioequivalence, social and behavioral studies and for all research conducted domestically or abroad.
Do case reports require ethical approval?
Case reports and studies intended for quality improvement are often considered not research and do not need IRB approval. Nevertheless, there should be some processes of clearing those studies with respect to ethical handling of patients and related data.
When or in what case it is not necessary for informed consent?
Exceptions to Informed Consent Several exceptions to the requirement for informed consent include (1) the patient is incapacitated, (2) life-threatening emergencies with inadequate time to obtain consent, and (3) voluntary waived consent.
Do case reports require IRB approval?
Under HIPAA, a case report is an activity to develop information to be shared for medical/educational purposes. Although the use of protected health information to prepare the paper does not require IRB review, the author of a case report must comply with HIPAA.
Can you treat a patient without informed consent?
If adult patients are mentally able to make their own decisions, medical care cannot begin unless they give informed consent. The informed consent process makes sure that your health care provider has given you information about your condition along with testing and treatment options before you decide what to do.
When can a patient be treated without consent?
You can only be treated for a physical health problem without your consent if: you lack capacity, or. your physical health problem is a symptom or underlying cause of a mental health problem. In this case, the Mental Health Act says that you can be given treatment against your wishes.
When can you waive informed consent?
Waiver of Documentation of Informed Consent (45 CFR 46.117) A waiver of documentation is permissible when: The signature on the informed consent document would be the only record linking the subject to the research and the principal risk of harm to the subject would be a breach of confidentiality.
Do case studies need informed consent?
Although not technically required, especially if the case report does not include any identifying information, some journals require informed consent for all case reports before publishing. The CARE guidelines recommend obtaining informed consent AND the patient's perspective on the treatment/outcome (if possible).
Are case studies exempt from IRB review?
As a result, case studies generally qualify for exempt review by the IRB provided that the study (a) does not involve a sensitive topic, (b) is conducted in a manner that protects subjects' identity, and (c) does not involve at-risk or special populations.
Does case report count as research?
The case report is a research design where an unexpected or novel occurrence is described in a detailed report of findings, clinical course, and prognosis of an individual patient, which might be, but not mandatory, accompanied by a review of the literature of other reported cases.
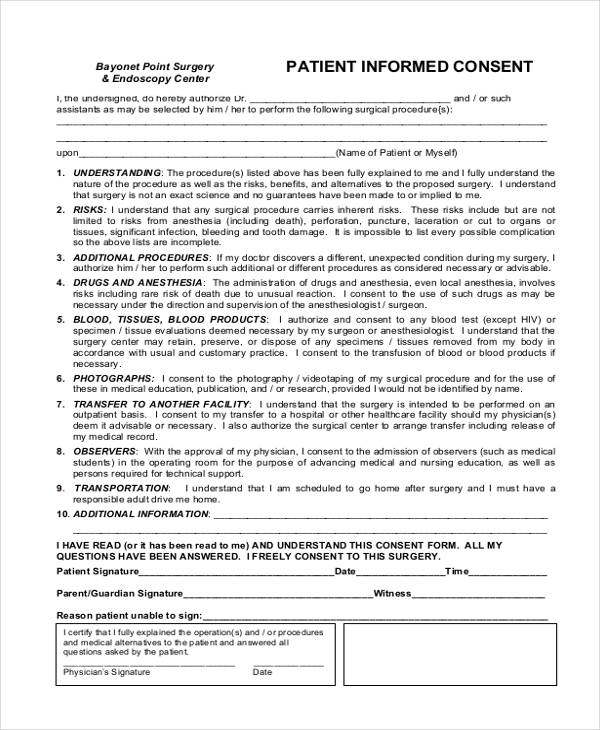
What is non informed consent?
A lack of informed consent refers to a physician or hospital neglecting to provide a patient appropriate information about the risks, benefits and alternatives to a surgery or treatment with medication in a non-emergency setting.
Is lack of informed consent negligence?
In both medical and legal terminology, this is called "informed consent." If a doctor does not get informed consent from a patient, and the patient is injured, the patient may have grounds to sue the doctor for medical malpractice.
Is consent a legal requirement?
Consent forms Written consent is not usually required by law, but is considered good practice. It serves as a record of the information given to the patient, and of the patient's consent. Modern consent forms usually include details of the risks and benefits of the procedure.
What was the case report submitted to journal X?
A case report was submitted to journal X reporting on a child who had been admitted to hospital suffering an injury, which the doctors suspected resulted from a deliberate cigarette burn.
Can a child be identified in a hospital?
It is possible that the child could be identified, because the location of the hospital is given in the authors’ affiliations, the injuries are clearly detailed and the parents have been convicted of child abuse (it is not known if there was any press coverage of this case).
Can a case report be published without consent?
Some members of the Forum argued that a paper containing identifiable details of a patient cannot be published without consent unless the patient is dead or the patient has given informed consent to publication. In this case, consent cannot be obtained and therefore the presumption should be that the case report should not be published. The Forum advised that the editor should consider not only the ethical and legal issues involved in deciding to publish, but also the data protection issues. In terms of whether the pubic health value of publication should overturn considerations of consent and confidentiality, the general consensus of the Forum was that it is unlikely that a single case report is so medically important that it must be published, and that if he or she wishes to use a public interest defence, the editor must be prepared to defend their decision in the event of a complaint by the patient or a regulatory body.
