Medicare Progress Note Requirements for Physical Therapy Guide
31 hours ago or. The U.S. Department of Health and Human Services – Office of the Inspector General. Provider fraud or abuse in a Medicare Advantage Plan or a Medicare drug plan (including a fraudulent claim) 1-800-MEDICARE (1-800-633-4227) or. The Investigations Medicare Drug Integrity Contractor. (I-MEDIC) at 1-877-7SAFERX (1-877-772-3379), or by US mail: >> Go To The Portal
Full Answer
What is the purpose of a Medicare progress report?
Terminate services, if necessary (see the discharge note section below). According to Jewell and Wallace, “The Medicare progress report is intended to address the patient’s progress toward his or her goals as noted in the established plan of care.
What is the proper format for a progress note for Medicare?
There is no particular format required by Medicare as long as all the above is contained in the note as long as it happens at least once every 10 treatment visits. When co-treating a patient with a PTA or OTA the PT or OT must personally provide one full billable service on one date of service (DOS) within that progress note period.
What is included in a patient progress report template?
This Sample Patient Progress Report Template has the patient's personal information, physiological and psychological health progress. The progress report specifies the patient's mood, communication, appearance, emotional status, mental stability, interventions, and respond to treatment, and the report summary.
How often should I report my patient’s progress?
The Centers for Medicare and Medicaid Services (CMS) provides some relatively standard requirement for progress reports. For example, their guidelines clearly state that a clinician is required to report once every 10 treatment days.
How often does Medicare require a progress note?
every 10 treatment daysMedicare requires a Progress Report be completed at least every 10 treatment days. The next reporting period begins on the next treatment day after the Progress Report was performed. It is important to know that the dates for recertification of a Medicare POC do not affect the dates of a required Progress Report.
Does Medicare require progress note every 30 days?
Medicare requires that a licensed physician or nonphysician practitioner (NPP) date and sign the POC within 30 days. To make things easier, though, the certifying physician doesn't have to be the patient's regular physician—or even see the patient at all (although some physicians do require a visit).
How do I write a PT progress report?
6:068:18How to Write a Physical Therapy Progress Note - YouTubeYouTubeStart of suggested clipEnd of suggested clipControl for better scapular mechanics recommended continuation of therapy two times a week for threeMoreControl for better scapular mechanics recommended continuation of therapy two times a week for three weeks to achieve goals all right on to the final portion of the progress.
What are the Medicare requirements for documenting levels of assistance?
Requirements: Documentation must show objective loss of joint motion (degrees of motion), strength (strength grades), or mobility (levels of assistance) Documentation must show how these therapeutic exercises are helping the patient progress towards their stated, objective and measurable goals.
How often should progress notes be written?
once every 10 treatment visitsProgress Reports need to be written by a PT/OT at least once every 10 treatment visits.
When do you use a progress note?
Progress notes serve as a record of events during a patient's care, allow clinicians to compare past status to current status, serve to communicate findings, opinions and plans between physicians and other members of the medical care team, and allow retrospective review of case details for a variety of interested ...
How do you write PT notes?
9:1710:21How to Write Clinical Patient Notes: The Basics - YouTubeYouTubeStart of suggested clipEnd of suggested clipMake sure you've got some sort of heading if you're in a multidisciplinary or a hospital basedMoreMake sure you've got some sort of heading if you're in a multidisciplinary or a hospital based environment. So that people know who is writing this note and what it's for make. Sure you have the date.
How do you write a good physical therapy note?
0:544:27How to Write a Progress Note for Physical Therapy - YouTubeYouTubeStart of suggested clipEnd of suggested clipAnd may even require you to complete a progress note sooner than that in that case you need toMoreAnd may even require you to complete a progress note sooner than that in that case you need to follow the rules. Set by your state okay now let's dive into the anatomy of a progress note as outlined.
How do you write a physical therapy assessment?
11:2715:45How To Write a Physical Therapy Evaluation - YouTubeYouTubeStart of suggested clipEnd of suggested clipInformation as a baseline to show how the patient is progressing with physical therapy. And even ifMoreInformation as a baseline to show how the patient is progressing with physical therapy. And even if you were unable to complete every necessary test during your initial. Evaluation.
What are the criteria for documentation of medical necessity?
How does CMS define medical necessity?“Be safe and effective;Have a duration and frequency that are appropriate based on standard practices for the diagnosis or treatment;Meet the medical needs of the patient; and.Require a therapist's skill.”
What should be documented in a patient's medical record?
They should include: 1) All relevant clinical findings. 2) A record of the decisions made and actions agreed as well as the identity of who made the decisions and agreed the actions. 3) A record of the information given to patients. 4) A record of any drugs prescribed or other investigations or treatments performed.
