Subjective Report - an overview | ScienceDirect Topics
34 hours ago The patient’s report of pain, pressure, and nausea are subjective data because only the patient can feel the sensation of pain or pressure and nauseous sensation. The report of fever off and on is subjective because the nurse did not measure the temperature on the previous days. >> Go To The Portal
Full Answer
What should be included in symptom description and subjective report?
Symptom Description and Subjective Report may contain information told to the clinician and can include direct quotations of clients such as, "These visits are really helping me to strengthen my parenting" or "I think that these coping strategies are really working; I was able to concentrate at work all day."
What is subjective data in a patient interview?
Patients are first asked the reason for visiting the doctor. Then whatever they say is classified as the subjective data. Patients often complain about physical symptoms pertaining to how they feel. This can be pain, discomfort, itching or any type of abnormal sensations.
How do you conduct a subjective health assessment?
The Complete Subjective Health Assessment The complete subjective health assessment is commonly referred to as a health history. It provides an overview of the client’s current and past health and illness state. You conduct it by interviewing the client as illustrated in Figure 1.1, asking them questions, and listening to their narrative.
Can you observe signs in a subjective assessment?
Although you can observe signs, in the context of a subjective assessment, the client shares this subjective information with you. For example, a rash is both subjective and objective data as it could be something that the client shares with you, but it is also something that you can observe.
What is subjective patient information?
Subjective data is gathered from the patient telling you something that you cannot use your five senses to measure. If a patient tells you they have had diarrhea for the past two days, that is subjective, you cannot know that information any other way besides being told that is what happened.
What is a subjective statement in healthcare?
Subjective data is going to be information that you receive from the patient or from one of his or her knowledgeable companions. Subjective data is what you are able to pull from the patient such as how they are feeling, what their symptoms are, or what their current concerns are.
What is a subjective documentation?
Subjective. The subjective section of your documentation should include how the patient is currently feeling and how they've been since the last review in their own words. As part of your assessment, you may ask: “How are you today?” “How have you been since the last time I reviewed you?”
What is subjective charting?
0:073:33SUBJECTIVE VS OBJECTIVE DATA (NURSING) - YouTubeYouTubeStart of suggested clipEnd of suggested clipSo for example this would be like the patient's pain level if they feel tingling in their legs. OrMoreSo for example this would be like the patient's pain level if they feel tingling in their legs. Or their past experiences.
What is subjective assessment in nursing?
The complete subjective health assessment is commonly referred to as a health history . It provides an overview of the client's current and past health and illness state. You conduct it by interviewing the client as illustrated in Figure 1.1, asking them questions, and listening to their narrative.
What is subjective information in nursing?
Subjective nursing data are collected from sources other than the nurse's observations. This type of data represents the patient's perceptions, feelings, or concerns as obtained through the nursing interview. The patient is considered the primary source of subjective data.
What does subjective mean in medical terms?
sub·jec·tive (sŭb-jek'tiv), 1. Perceived only by the patient only and not evident to the examiner; said of certain symptoms, such as pain. 2. Colored by one's personal beliefs and attitudes.
What is difference between subjective and objective reporting?
Subjective information or writing is based on personal opinions, interpretations, points of view, emotions and judgment. It is often considered ill-suited for scenarios like news reporting or decision making in business or politics. Objective information or analysis is fact-based, measurable and observable.
How do you document subjective data?
When documenting subjective data, provide accurate examples of what the client said using quotation marks to identify her or his comments. Objective data is data that can be observed, such as “client was crying,” or measured, such as the blood pressure is 120/80.
Why is subjective information important in patient documentation?
The subjective examination is often undervalued in the assessment and management of a patient. It is the most crucial aspect of the examination as it determines the severity, irritability and nature (SIN) of the patient's condition.
What is objective patient data?
Objective patient data involves measurable facts and information like vital signs or the results of a physical examination. Subjective patient data, according to Mosby's Medical Dictionary, “are retrieved from” a “description of an event rather than from a physical examination.”
