Asthma Reports and Publications | CDC
34 hours ago · Asthma Facts: CDC’s National Asthma Control Program Grantees pdf icon [PDF – 2.7 MB] This report describes asthma prevalence, healthcare utilization, asthma self-management education, and mortality for the program’s funded grantees (2009-2014) in 34 states, the District of Columbia, and Puerto Rico. Fact Sheet Cdc-pdf pdf icon [PDF – 430 KB] >> Go To The Portal
What are the symptoms of asthma in a case study?
A case study of a patient with Asthma. This is a case of a 25-year old woman with episodic shortness of breath and chest tightness. The physical findings of chest pains, wheezing, heavy coughs, blocked sinuses, breathing difficulties, skin rashes together with presented symptoms is suggestive to Asthma infection.
How is asthma diagnosed?
An asthma diagnosis is based on several factors, including a detailed medical history, a physical exam, your symptoms, and overall health and test results. The first step in diagnosing asthma is talking to your doctor about your symptoms and your health.
What are supportive measures for the treatment of asthma?
Supportive measures include seeking medicalattention, avoiding Asthma triggers, taking medication, and check peak flow meter for a measure of infection.
What is a controlled asthma diagnosis?
The definition of controlled asthma Diagnostic evaluation Obstruction of the respiratory tract is objectively demonstrated with pulmonary function testing. Spirometry is the most important testing technique.
How do you assess a patient with asthma?
Physical examExamine your nose, throat and upper airways.Use a stethoscope to listen to your breathing. Wheezing — high-pitched whistling sounds when you breathe out — is one of the main signs of asthma.Examine your skin for signs of allergic conditions such as eczema and hives.
What is the clinical presentation of asthma?
The clinical manifestations of asthma include recurrent episodes of wheezing, chest tightness, cough and shortness of breath. The symptoms are often worse at night or on waking from sleep. Usually, they resolve spontaneously or with the inhalation of a reliever medication.
What is asthma summary?
Asthma is a condition in which your airways narrow and swell and may produce extra mucus. This can make breathing difficult and trigger coughing, a whistling sound (wheezing) when you breathe out and shortness of breath. For some people, asthma is a minor nuisance.
What are the 3 types of asthma?
Types of asthmaDifficult to control asthma.Severe asthma.Occupational asthma.
What is the physical examination findings of bronchial asthma?
During a physical exam for asthma or allergies, your doctor will look at your ears, nose, throat, eyes, skin, chest and lungs. They may: Listen to your lungs for wheezing or whistling that could mean inflammation. Look in your nose and throat for swelling and drainage that could be caused by allergies.
What are the clinical features of severe asthma?
Severe asthma attacks severe shortness of breath where you experience difficulty speaking. rapid breathing where your chest or ribs visibly have retractions. straining your chest muscles and working hard to breathe. nostrils that flare out, moving rapidly as you breathe.
What are 5 causes of asthma?
Common Asthma TriggersTobacco Smoke.Dust Mites.Outdoor Air Pollution.Pests (e.g., cockroaches, mice)Pets.Mold.Cleaning and Disinfection.Other Triggers.
What are the 4 types of asthma?
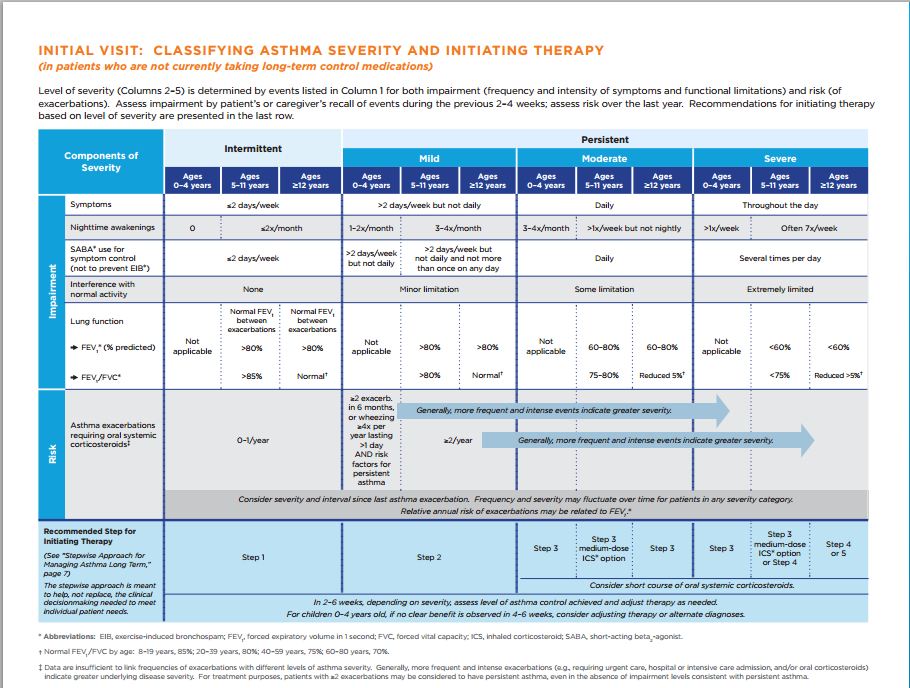
The four main categories of asthma, a chronic respiratory disease that makes it difficult to breathe, are intermittent, mild persistent, moderate persistent, and severe persistent. Asthma is a chronic respiratory disease that causes inflammation and narrowing of the airways, making it difficult to breathe.