Who is able to document in a patient health record?
Anyone documenting in the medical record should be credentialed and/or have the authority and right to document as defined by facility policy. Individuals must be trained and competent in the fundamental documentation practices of the facility and legal documentation standards.
What is a plan of care for Medicare?
When treating Medicare patients, the Plan of Care refers to the written treatment plan for which the intended therapy services must specifically relate to. The Plan of Care is established at the time of the first visit with the patient and is derived from the clinical information gathered during the Initial Therapy Evaluation.
Can Medicare deny POCs?
Since Medicare could potentially deny or claw back payment if the above time frames are not met, it is essential that your practice establish a workflow to keep track of Medicare POCs and Progress Reports. If your EMR does not offer a tracking system, then this may end up being a manual process using home grown spreadsheets or some other recording method. However, if you are an OptimisPT user, you can take advantage of the embedded alerts, reminders and reports that can track this for you.
What is client progress report?
Client Progress Report for Psychotherapy PDF template provides the essential information that should contain in a clinical psychotherapy report such as the name of the patient, the type of session made with the patient, the date of the session, a comprehensive assessment, and treatment goals and objective for the patient/client.
What is a school counselor's progress report?
School Counseling Progress Report Sample will help teachers or school counselors to record and monitor students progress in an efficient manner. It provides a standard way of scoring or evaluating students.
What is a BMI chart?
BMI Chart document useful for both individuals and dietitians to track and document their records. The report comes with a BMI Chart and provides body metrics of submitters with their BMI Score and the body type they fit in.
How often do you need a progress note for Medicare?
Currently, Medicare only requires a progress note be completed, at minimum, on every 10th visit. I hope that helps!
What is a progress note for a therapist?
In it, the therapist must: Include an evaluation of the patient’s progress toward current goals. Make a professional judgment about continued care.
How long does it take for Medicare to recertify?
And even when things do go according to plan, Medicare requires recertification after 90 days of treatment. If you’re a WebPT Member, you can use WebPT’s Plan of Care Report to identify which plans of care are still pending certification as well as which ones require certification—before those 90 days are up.
What is a POC in therapy?
The Plan of Care (POC) Based on the assessment, the therapist then must create a POC —complete with treatment details, the estimated treatment time frame, and the anticipated results of treatment. At minimum, Medicare requires the POC to include: Medical diagnosis. Long-term functional goals.
How long does it take to sign a POC?
Medicare requires that a licensed physician or nonphysician practitioner (NPP) date and sign the POC within 30 days. To make things easier, though, the certifying physician doesn’t have to be the patient’s regular physician—or even see the patient at all (although some physicians do require a visit).
How long does it take for Medicare to discharge a patient?
Medicare automatically discharges patients 60 days after the last visit. Unfortunately, if the patient has been discharged, then you will need to perform a new initial evaluation. If you do not live in a direct access state, then you will also need to to get the physician's signature on the patient's new POC.
What is the evaluation of a licensed therapist?
Before starting treatment, the licensed therapist must complete an initial evaluation of the patient, which includes: Objective observation (e.g., identified impairments and their severity or complexity) And, of course, all of this should be accounted for you in your documentation.
What should be included in a progress report for Medicare?
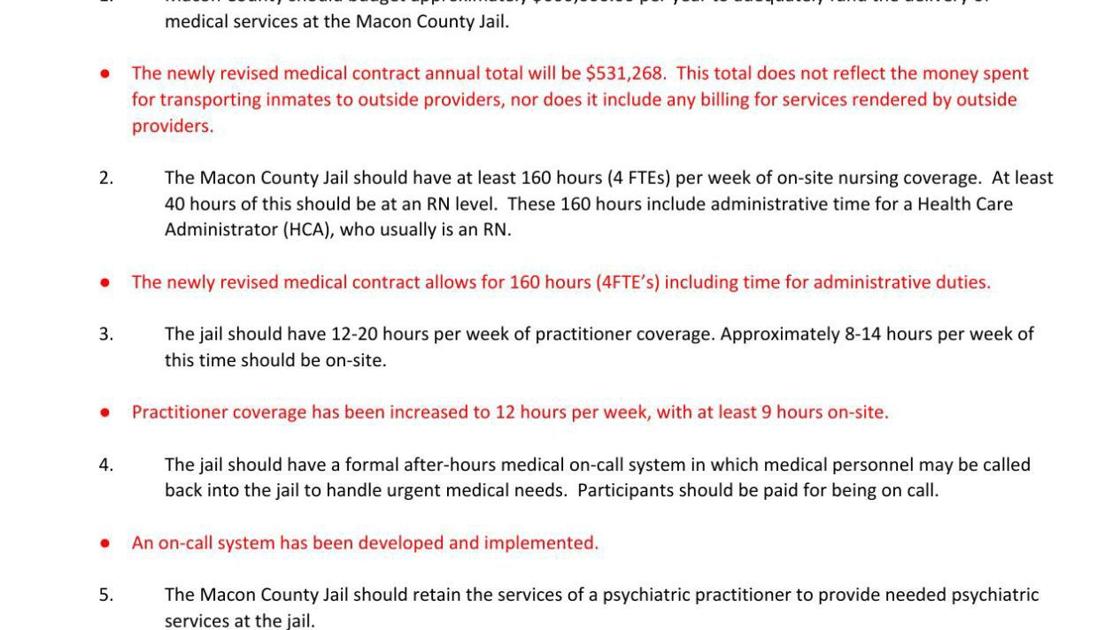
Now that we know when to complete a progress report, let’s look at the required 7 of the things that your progress reports should include for individuals receiving outpatient therapy through the Medicare program: 1) Include the start and end date of the reporting period, as well as the date that the report was written.