What is an example of a subjective statement?
The sentence “It's very cold outside” is a subjective statement, because how true this sentence is depends on personal opinions and experiences. Many temperatures would feel very cold to someone who grew up in Arizona, but comfortably warm to someone who grew up in Alaska.
What is subjective and objective in medical?
Subjective data are information from the client's point of view (“symptoms”), including feelings, perceptions, and concerns obtained through interviews. Objective data are observable and measurable data (“signs”) obtained through observation, physical examination, and laboratory and diagnostic testing.
What is an example of a subjective observation?
A subjective observation includes your opinions and assessments. Using the same example: Kimber showed determination and patience while trying to put her sweater on. She didn't get upset.
What is the difference between subjective and objective?
Based on or influenced by personal feelings, tastes, or opinions. Objective: (of a person or their judgement) not influenced by personal feelings or opinions in considering and representing facts.
What is the difference between subjective and objective assessment?
Objective means making an unbiased, balanced observation based on facts which can be verified. Subjective means making assumptions, making interpretations based on personal opinions without any verifiable facts. Objective observations or assessments can be used before arriving at any decisions.
What is objective in medical terminology?
Objective. Information that you observe when conducting a physical assessment, and lab and diagnostic results. You observe that a client has a bright red rash on the dorsal side of the foot, the lateral malleolus, and anterior and lateral side of the lower leg.
What is subjective assessment?
A term often used in reference to, or in place of, the complete subjective health assessment. Information that the client shares with the health professional. Information that the health professional collects when performing a physical exam. Something that the client feels.
Can you observe signs in a subjective assessment?
Although you can observe signs, in the context of a subjective assessment, the client shares this subjective information with you. For example, a rash is both subjective and objective data as it could be something that the client shares with you, but it is also something that you can observe.
What is a care partner?
Care partners are family and friends who are involved in helping to care for the client. You may hear care partners being referred to as “informal caregivers” or “family caregivers,” but “care partner” is a more inclusive term that acknowledges the energy, work, and importance of their role.
What is the difference between subjective and objective data?
The signs refer to the objective data, while the symptoms refer to the subjective data. Here is a way to help you distinguish between them. Notice the words 'subjective' and 'says' both begin with the letter 'S,' while 'objective' and 'observes' begin with the letter 'O.'. Sometimes the data can be subjective and objective at the same time.
What does it mean when a patient says she has stomach pain?
A patient says she has stomach pain as the nurse observes her clutching her abdomen. There can also be times when the subjective and objective data do not match. The patient may state having a certain symptom or belief, but observations of them reveal something different.
What is objective data?
Objective data is another type of information that is collected from patients. It can be defined as the data medical professionals obtain through observations by seeing, hearing, smelling and touching. This can include patient behaviors, actions and information gathered from test measurements or the physical examination.
What is subjective data in nursing?
Subjective data in nursing is part of the health assessment that involves collecting information through communication. Patients are first asked the reason for visiting the doctor. Then whatever they say is classified as the subjective data. Patients often complain about physical symptoms pertaining to how they feel.
What are the symptoms of a symtom?
Patients often complain about physical symptoms pertaining to how they feel. This can be pain, discomfort, itching or any type of abnormal sensations. They state problems they are experiencing with their bodies, such as coughing, vomiting or muscle spasms.
Why do people think they have a particular illness?
They may think they have a particular illness because they had it before or researched their symptoms on the Internet. Other patients may feel they are healthy and just want a doctor's check-up.
Is chest pain subjective or objective?
A patient complaining of mild chest pain may not be aware that what he thinks is indigestion could actually be a heart attack. Subjective data is different from objective data, which is the data medical professionals obtain through observations by seeing, hearing, smelling and touching. Learning Outcomes.