How Does asthma affect daily life?
Living with asthma can affect your daily routines and the way in which you manage the daily tasks that we all need to do; getting dressed, having a shower, shopping, cooking and so on. You may notice there are times when you are more, or less, breathless.
What is the best treatment for asthma?
Long-term control medications such as inhaled corticosteroids are the most important medications used to keep asthma under control. These preventive medications treat the airway inflammation that leads to asthma symptoms. Used on a daily basis, these medications can reduce or eliminate asthma flare-ups.
What drink is good for asthma?
Certain herbal teas may help relieve asthma symptoms. Research suggests that ginger tea, green tea, black tea, eucalyptus tea, fennel tea, and licorice tea may reduce inflammation, relax your respiratory muscles, and boost your breathing, among other benefits.
What is serious asthma?
What is severe asthma? Severe asthma is a type of asthma that does not respond well to standard asthma treatments. The symptoms by definition, are more intense than regular asthmatic symptoms and can last for prolonged periods. Sufferers of severe asthma often find their symptoms persistent and difficult to control.
How to test for asthma?
A doctor may use a few different ways of testing for asthma. These include: 1 Taking a detailed medical history 2 A physical exam 3 Lung function tests 4 Chest or sinus X-ray
What are the symptoms of asthma?
Common symptoms are coughing, shortness of breath, wheezing and chest tightness. Asthma may lead to a medical emergency. It is important to know the signs of a severe asthma episode (or asthma attack).
How to manage asthma?
The best way to manage asthma is to avoid triggers, take medications to prevent symptoms and prepare to treat asthma episodes if they occur. AAFA has a lot of information on our site to help you learn more about asthma.
How to prevent asthma attacks?
The best way to prevent an asthma episode, or attack, is to follow your treatment plan. Learn your triggers and avoid them. Take your allergy and asth ma medicines when you should. Use your quick-acting medicine as soon as you start to notice symptoms.
What causes swelling in the airways?
A trigger is something you are sensitive to that makes your airways become inflamed. This causes swelling, mucous production and narrowing in your airways. Common asthma triggers are pollen, chemicals, extreme weather changes, smoke, dust mites, stress and exercise.
How to monitor asthma after diagnosis?
To monitor your asthma after diagnosis. If you know you have asthma, work with your doctor to keep it under control. Good long-term control helps you feel better from day to day and can prevent a life-threatening asthma attack. If your asthma symptoms get worse.
How do you know if you have asthma?
Asthma symptoms vary from person to person. You may have infrequent asthma attacks, have symptoms only at certain times — such as when exercising — or have symptoms all the time. Asthma signs and symptoms include: Shortness of breath. Chest tightness or pain.
How do you know if your asthma is worsening?
Signs that your asthma is probably worsening include: Asthma signs and symptoms that are more frequent and bothersome. Increasing difficulty breathing, as measured with a device used to check how well your lungs are working (peak flow meter) The need to use a quick-relief inhaler more often.
Why does asthma flare up?
For some people, asthma signs and symptoms flare up in certain situations: Exercise-induced asthma, which may be worse when the air is cold and dry. Occupational asthma, triggered by workplace irritants such as chemical fumes, gases or dust.
How to prevent asthma flare ups?
Get vaccinated for influenza and pneumonia. Staying current with vaccinations can prevent flu and pneumonia from triggering asthma flare-ups. Identify and avoid asthma triggers. A number of outdoor allergens and irritants — ranging from pollen and mold to cold air and air pollution — can trigger asthma attacks.
What to do if your asthma doesn't improve?
