Biopsy Samples and the Diagnosis of Celiac Disease
18 hours ago Conclusion: In the IIM cases presented here, duodenal biopsy findings consistent with celiac disease was sometimes present without classical CeD symptoms or positive traditional CeD serology, and in the majority of cases, the IIM improved after introduction of a gluten-free diet. While extra vigilance towards CeD in IIM patients seems warranted, there is need for more … >> Go To The Portal
Multiple tissue samples are vital to an accurate diagnosis—celiac disease
Celiac Disease
A chronic immune mediated disorder triggered by gluten ingestion.
Full Answer
How accurate is a biopsy for celiac disease?
The researchers note that no current blood test is 100% accurate for identifying celiac disease, and they recommend that physicians continue to perform biopsies in most cases. Click to see full answer
How necessary is a biopsy for celiac disease?
How Necessary is a Biopsy for Celiac Disease? A biopsy has been considered as one of the gold standards to confirm celiac disease, an autoimmune disease that is caused by gluten, a protein found in wheat, barley, and rye. A biopsy is an invasive procedure, so some do not want to undergo it.
What blood test checks for celiac disease?
What tests do doctors use to diagnose celiac disease?
- Blood tests. A health care professional will take a blood sample from you and send the sample to a lab. ...
- Biopsies of the small intestine. A doctor obtains biopsies of the small intestine during an upper GI endoscopy. ...
- Skin biopsies. For skin biopsies, a doctor removes small pieces of skin tissue on and next to the rash. ...
- Genetic testing. ...
What to expect from an endoscopy for celiac disease?
- What to expect. “You will need to fast starting the night before,” Dr. Verma says. ...
- The endoscope. “The endoscope is a long tube, about the width of a thumb,” Verma explains, “and the scope has a light at the end, and a hole for the ...
- Where it goes. “I tell my pediatric patients that the tube takes the same path as your sandwich. ...
How does a biopsy show celiac?
In individuals with celiac disease, gluten damages the villi and causes them to flatten. As a result, the body can't get the nutrients it needs, which leads to many of the health problems associated with celiac disease. With a biopsy, doctors can see if the villi are flattened.
Will a biopsy show celiac disease?
Endoscopies and biopsies are the best way to diagnose celiac disease. A gastroenterologist (doctor who treats people with disorders of the stomach and intestines) will do an endoscopy if your/your child's blood tests or genetic tests show signs of celiac disease.
What happens on a tissue level with celiac disease?
Celiac disease is associated with an inappropriate immune response to a segment of the gluten protein called gliadin . This inappropriate activation of the immune system causes inflammation that damages the body's organs and tissues and leads to the signs and symptoms of celiac disease.
What tissue does celiac disease affect?
If you have celiac disease, eating gluten triggers an immune response in your small intestine. Over time, this reaction damages your small intestine's lining and prevents it from absorbing some nutrients (malabsorption).
Can a positive biopsy for celiac be wrong?
As a result, many people with gluten sensitivity or another food allergy can get a false positive. Dr Amy Burkhart insists, “it is important to keep eating a diet containing gluten until the biopsy is done so the results are accurate”.
What is a positive result for celiac disease?
All celiac disease blood tests require that you be on a gluten-containing diet to be accurate. The tTG-IgA test will be positive in about 93% of patients with celiac disease who are on a gluten-containing diet. This refers to the test's sensitivity, which measures how correctly it identifies those with the disease.
What tests confirm celiac disease?
Two blood tests can help diagnose it: Serology testing looks for antibodies in your blood. Elevated levels of certain antibody proteins indicate an immune reaction to gluten. Genetic testing for human leukocyte antigens (HLA-DQ2 and HLA-DQ8) can be used to rule out celiac disease.
How is Celiacs disease diagnosed?
Doctors use information from your medical and family history, a physical exam, a dental exam link, and medical test results to look for signs that you might have celiac disease and should be tested. Doctors typically diagnose celiac disease with blood tests and biopsies of the small intestine.
Is celiac disease serious?
Celiac disease is a serious autoimmune disease that occurs in genetically predisposed people where the ingestion of gluten leads to damage in the small intestine. It is estimated to affect 1 in 100 people worldwide, but only about 30% are properly diagnosed.
What are the early warning signs of celiac disease?