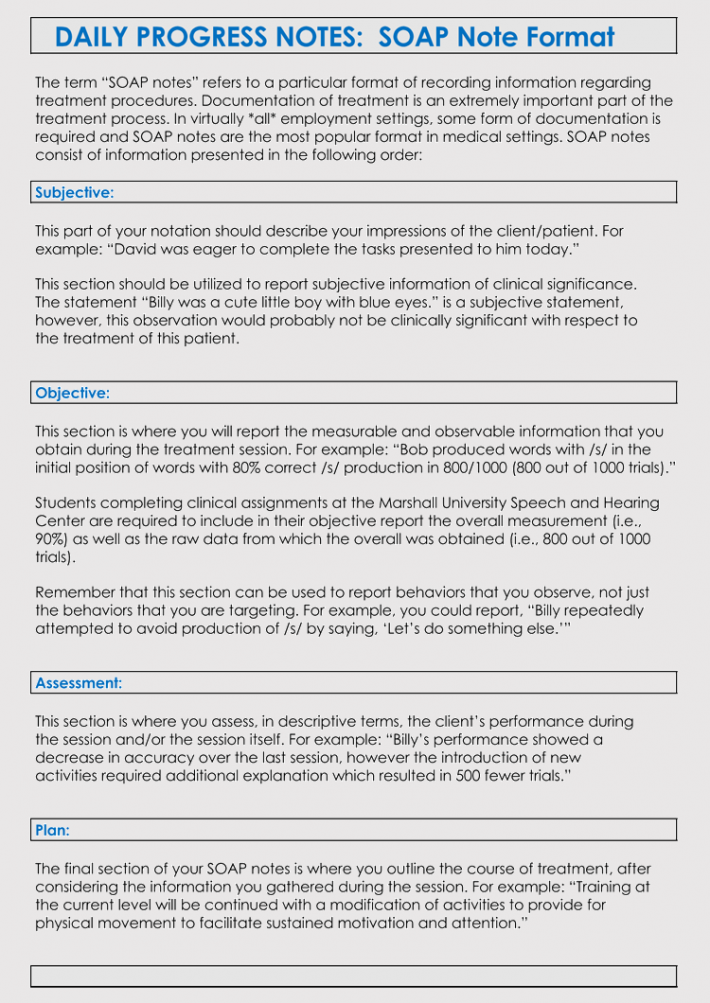
How to edit a note header?
To edit information in the note header such as the Note Title or Service Code or to add information such as add-on codes, click anywhere on the note header or click Edit in the upper right corner.
What is Relevant Content field?
The Relevant Content field is also where you can document specific information about conversations or interventions used during the session. If you want to take notes about conversations in the appointment, or document private thoughts or impressions, you may want to use a Process Note as well.
What is a plan of action?
The Plan is the clinician’s plan of action, if any, and includes recommendations for the client or collateral contacts, therapeutic interventions, and a prognosis (poor, guarded, fair, good or excellent). Use the Recommendation radio buttons to document your treatment recommendations. Enter how often you plan to see the client going forward in the Prescribed Frequency of Treatment field.
What is progress note?
Progress Notes contain a full Current Mental Status exam. Use our one-click autofill options ( All Normal or All Not Assessed) to simultaneously fill each of the fields, click in each field to select from a list of common responses, or enter your own information in each field.
What is objective content?
Objective Content. Report the measurable and observable information that you obtain during the session. Here, you may report behaviors that you observe, not just the behaviors you are targeting. There are two types of objective data: the provider’s observations and outside written materials.
Can electronic signatures be edited?
The application automatically captures the timestamp for the signature as well. Electronic signatures cannot be edited or modified.
Popular Posts:
- 1. norman smith bowie patient portal
- 2. dr barimo patient portal
- 3. dr. william silver patient portal
- 4. synergy family phisicians patient portal
- 5. rapha family medicine patient portal
- 6. patient portal email gateway
- 7. womens health services patient portal
- 8. partners portal patient
- 9. patient report to a clinic with complaints of breast tenderness few merkley's
- 10. acmh patient portal