Patient Fall Incident Report Example - SignNow
12 hours ago Follow the step-by-step instructions below to design your incident report patient fall sample: Select the document you want to sign and click Upload. Choose My Signature. Decide on what kind of signature to create. There are three variants; a typed, drawn or uploaded signature. Create your signature and click Ok. Press Done. >> Go To The Portal
How is a patient Fall recorded and reported?
The mechanism for recording and reporting a patient fall will vary depending on the state and the in-house mechanism the healthcare facility uses. Generally, mishaps such as falls are recorded in an incident report. After the fall, a nurse and a medical provider will likely perform an examination of the patient and document their findings.
What happens if a medical provider fails to prevent a fall?
It could also include failing to diagnose conditions, like a stroke or a seizure, that could lead to falling. In these cases, a medical provider may have broken or violated the appropriate standard of care, because they failed to address conditions that led to a fall or failed to take the necessary precautions to prevent a fall from occurring.
What is a reportable fall?
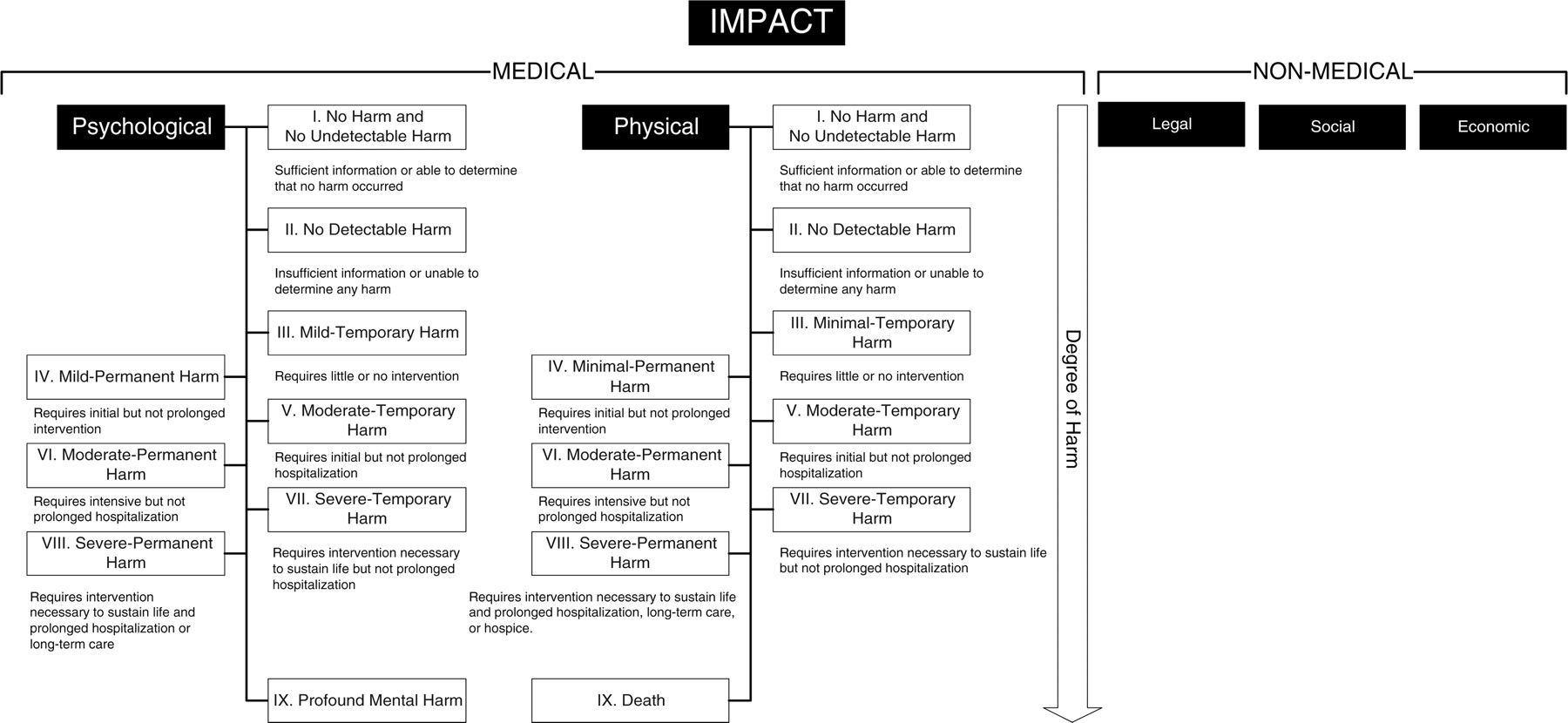
(Figure 2) The Centers for Medicare and Medicaid Services' definition of a reportable fall includes the following: An episode where a resident lost his/her balance and would have fallen, were it not for staff intervention, is a fall. In other words, an intercepted fall is still a fall.