9 Symptoms of Celiac DiseaseDiarrhea. Loose, watery stool is one of the first symptoms that many people experience before being diagnosed with celiac disease. ... Bloating. Bloating is another common symptom that people with celiac disease experience. ... Gas. ... Fatigue. ... Weight loss. ... Iron deficiency anemia. ... Constipation. ... Depression.More items...
Can you recover from celiac disease?
For example, most children diagnosed with celiac disease heal completely within six months when gluten is removed from their diets. Full healing can take longer for adults, sometimes up to a year or two. People who have symptoms for quite a while may take longer to heal, and some never completely recover.
What does HLA-DQ2 positive mean?
If the test results are positive for HLA DQ2 or DQ8, your child is at risk of developing celiac disease. It doesn't mean they will definitely have celiac disease and the chance of developing celiac disease is still low.
How to diagnose celiac disease?
Diagnosis. The only way to confirm a celiac disease diagnosis is to have an intestinal biopsy. A pathologist will assign a Modified Marsh Type to the biopsy findings. A Type of 3 indicates symptomatic celiac disease. However, Types 1 and 2 may also indicate celiac disease.
Why an Intestinal Biopsy?
An intestinal (duodenal) biopsy is considered the “gold standard” for diagnosis because it will tell you (1) if you have celiac disease, (2) if your symptoms improve on a gluten-free diet due to a placebo effect (you feel better because you think you should) or (3) if you have a different gastrointestinal disorder or sensitivity which responds to change in your diet.
How many duodenal samples should be taken for celiac disease?
It is recommended that the doctor take at least 4-6 duodenal samples from the second part of duodenum and the duodenal bulb, in order to obtain an accurate diagnosis.
What is the procedure to see what is going on inside the GI tract?
If the results of the antibody or genetic screening tests are positive, your doctor may suggest an endoscopic biopsy of your small intestine. An endoscopy is a procedure that allows your physician to see what is going on inside your GI tract. A scope is inserted through the mouth and down the esophagus, stomach and small intestine, ...
How many IELs are there in the immune system?
Density of intra-epithelial lymphocytes (IELs), which are white blood cells found in the immune system. More than 25 I ELs per 100 epithelial cells is significant. Epithelial cells line your intestines and act as a barrier between the inside and the outside of your body.
How long does it take to get a biopsy done?
This procedure takes a little less than thirty minutes and, for adults, sedatives and local anesthetics are used. Children are usually put under general anesthesia. During the biopsy, the gastroenterologist will insert a small tube with a camera through the patient’s mouth and into the digestive tract to the small intestine. 2
Is a bowel surgery painful?
Since there are no nerve endings in the lining of the intestine, the procedure is not painful – though some patients may experience a sore throat.
What is the diagnosis of celiac disease?
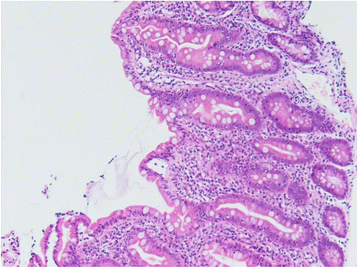
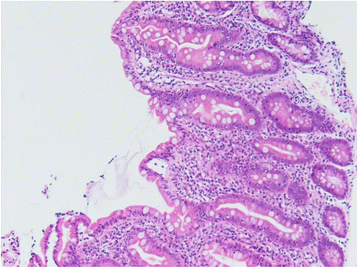
Diagnosis/histology. A small bowel biopsy is obligatory to confirm a diagnosis of celiac disease. The histologic features include increased numbers of intraepithelial lymphocytes, villous shortening or flattening, crypt hyperplasia, and infiltration of the lamina propria with lymphoid cells.
How many biopsies are required for gluten free diet?
The original criteria requiring a series of three biopsies, i.e., first to confirm the diagnosis, second for demonstration of response to a gluten-free diet, and the third for deterioration after gluten challenge, are required only in those few patients in which there still remains some diagnostic uncertainty.
What is the best way to diagnose celiac sprue?
Based on the 1990 revised criteria of the European Society of Pediatric Gastroenterology and Nutrition, the diagnosis of celiac sprue can be made with a diagnostic small bowel biopsy in a patient with highly suggestive clinical symptoms, followed by an objective clinical response to a gluten-free diet. Endoscopic biopsies from the distal duodenum are preferable because the presence of Brunner glands in the duodenal bulb and proximal second portion of the duodenum may affect histologic interpretation. The original criteria requiring a series of three biopsies, i.e., first to confirm the diagnosis, second for demonstration of response to a gluten-free diet, and the third for deterioration after gluten challenge, are required only in those few patients in which there still remains some diagnostic uncertainty.
