Preventive Medicine Services Reporting - AAPC Knowledge Center
36 hours ago Preventive Medicine Services Reporting. By John Verhovshek. In Coding. October 31, 2018. 7 Comments. Print Post. Preventive medicine services, or “well visits,” are evaluation and management (E/M) services provided to a patient without a chief complaint. The reason for the visit is not an illness or injury (or signs or symptoms of an illness or injury), but rather to evaluate the patient’s overall health, and to identify potential health problems … >> Go To The Portal
Full Answer
What is the difference between preventive medicine and Preventive Medicine reports?
While Preventive Medicine focuses on publishing articles that appeal more broadly to the preventive medicine and health promotion communities, Preventive Medicine Reports publishes papers that have a … Associations of Telemedicine vs.
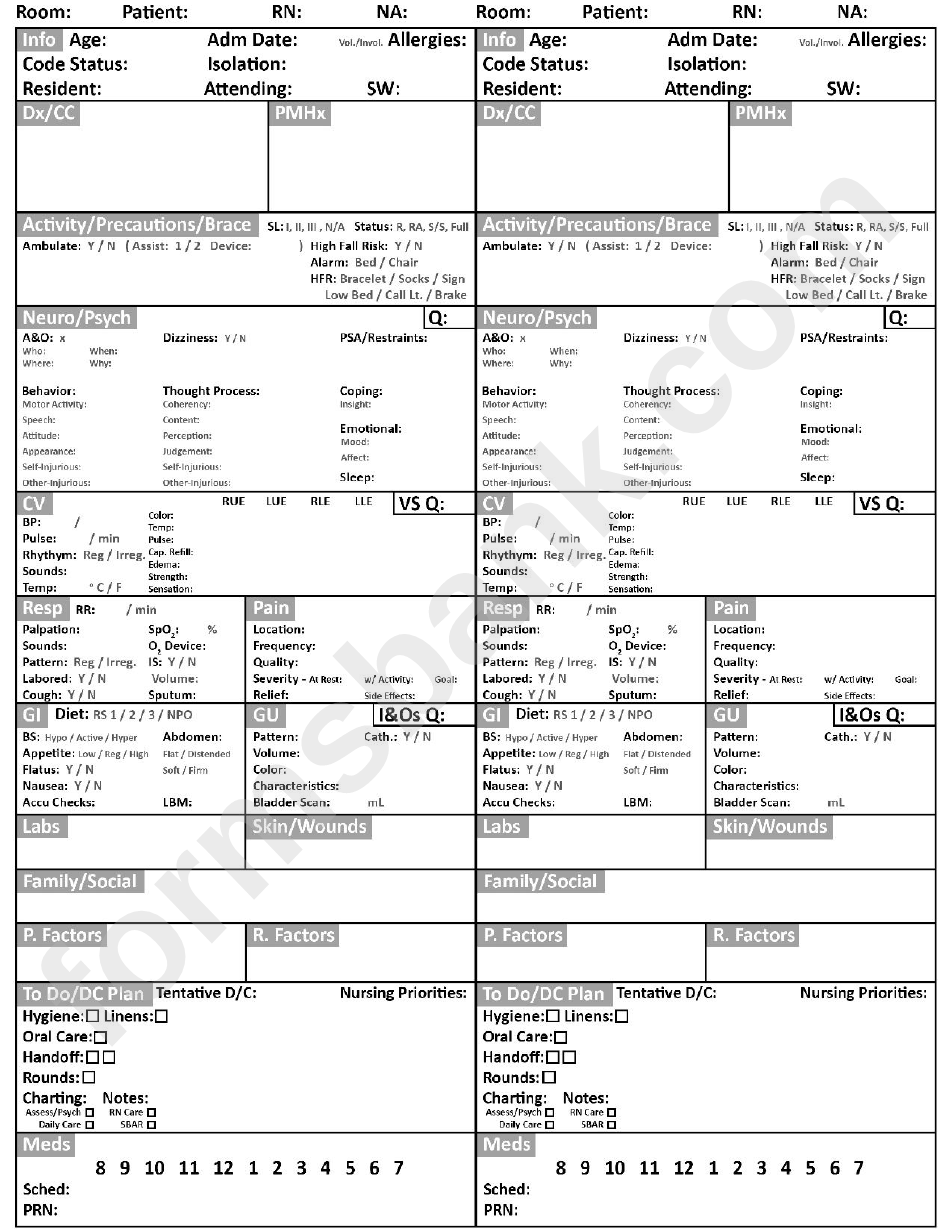
What is a patient report form?
Report Forms FREE 14+ Patient Report Forms in PDF | MS Word Healthcare personnel in hospitals or medical centers ensure that they provide the needs of the patients (pertaining to the treatments or medications needed) and their individual relatives (pertaining to the answers or provision of exact details from the medical results).
Why should you secure your patient report forms?
In other words, the patient report forms are organized and layered which makes it easier to be filled with all the relevant information. And when all the precise information are provided, it is much easier to assess or evaluate the current state of one’s health condition. There are further reasons or purposes why patient reports should be secured.
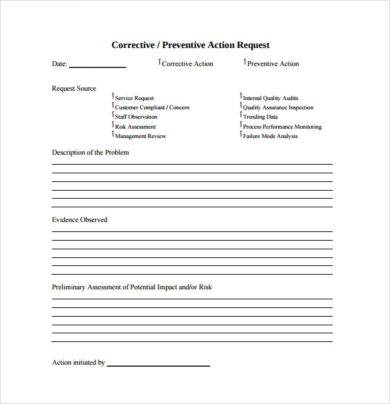
What should be included in a patient incident report?
A patient incident report should include the basic information about the incident: the who, what, where, when and how. You should also add recommendations on how to address the problem to reduce the risk of future incidents. Every facility has different needs, but your incident report form could include:
What is a preventive health assessment?