If your symptoms don't improve, get medical help as directed in your action plan. Take your medication as prescribed. Don't change your medications without first talking to your doctor, even if your asthma seems to be improving. It's a good idea to bring your medications with you to each doctor visit.
What are the complications of asthma?
Asthma complications include: Signs and symptoms that interfere with sleep, work and other activities. Sick days from work or school during asthma flare-ups. A permanent narrowing of the tubes that carry air to and from your lungs (bronchial tubes), which affects how well you can breathe.
What is the CDC's asthma program?
CDC’s National Asthma Control Program works to help Americans with asthma achieve better health and improved quality of life. The program funds states, school programs, and non-government organizations to help them improve surveillance of asthma, train health professionals, educate individuals with asthma and their families, ...
Does the CDC help with asthma?
You must also remove the triggers in your environment that can make your asthma worse. CDC’s National Asthma Control Program works to help Americans with asthma achieve better health and improved quality of life.
How to diagnose asthma in 5 years?
Spirometry. This is the main test doctors generally use to diagnose asthma in people 5 years or older. To help determine how well your lungs are working (pulmonary function), you take a deep breath and forcefully breathe out (exhale) into a tube connected to a spirometer. This records both the amount (volume) of air you exhale ...
What tests are needed for asthma?
If your doctor suspects that you have a condition in addition to or other than asthma, you may need tests such as: X-ray or computerized tomography (CT) imaging of your chest. CT scans of your sinuses. Blood tests. Gastroesophageal reflux assessment.
Why is it so hard to diagnose asthma in children?
It can be especially difficult to diagnose asthma in young children because there are many conditions that cause asthma-like symptoms in this age group. If your child's doctor suspects asthma, the doctor may prescribe a bronchodilator — a drug that opens the airways.
What are the symptoms of asthma in children?
These may include: Louder or faster than normal breathing. Frequent coughing or coughing that worsens after active play. Coughing, clear mucus and a runny nose caused by hay fever. Frequent missed school days.
What are the steps to diagnosing asthma?
Asthma: Steps in testing and diagnosis. Diagnosing asthma generally includes a medical history, physical exam and lung tests. An asthma diagnosis is based on several factors, including a detailed medical history, a physical exam, your symptoms, and overall health and test results.
What does it mean when your lung test is below normal?
If certain measurements are below normal for a person your age, it may indicate that asthma has narrowed your airways. After taking lung test measurements, your doctor may ask you to inhale an asthma drug to open air passages and then do the test again.
What is the name of the device that measures the amount of air you breathe in and out?
Spirometer. Spirometer. A spirometer is a diagnostic device that measures the amount of air you're able to breathe in and out and its rate of flow. Your doctor may use several tests to determine how well your lungs are working.
What are the precipitants of asthma?
Symptoms. Intermittent and variable (may also be absent, e.g., during symptom-free intervals or in mild disease) Shortness of breath (o ften in acute episodes) Expiratory wheezes.
What is the cardinal manifestation of asthma?
The cardinal manifestation of asthma consists of recurrent episodes of shortness of breath of acute onset, typically at night or in the early morning hours . Bronchial asthma afflicts about 10% of children and 5% of adults.
What is bronchial asthma?
Bronchial asthma is a chronic inflammatory disease of the airways characterized by bronchial hyperreactivity and a variable degree of airway obstruction. It is diagnosed on the basis of the clinical history, physical examination, and pulmonary function tests, including reversibility testing and measurement of bronchial reactivity.
What is the most important risk factor for bronchial asthma?
An atopic diathesis, i.e., a genetic predisposition toward the production of IgE antibodies in response to (for example) pollen, house dust mites, fungi, or animal-derived proteins, is the most important risk factor for bronchial asthma.
How often do you have to take bronchodilators for asthma?
No symptoms at night, or no awakening because of asthma. No need for rapidly-acting bronchodilators for symptomatic treatment ("relievers"), or at most two times per week.
Is bronchial asthma a global health problem?
Bronchial asthma is a serious global health problem. 5% to 10% of persons of all ages suffer from this chronic airway disorder. This review article presents important considerations of diagnosis and treatment in view of the current national and international asthma guidelines. Methods.
Can asthma be identified as a non-allergic disease?
In childhood, bronchial asthma is usually due to allergies; on the other hand, in 30% to 50% of adults with asthma, no allergy can be identified, at least not with the standard techniques. Non-allergic asthma in adults can arise, for example, after a viral infection of the lower respiratory tract.
What causes asthma in the office?