What is the eosin section of a small bowel biopsy?
Hematoxylin & eosin section from a small bowel biopsy shows numerous round plasmodial forms in the apical cytoplasm of enterocytes, along with numerous intraepithelial lymphocytes .
How to diagnose CD?
Small bowel biopsy remains the gold standard for establishing the diagnosis of CD. Patients who are positive for IgA TTG should undergo esophagogastroduodenoscopy to obtain a small bowel biopsy in order to confirm the diagnosis of CD. The current recommendation is to obtain four to six biopsies from the second part of the duodenum and the mucosa of the bulb. 45–47 The histologic features are described using the Marsh–Oberhuber classification. 48 The spectrum ranges from Marsh 0, with no villous atrophy, to Marsh 4, which refers to total villous atrophy, increased intraepithelial lymphocytes, and crypt hypoplasia. In the presence of positive serology and characteristic histologic changes in the small bowel biopsy, the diagnosis of CD is confirmed.
Why is a small bowel biopsy important?
Small bowel biopsy is important in the evaluation of watery diarrhea. It can detect mucosal diseases such as celiac disease, previously discussed, in addition to eosinophilic enteritis, with the highest yield through duodenal biopsies. Infections with organisms such as Mycobacterium tuberculosis and Strongyloides stercoralis may be identified ...
What is a small intestinal biopsy?
Small intestinal biopsy is the cornerstone of diagnosis and should be undertaken in all patients with suspected celiac disease. Biopsies can be obtained using a capsule with a suction-guillotine mechanism (e.g. Watson capsule).
What is the procedure for celiac disease?
You/your child are scheduled to have an endoscopy and/or biopsy. These procedures are helpful for figuring out if a person has celiac disease. In this handout, you will learn what to expect at your/your child’s endoscopy and/or biopsy .
What is Celiac Disease?
Celiac disease is an autoimmune disease in which a person cannot eat gluten (a protein found in wheat, rye and barley). In people with celiac disease, gluten damages the small intestine. Over time, the damage affects how the small intestine absorbs nutrients from food. Autoimmune diseases cause the immune system (system that fights germs and infections) to mistakenly attack healthy cells.
What are Endoscopy and Biopsy Procedures?
An endoscopy is a procedure in which a doctor looks at the digestive tract (throat, stomach and intestines) with an endoscope (a thin, flexible tube with a light and camera attached). The endoscope is guided down a person’s throat and into their small intestine. An endoscopy does not cause pain because there are no nerve endings in the lining of the small intestine.
Why Do I/My Child Need an Endoscopy and/or Biopsy?
Endoscopies and biopsies are the best way to diagnose celiac disease. A gastroenterologist (doctor who treats people with disorders of the stomach and intestines) will do an endoscopy if your/your child’s blood tests or genetic tests show signs of celiac disease.
How to check for damage in small intestine?
Doctors use an endoscope to check for signs of damage in the small intestine. They will guide the endoscope gently down your/your child’s throat until it reaches the small intestine. The endoscope has tiny tools attached for taking samples. Doctors will take 4-6 small samples of the lining of the small intestine to check under a microscope.
Why does endoscopy not cause pain?
An endoscopy does not cause pain because there are no nerve endings in the lining of the small intestine. A biopsy is a procedure in which doctors remove small pieces of tissue from the body and check them under a microscope for signs of disease or infection.
Can you cure celiac disease with a gluten free diet?
Follow a strict gluten-free diet under the care of a licensed dietitian. While there is no cure for celiac disease, following a gluten-free diet lets the intestine heal. Symptoms typically get better after removing gluten from your/your child’s diet. If the results come back negative ...
How many biopsies are done for celiac disease?
Working in concert with a surgical nurse, the physician will take 5 to 6 biopsies. Each one is taken by grasping sections of the small intestine and slicing them gently away from the walls of the intestine. Multiple tissue samples are vital to make an accurate diagnosis—celiac disease can cause patchy lesions in the duodenum, which can be missed if only one or two samples are taken. Results of the biopsy will confirm if a patient has celiac disease. There are no nerve endings in the lining of the intestine, so this procedure does not cause any pain. Afterward, some patients experience a sore throat, but most have no memory of the procedure.