What is required to submit a case report?
Journals often have specific requirements for publishing case reports, which could include a requirement for informed consent, a letter or statement from the IRB and other things.
What should I do after writing a case report?
Once you have written a draft of the case report, you should seek feedback on your writing, from experts in the field if possible, or from those who have written case reports before .
Why is it important to write a case report?
the reason you would go to the trouble of writing one, is that the case is sufficiently unique, rare or interesting such that other medical professionals will learn something from it.
Does CHM have funding for publication?
It is best practice to check the journal's Info for Authors section or Author Center to determine what the cost is to publish. CHM does NOT have funds to support publication costs, so this is an important step if you do not want to pay out of pocket for publishing.
Is it free to publish a case report?
Be aware that it may not be free to publish your case report. Many journals charge publication fees. Of note, many open access journals charge author fees of thousands of dollars. Other journals have smaller page charges (i.e. $60 per page), and still others will publish for free, with an "open access option".
Do you need informed consent for a case report?
Although not technically required, especially if the case report does not include any identifying information, some journals require informed consent for all case reports. The CARE guidelines recommend obtaining informed consent AND the patient's perspective on the treatment/outcome (if possible).
Do journals have informed consent?
Journals may have their own informed consent form that they would like you to use, so please look for this when selecting a journal. Once you've identified the case, selected an appropriate journal (s), and considered informed consent, you can collect the required information to write the case report.
Basic principles
Patient privacy and consent are subject to guidance such as the CARE guidelines and COPE, which cover two key aspects: informed consent and removal of patient identifiers from manuscripts as well as clinical images, figures and datasets.
Did they really consent?
Authors and editors must critically assess whether consent for publication (distinct from consent for treatment) was truly given prior to writing or considering a case report for publication. When the patient is considered particularly vulnerable e.g. from a minority group, a child, a prisoner, having disabilities or diminished mental capacity etc.
What happens when things go wrong?
If a paper was published without appropriate consent and it cannot be obtained retroactively, this is an extremely serious matter and the paper may need to be retracted or withdrawn/removed depending on the sensitivity of the content and publication stage.
Katie Eve
Katie Eve is a Communications Manager in Elsevier’s Global Publishing Development department. She joined Elsevier in 2010 and worked as a Publisher for journals across earth sciences and energy before moving into her communications position in 2017.
Catriona Fennell
Following graduation from the National University of Galway, Ireland, Catriona Fennell joined Elsevier as a Journal Manager in 1999. She later had the opportunity to learn about the intricacies of peer review while supporting and training hundreds of editors during the introduction of Elsevier Editorial System (EES).
Margaret Rees
Margaret Rees has an international reputation of leadership in women's midlife health and is the Executive Director of the European Menopause and Andropause Society. A gynaecologist, she is Editor-in-Chief of Case Reports in Women’s Health and Emeritus Editor of Maturitas.
What is a case report?
A case report is a medical/educational activity that does not meet the DHHS definition of “research”, which is: "a systematic investigation, including research development, testing and evaluation, designed to develop or contribute to generalizable knowledge.".
Does a case report have to be approved by the IRB?
Yes. Under HIPAA, a case report is an activity to develop information to be shared for medical/educational purposes. Although the use of protected health information to prepare the paper does not require IRB review, the author of a case report must comply with HIPAA.
Do journals require an IRB letter?
Background: Many journals now require a letter, or other acknowledgement, from an IRB prior to publication of a case report. Specifically, they wish to know whether IRB approval was obtained or was not required for the described case. The JHM IRBs have adopted a policy to address the following question and answers.
What is a case report?
A case report is an unsystematic clinical observation that states the outcome or response of a single patient to a diagnostic strategy or treatment . Case reports serve to document and share novel cases amongst the medical community for educational purposes.
When case reports describe or discuss unique or rare circumstances, as they often do, it may be difficult or impossible to answer
When case reports describe or discuss unique or rare circumstances, as they often do, it may be difficult or impossible to de-identify those cases such that there is no reasonable expectation that the individuals included can be identified, so patient authorization generally would be required.
When safe harbor de-identification is not possible or the opportunity to identify the patient exists, even after de-ident
When safe harbor de-identification is not possible or the opportunity to identify the patient exists, even after de-identification, the expert determination method for de-identification can be considered. For purposes of de-identification, an expert is defined as: A person with appropriate knowledge of and experience with generally accepted statistical and scientific principles and methods for rendering information not individually identifiable:
Is PHI de-identified under HIPAA?
It is important to understand that determining whether data are de-identified under HIPAA is a more restrictive determination than determining whether private information is individually identifiable under the Common Rule. The HIPAA rule considers PHI as any information that may identify an individual; was created or received by a member of a HIPAA covered entity; and relates to the individual's past, present, or future physical/mental health or condition, health care, or payment for health care. HIPAA recognizes two methods for de-identification of data.
Popular Posts:
- 1. ehr for therapists with patient portal
- 2. anamnestic patient report
- 3. joslin patient portal
- 4. greenbrier valley medical center patient portal
- 5. stern patient portal
- 6. a patient had an appendectomy due to appendicitis. this operative report must be completed when?
- 7. blanchard valley hospital patient portal login
- 8. uf health appointment
- 9. pcinternists.com patient portal
- 10. professional physical therapy patient portal