Allergy-induced asthma, caused by airborne contaminants such as pollen, mold spores, cockroach or skin debris, and pet-shredded, dried saliva.
What are the symptoms of respiratory problems?
Respiratory: increased breathing, chest pains, shortness of breath, wheeze, heavy cough, speaking difficulty, and chest tightness. The case study patient for this paper presented with episodic shortness of breath, and chest tightness.
How often does chest tightness occur?
The patient presented herself to the healthcare office with complaints over chest tightness and episodic shortness of breath that occurs twice or thrice a month.
What are the symptoms of a smoker's disease?
Also, the disease presents dizziness, fatigue, and abdominal pains. The disease was considered based on the patient’s wheezing, smoking, congestive lungs, breath shortness, and abdominal pains, characteristics that appear in patients with smoking habits. This disease was considered based on the patient physical symptoms.
Can atopic dermatitis cause asthma?
Several results indicate that children with atopic dermatitis can suffer more serious and chronic adult asthma. Differential Diagnoses. 1. Chronic obstructive pulmonary disease (COPD) This disease was considered because the patient is an adult aged 25 years, which is the age group of the case study.
Can asthma patients use inhalers?
Besides, those with critical Asthma are advised to keep their inhalers nearby for use in case of panic attacks or allergic reactions (“Asthma – Diagnosis and treatment – Mayo Clinic,” 2018). Moreover, Asthmatic patients avoid Asthma trigger s such as smoking, perfumes, unprescribed drugs, and irritative pets.
What does the forecast mean for asthma?
What the Forecast Means. Asthma index: a combination of weather factors that can trigger asthma symptoms. A higher index value means more people with asthma will potentially be affected by weather factors, such as changes in temperature or allergens in the air. Allergy index: a combination of weather factors and plant growth stages ...
How does weather affect asthma?
How does the weather affect symptoms? 1 Humid air is moist and heavy. When the air is stagnant, air quality goes down, making breathing harder for everyone. It can trigger an asthma and allergy flare-up since mold and bacteria grow better in moist environments. Humid weather can worsen allergy symptoms. 2 Hot weather often impacts air quality. Ozone can rise to dangerous levels, irritating your respiratory system. Increased traffic, exhaust, smog and other pollutants can make breathing harder if you have asthma. 3 Cold, dry air may seem better for your breathing than hot, humid air, but unfortunately, breathing it in can make the bronchial tubes constrict and spasm as they try to keep airways open, making symptoms worse. 4 Thunderstorms bring barometric changes, high humidity and winds that blow pollen and mold spores everywhere. This can lead to a phenomenon called thunderstorm asthma. In addition, lightning generates nitrogen oxides that can impact ground-level ozone, irritating the lungs and airways. 5 Changing weather patterns alter barometric pressure, which can trigger sinus problems and make breathing harder if you have asthma.
How to manage weather allergies?
How to manage weather allergy symptoms. The key to managing allergy and asthma symptoms is knowing your triggers. You might find cold air ramps up your asthma symptoms. Pollen might bother you a bit, or it can make you miserable. Asthma and allergies are unique to each person, so identifying what worsens your symptoms is vital.
How do pollen counts work?
Pollen counts measure how much pollen is in the air on a given day. Scientists use air sampling devices to collect particles from the air and then analyze them. They identify types of pollen as well as how much of each is in the sample.
What is allergy index?
Allergy index: a combination of weather factors and plant growth stages that increase the release and airborne spread of pollen. A higher index value represents a high pollen count and/or spread of pollen. Flu index: a combination of historical flu data and temperatures. The index represents the degree to which transmission ...
When do allergy patients think of spring?
Spring. When most people think of allergy season, they think of springtime when plants come to life and pollen and mold invade the air. Warm weather and rainfall in spring aids plant growth. Showers may offer allergy patients a break – moisture weighs down the pollen, keeping it on the ground.
Why is it so hard to breathe with asthma?
Increased traffic, exhaust, smog and other pollutants can make breathing harder if you have asthma. Cold, dry air may seem better for your breathing than hot, humid air, but unfortunately, breathing it in can make the bronchial tubes constrict and spasm as they try to keep airways open, making symptoms worse.

Popular Posts:
- 1. uh health patient portal
- 2. uh patient portal cleveland
- 3. northwest orthopaedic patient portal
- 4. dr farr patient portal
- 5. patient report of findings
- 6. http://www.ucsf.edu my patient portal
- 7. rosedale family medical center patient portal.
- 8. follow my patient login
- 9. hendricks regional health patient login
- 10. florida orthopedic patient portal