How to diagnose celiac disease?
If antibody tests and symptoms suggest celiac disease, the physician needs to establish the diagnosis by obtaining tiny pieces of tissue from the upper small intestine to check for damage to the villi. This is done in a procedure called a biopsy.
Are you scheduled for a biopsy? Are you eating gluten?
You must be eating gluten every day, in an amount equivalent to at least 1 slice of bread, for at least 2 to 3 weeks before the procedure. If you are scheduled for a biopsy and are not eating gluten, talk to your doctor about what is necessary to obtain accurate results. If you have eaten gluten only a short time before the biopsy, you and your physician will not know if a negative test result is accurate or due to your diet.
How long does a child have to eat gluten for a biopsy?
The longer a child is on the gluten-free diet, the more difficult it becomes to correctly diagnose the child with celiac disease. (This is also true for adults.) A child may have to eat gluten for 4 to 8 weeks (a gluten challenge) in order to have a biopsy as if that child has been eating gluten for several months or more. A gluten challenge in adults can last 3 months.
How is celiac disease diagnosed?
This is done in a procedure called a biopsy. The physician eases a long, thin tube called an endoscope through the mouth and stomach into the small intestine, and then takes samples of the tissue using small instruments passed through the endoscope. Biopsy remains the most accurate way to diagnose celiac disease.
What is the camera on a small intestine tube?
As the tube is making its way to the small intestine, the camera on the end sends a video image to a monitor in the procedure room. On the monitor the physician can visually assess any evident abnormalities such as ulcers or gastritis. In the small intestine, the physician examines most of the duodenum, the area affected by celiac disease.
Which is the most accurate way to diagnose celiac disease?
Biopsy remains the most accurate way to diagnose celiac disease.
How to diagnose celiac disease?
Celiac Disease is diagnosed only by analyzing biopsies from the small intestine to see that damage has occurred. A Marsh Score is used to rate the extent of damage to the villi. The diagnosis is then confirmed with a positive response to the gluten free diet.
How is celiac disease diagnosed?
This is done in a procedure called a biopsy: the physician eases a long, thin tube called an endoscope through the mouth and stomach into the small intestine, and then takes samples of the tissue using instruments passed through the endoscope. Biopsy of the small intestine is the only way to diagnose celiac disease.
How long does a gluten free child have to eat gluten?
(This is also true for adults.) A child may have to eat gluten for 12 weeks (a gluten challenge) in order to have a biopsy if that child has not been eating gluten for several months or more. A gluten challenge in adults can last three months.
Why is it important to remove tissue under a microscope?
This is why the surgical removal of tissue is so important, for it is only under a microscope that a definitive diagnosis of celiac disease can be made . At this point, the physician will insert a tiny surgical instrument through the tube.
How to diagnose DH?
DH is diagnosed by a skin biopsy, which involves removing a tiny piece of skin near the rash and testing it for the IgA antibody. DH is treated with a gluten-free diet and medication to control the rash, such as dapsone or sulfapyridine. Drug treatment is short term, usually until the gluten-free diet starts to relieve symptoms. It is not necessary to perform an intestinal biopsy to establish the diagnosis of celiac disease in a patient with DH; the skin biopsy is definitive.
How many areas of the small intestine are biopsy taken?
It reaches the small intestine, and working in concert with a surgical nurse, the physician will biopsy 5-6 areas of the small intestine. The biopsy is taken by grasping very small sections of tissue and slicing them gently away from the walls of the intestine. Multiple tissue samples are also vital to an accurate diagnosis-celiac disease can cause ...
Can you have celiac disease if you have not been biopsied?
While many people who have not been biopsied may not have celiac disease, this approach to the gluten-free diet is concerning for those who do in fact have celiac disease but don't really know it.
Popular Posts:
- 1. patient portal pwhc
- 2. erik stromeyer radiologist patient portal
- 3. cochise health and wellness patient portal
- 4. angel patient portal dr donna bacon
- 5. penn highlands huntingdon patient portal
- 6. health care partners nevada patient portal
- 7. hendricks regional health patient payment portal
- 8. patient portal takecarehealth sites rutherford county
- 9. gainesville digestive associates patient portal
- 10. what's myhealth? patient portal