What happens if fall circumstances are not investigated?
If fall circumstances are not investigated at the time of the incident, it is very difficult later to piece together the event and to determine what risk factors were present.
When a resident falls who has already been entered into the FMP, should the nurse send a FAX alert
What is a written full description of all external fall circumstances at the time of the incident?
What is the FMP assessment?
What should a nurse do after a resident falls?
How long does it take to develop a fall care plan?
What is the section A of the TRIPS form?
What is an immediate response?
See more
About this website

Documenting on patient falls or what looks like one in LTC
Thanks everyone for your responses.....however I did proceed to follow through on what I did FIND out or OBSERVE from this patients incident. He was awake and able to answer questions in regard to the fall, I took vitals, gave him a full body assessment, and FOUND out that he was just trying to get up out of bed and his legs gave out.
Documentation of a fall - General Nursing Support, Stories - allnurses
I'm on a ICU stepdown / telemetry unit. If someone falls, and doesn't need anything more than first aid, we: 1) call the doc. 2) enter the incident into the risk management software, detailing where the pt fell, were they on fall precautions, seizure precautions, psych history, blind, dementia, sundowner -- anything that could explain why the person took a header.
Fact Sheet Risk Factors for Falls
Title: Fact Sheet Risk Factors for Falls Author: Department of Health and Human Services \(HHS\) Subject: Fact Sheet Risk Factors for Falls Keywords
Using Fall Risk Assessment Tools in Care Planning
•An 82-year-old man with type 2 diabetes was admitted to the telemetry unit with chest pain and shortness of breath on exertion. •On admission, the patient was alert and oriented to
The Falls Management Program: A Quality Improvement Initiative for ...
T he Falls Management Program (FMP) is an interdisciplinary qualityimprovementinitiative. It is designed to assist nursing facilities in providing individualized,person-centered care,and im-
When a resident falls who has already been entered into the FMP, should the nurse send a FAX alert
When a resident falls who has already been entered into the FMP, the nurse should send a FAX Alert to the primary care provider. The purpose of this alert is to inform the physician, nurse practitioner or physician's assistant of the resident's most recent fall as well as the resident's total number of falls during the previous 180 days.
What is a written full description of all external fall circumstances at the time of the incident?
A written full description of all external fall circumstances at the time of the incident is critical. This includes factors related to the environment, equipment and staff activity. ( Figure 1)
What is the FMP assessment?
In addition to the clues discovered during immediate resident evaluation and increased monitoring, the FMP Falls Assessment is used for a more in-depth look at fall risk. Five areas of risk accepted in the literature as being associated with falls are included. They are:
What should a nurse do after a resident falls?
Upon evaluation, the nurse should stabilize the resident and provide immediate treatment if necessary.
How long does it take to develop a fall care plan?
Results of the Falls Assessment, along with any orders and recommendations, should be used by the interdisciplinary team to develop a comprehensive falls care plan within 1-7 days after the fall. The Fall Interventions Plan should be used by the Falls Nurse Coordinator as a worksheet and to record the final interventions selected for the resident. The interventions listed on this form are grouped in the same five risk areas used for the Falls Assessment.
What is the section A of the TRIPS form?
Section A includes basic resident information, methods for documentation in the medical record and notification of the primary care provider and family. In section B there are questions related to 1) circumstances, 2) staff response and 3) resident and care outcomes.
What is an immediate response?
An immediate response should help to reduce fall risk until more comprehensive care planning occurs. Therefore, an immediate intervention should be put in place by the nurse during the same shift that the fall occurred.
Why do medical professionals review the circumstances surrounding a fall?
The circumstances surrounding the fall are reviewed with the goal of determining what could prevent something like that from happening again. In most cases, medical professionals are required to make an initial evaluation of their patient to determine if they are at risk of falling before administering care.
Why are hospitals required to record falls?
Hospitals are required by law to create a safe environment for their patients and family members visiting the hospital facilities. If a patient slips and falls, most hospitals and nursing homes require their staff to document the fall and notify family members or caregivers. The mechanism for recording and reporting a patient fall will vary ...
What are the different types of falls?