How often do you need to report progress on Medicare?
For example, their guidelines clearly state that a clinician is required to report once every 10 treatment days.
What is progress report?
Let’s examine the 7 things your progress reports must include. Progress reports are an essential component of a patient’s recovery process. They help ensure that the patients are on the right track, and that the treatment they’re receiving is having a positive affect on them.
Do progress reports have to be the same?
Generally speaking, progress reports have certain requirements that are the same across the board, and they can have certain requirements that are unique to individual payors—it’s up to you to get in touch with the payors and find out exactly what’s required by them.
How often do you need to complete a progress report?
A clinician must complete a progress report at least once every 10 treatment days or at least once during each certification interval, whichever is less. The beginning of the first reporting period is the first day of the episode of treatment regardless of whether the service provided on that day is an evaluation, re-evaluation, or treatment.
What is the beginning of the first reporting period?
The beginning of the first reporting period is the first day of the episode of treatment regardless of whether the service provided on that day is an evaluation, re-evaluation, or treatment. Progress notes should contain: An assessment of improvement, extent of progress (or lack thereof) toward each goal;
What is an evaluation in a plan of care?
Evaluation. The initial evaluation, or the plan of care including an evaluation, should document the necessity for a course of therapy through objective findings. Documentation of the evaluation should list the conditions and complexities and, where it is not obvious, describe the impact of the conditions and complexities on ...
What is the Medicare requirement for therapy?
In general, Medicare requires that therapy services are of appropriate type, frequency, intensity, and duration for the individual needs of the patient. Documentation should: Establish the variables that influence the patient's condition, especially those factors that influence the clinician's decision to provide more services than are typical ...
When is therapy service payable?
The Centers for Medicare and Medicaid Services (CMS) states that therapy services shall be payable when the medical record and the information on the claim form consistently and accurately report covered therapy services. Documentation should also include objective measures of the patient's improvement as a means to justify therapy services ...
What is discharge note?
The Discharge Note is required and shall be a progress report written by a clinician and shall cover the reporting period from the last progress report to the date of discharge. The discharge note shall include all treatment provided since the last progress report and indicate that the therapist reviewed the notes and agrees to the discharge.
What is the long term treatment goal?
Long term treatment goals should be developed for the entire episode of care and not only for the services provided under a plan for one interval of care . The plan of care shall contain, at minimum, the following information: Type, amount, duration, and frequency of therapy services.
What is Medicare Administrative Contractor?
The Medicare Administrative Contractor is hereby advised that this constitutes technical direction as defined in your contract. CMS does not construe this as a change to the MAC Statement of Work. The contractor is not obligated to incur costs in excess of the amounts allotted in your contract unless and until specifically authorized by the Contracting Officer. If the contractor considers anything provided, as described above, to be outside the current scope of work, the contractor shall withhold performance on the part(s) in question and immediately notify the Contracting Officer, in writing or by e-mail, and request formal directions regarding continued performance requirements.
What is an initial evaluation?
The initial evaluation, or the plan of care including an evaluation, should document the necessity for a course of therapy through objective findings and subjective patient self-reporting. Utilize the guidelines of the American Physical Therapy Association, the American Occupational Therapy Association, or the American Speech-Language and Hearing Association as guidelines, and not as policy. Only a clinician may perform an initial examination, evaluation, re-evaluation and assessment or establish a diagnosis or a plan of care. A clinician may include, as part of the evaluation or re-evaluation, objective measurements or observations made by a PTA or OTA within their scope of practice, but the clinician must actively and personally participate in the evaluation or re-evaluation. The clinician may not merely summarize the objective findings of others or make judgments drawn from the measurements and/or observations of others.