In most medical settings, falls are categorized as: 1 Accidental Falls: These are falls that happen among patients who have very low risk of falling, but they fall because of the environment they are in. They may fall out of bed or slip on a wet floor. 2 Anticipated Physiological Falls: These are the most frequent types of falls. They’re usually caused by an underlying condition affecting the patient. A patient may have a problem walking, their gait may be abnormal, they may be battling with dementia, or they may be on medication that is affecting their balance or their perception. 3 Unanticipated Physiological Falls: These are falls with patients who appear to be low risk for falls, however, they suffer a unexpected negative event. They may faint, they may have a seizure, or they may have a heart attack or a stroke. 4 Behavioral Falls: These are falls that happen because a patient becomes unruly or acts out for one reason or another. These includes instances where patients fall on purpose.
What states require licensed healthcare facilities to report falls to the NQF?
The National Quality Forum includes falls that result in death or serious injury as reportable events. States such as Minnesota require licensed healthcare facilities to report falls to the NQF.
What percentage of hospitalized patients fall?
Research shows that up to 50 percent of hospitalized individuals run the risk of falling. Of those who do fall, 50 percent suffer injury. The injuries sustained from hospital falls range ...
What happens after a fall?
After the fall, a nurse and a medical provider will likely perform an examination of the patient and document their findings. Once the patient has been evaluated and once the report has been compiled, it is generally sent to the hospital’s or the nursing home’s risk management department. The circumstances surrounding the fall are reviewed with ...
How old was the nursing home resident when she fell?
According to reports, a 93-year-old resident fell at the hospital. The nursing home aides assisted her, but no accident reports were written. A few days later, it was noticed that the 93-year-old nursing home resident had extensive bruising on her body. She was taken to the hospital and a few days later died.
What happens when a patient falls within a healthcare environment?
When a patient falls within a healthcare environment, the actions of the staff members can be critical. They can make the difference between life and death, between the patient getting a prompt evaluation for injuries or a delay in treatment, and between normal function and paralysis.
What is the last part of a post fall assessment?
The last part of the post-fall assessment is to review the plan of care and to add more fall prevention strategies. The biggest risk factor for another fall is a history of a prior fall.
What is the first priority of a patient?
The first priority is to make sure the patient has a pulse and is breathing. Next, the caregiver should call for help. Then the providers should assess the patient’s ability to move her arms and legs. The risk of a spinal cord compression from a back or neck injury has to be ruled out before the patient can be moved.
How often should a nurse perform vital signs?
Vital signs and neurological observations should be performed hourly for 4 hours and then every 4 hours for 24 hours, then as required.
When a resident falls who has already been entered into the FMP, should the nurse send a FAX alert
When a resident falls who has already been entered into the FMP, the nurse should send a FAX Alert to the primary care provider. The purpose of this alert is to inform the physician, nurse practitioner or physician's assistant of the resident's most recent fall as well as the resident's total number of falls during the previous 180 days.
What is a written full description of all external fall circumstances at the time of the incident?
A written full description of all external fall circumstances at the time of the incident is critical. This includes factors related to the environment, equipment and staff activity. ( Figure 1)
What is the FMP assessment?
In addition to the clues discovered during immediate resident evaluation and increased monitoring, the FMP Falls Assessment is used for a more in-depth look at fall risk. Five areas of risk accepted in the literature as being associated with falls are included. They are:
What should a nurse do after a resident falls?
Upon evaluation, the nurse should stabilize the resident and provide immediate treatment if necessary.
How long does it take to develop a fall care plan?
Results of the Falls Assessment, along with any orders and recommendations, should be used by the interdisciplinary team to develop a comprehensive falls care plan within 1-7 days after the fall. The Fall Interventions Plan should be used by the Falls Nurse Coordinator as a worksheet and to record the final interventions selected for the resident. The interventions listed on this form are grouped in the same five risk areas used for the Falls Assessment.
What is the section A of the TRIPS form?
Section A includes basic resident information, methods for documentation in the medical record and notification of the primary care provider and family. In section B there are questions related to 1) circumstances, 2) staff response and 3) resident and care outcomes.
What is an immediate response?
An immediate response should help to reduce fall risk until more comprehensive care planning occurs. Therefore, an immediate intervention should be put in place by the nurse during the same shift that the fall occurred.
Popular Posts:
- 1. stowe patient portal
- 2. woodholme gastroenterology patient portal
- 3. umdnj new brunswick patient portal
- 4. is a copy of an incident report placed in a patient record
- 5. pmr patient login
- 6. kenner army health clinic patient portal
- 7. muson patient portal
- 8. my jefferson health patient portal
- 9. patient portal laurie carpentier
- 10. st joes pontiac patient portal