What is the purpose of a treatment note?
The purpose of these notes is simply to create a record of all treatments and skilled interventions that are provided and to record the time of the services in order to justify the use of billing codes on the claim. Documentation is required for every treatment day, and every therapy service. The format shall not be dictated by contractors and may vary depending on the practice of the responsible clinician and/or the clinical setting.
Is speech language pathology a Medicare insured?
Services of speech-language pathology assistants are not recognized for Medicare coverage. Services provided by speech-language pathology assistants, even if they are licensed to provide services in their states, will be considered unskilled services and denied as not reasonable and necessary if they are billed as therapy services.
Can an occupational therapy assistant write a progress report?
Occupational Therapy Assistants may write elements of the Progress Report dated between clinician reports. Reports written by assistants are not complete Progress Reports. The clinician must write a Progress Report during each Progress Report Period regardless of whether the assistant writes other reports. However, reports written by assistants are part of the record and need not be copied into the clinicians report. Progress Reports written by assistants supplement the reports of clinicians and shall include:
Can a therapist bill Medicare?
In order to qualify to bill Medicare directly as a therapist, each individual must be enrolled as a private practitioner and employed in one of the following practice types: an unincorporated solo practice, unincorporated partnership, unincorporated group practice, physician/NPP group or groups that are not professional corporations, if allowed by state and local law. Physician/NPP group practices may employ physical therapists in private practice (PTPP) and/or occupational therapists in private practice (OTPP) if state and local law permits this employee relationship.
How often do you need to report progress on Medicare?
Per the Medicare Benefit Policy Manual, “The minimum progress report period shall be at least once every 10 treatment days. The day beginning the first reporting period is the first day of the episode of treatment regardless of whether the service provided on that day is an evaluation, reevaluation or treatment.
Who is responsible for noting the progress report?
Additionally, if a PTA assisted with the progress report, then that assistant must sign the note. Physical therapists, on the other hand, are solely responsible for noting the following required information: assessment of patient improvement or progress toward each goal;
What is an unanticipated discharge?
In the case of an unanticipated discharge (e.g., the patient stops showing up for therapy or self-discharges), the therapist may base any treatment or goal information on the previous treatment notes or the verbal reports of a PTA or other clinician.
What is discharge summary?
Functionally, a discharge summary (a.k.a. discharge note) is a progress note that covers the reporting period from the last progress report to the date of discharge. The discharge summary is required for each episode of outpatient therapy treatment.
What information is needed for physical therapy?
Physical therapists, on the other hand, are solely responsible for noting the following required information: 1 assessment of patient improvement or progress toward each goal; 2 decision regarding continuation of treatment plan; and 3 any changes or additions to the patient’s therapy goals.
What is progress note?
According to Mosby’s medical dictionary, progress notes are “notes made by a nurse, physician, social worker, physical therapist, and other health care professionals that describe the patient’s condition and the treatment given or planned.”.
Do you have to sign a discharge document?
To answer your question, no, a discharge document does not need to be signed by the patient's physician. That being said, some physicians may request you send them a copy of the discharge summary once the patient has been discharged from your care, but this is not a Medicare requirement.
Do I need a separate form for a physician certification?
AFTER: A specific, separate form is not needed. Other existing documentation may serve as the certification if the appropriate information is included. In addition, we added to the list of non-physician practitioners that may sign a certification statement when one cannot be obtained from the physician.
Do you need a separate statement for home health recertification?
Home health recertification documentation. BEFORE: Physicians needed to include a separate statement about how much longer home health services would be needed as part of the home health recertification. AFTER: A separate statement is not needed.
When to Use A Progress Report vs. A Plan of Care When Treating Medicare Patients
Plan of Care
- When treating Medicare patients, the Plan of Care refers to the written treatment plan for which the intended therapy services must specifically relate to. The Plan of Care is established at the time of the first visit with the patient and is derived from the clinical information gathered during the Initial Therapy Evaluation. Per Medicare, the minimal information required in the Plan of Care is as follows: 1. Diagnosis 2. Long-term treatment goals 3. T…
Progress Reports
- A Progress Report provides justification for the medical necessity of the skilled therapy being provided to the patient. Per Medicare, a Progress Report should include: 1. Objective evidence to support the need for skilled treatment 1.1. This includes such things as validated functional outcome measures and standardized patient assessment tools. Th...
Staying Compliant with Time Frames
- Since Medicare could potentially deny or claw back payment if the above time frames are not met, it is essential that your practice establish a workflow to keep track of Medicare POCs and Progress Reports. If your EMR does not offer a tracking system, then this may end up being a manual process using home grown spreadsheets or some other recording method. However, if you are an OptimisPT user, you can take advantage of the embedded …