They're known as tests that look for diseases before symptoms are present. In terms of conditions that often show no warning signs, preventive health screenings can be very effective at providing insights about early disease risk so you can take proactive steps with your doctor to prevent chronic illnesses.
What needs to be documented for preventive visits?
Documentation requirements for a preventive visit such as an “annual physical” include an age- and gender-appropriate history and physical examination, counseling or anticipatory guidance, and risk factor reduction interventions.
What does preventive mean in medical terms?
Preventive medicine: Medical practices that are designed to avert and avoid disease. For example, screening for hypertension and treating it before it causes disease is good preventive medicine. Preventive medicine takes a proactive approach to patient care.
How do you document preventive services?
Preventive Service Codes Codes 99381-99397 represent these services, and their selection is based on whether the patient is receiving an initial (new patient) or a periodic (established patient) preventive service, as well as the patient's age.
What is included in a preventive medicine visit?
You take the patient's interval medical, family and social history and perform a complete review of systems. You also perform a physical examination that includes a blood-pressure check and thyroid, breast, abdominal and pelvic examinations, and you obtain a Pap smear.
What is the diagnosis code for preventive care?
121, Z00. 129, Z00. 00, Z00. 01 “Prophylactic” diagnosis codes are considered Preventive.
What are the 3 levels of prevention?
Primary Prevention—intervening before health effects occur, through.Secondary Prevention—screening to identify diseases in the earliest.Tertiary Prevention—managing disease post diagnosis to slow or stop.
Why is preventive health care important?
Getting preventive care reduces the risk for diseases, disabilities, and death — yet millions of people in the United States don't get recommended preventive health care services. Healthy People 2030 focuses on increasing preventive care for people of all ages.
Which activity is included in preventative health care?
Examples include immunization against disease, maintaining a healthy diet and exercise regimen, and avoiding smoking. Methods to detect and address an existing disease prior to the appearance of symptoms. Examples include treatment of hypertension (a risk factor for many cardiovascular diseases), and cancer screenings.
What is preventive services in medical billing?
Routine health care that includes screenings, check-ups, and patient counseling to prevent illnesses, disease, or other health problems.
What does Medicare consider preventive services?
Preventive services include exams, shots, lab tests, and screenings. They also include programs for health monitoring, and counseling and education to help you take care of your own health. If you have Medicare Part B (Medical Insurance), you can get a yearly “Wellness” visit and many other covered preventive services.
Can Specialist bill for preventive care?
It would be unusual for an specialist to bill for a preventative visit when she all ready has the disease the physician is managing. If the intent of the visit is for follow up (Cheif Complaint) for a current disease i.e. hypothyroidism, it cannot be billed as a preventative visit.
When should you Bill preventive visit with office visit?
Here's some quick guidance from CPT: If a new or existing problem is addressed at the time of a preventive service and is significant enough to require additional work to perform the key components of a problem-oriented evaluation and management (E/M) service, you should bill for both services with modifier 25 attached ...
What is included in CPT 99395?
99395- Periodic comprehensive preventive medicine reevaluation and management of an individual including an age and gender appropriate history, examination, counseling/anticipatory guidance/risk factor reduction interventions, and the ordering of laboratory/diagnostic procedures, established patient; 18-39 years.
What are some examples of preventive care?
Preventive CareBlood pressure, diabetes, and cholesterol tests.Many cancer screenings, including mammograms and colonoscopies.Counseling on such topics as quitting smoking, losing weight, eating healthfully, treating depression, and reducing alcohol use.Regular well-baby and well-child visits.More items...
What is the difference between office visit and preventive care?
The questions and exam will focus on the problems discussed. This is different from preventative care. Hence, if you schedule a physical but your appointment is spent on specific health issues or problem(s), we can no longer bill this as a physical, but instead, as a problem-focused “office visit”.
What is CPT code?
Preventive Service Codes. The American Medical Association’s (AMA) CPT® code set describes the annual preventive exam as a periodic, comprehensive preventive medicine evaluation (or reevaluation) and management of a patient.
Is preventive medicine comprehensive?
A preventive medicine service is comprehensive in nature; however, the “comprehensive” nature of these services should not be confused with the comprehensive examination requirements in other E/M codes.#N#When determining if the physician or other qualified healthcare provider’s documentation supports a preventive medicine CPT® code, the question of how these services should be documented inevitably comes up, along with many other questions:
Why is preventive care important?
Getting preventive care reduces the risk for diseases, disabilities, and death — yet millions of people in the United States don’t get recommended preventive health care services.1 Healthy People 2030 focuses on increasing preventive care for people of all ages.
What are the barriers to preventive care?
Barriers include cost, not having a primary care provider, living too far from providers, and lack of awareness about recommended preventive services. 4, 5. Teaching people about the importance of preventive care is key to making sure more people get recommended services.
What are physician reports dominated by?
Physician reports are dominated by breakdowns in information transfer and ultimate treatment errors, 12, 13 whereas our results suggest that patients cite problems of access and relationship, which are dominated by psychological injuries.
How to build a safer health system?
The report by the Institute of Medicine To Err is Human: Building a Safer Health System 1 focused public attention on the problem of medical error. It also stimulated policy makers to devote new resources to characterize and prevent medical errors across the spectrum of health care. Much of the effort to date focuses on improving patient safety in hospitals, an appropriate priority given the suggested incidence of errors in inpatient settings, 2– 4 the resulting anxiety engendered in the public sector, 5 and the opportunities for system redesign that can reduce the risk for errors and harms. 6 Yet most medical care occurs in ambulatory settings provided by primary care clinicians. 7, 8
About the journal
Preventive Medicine Reports is the open access companion journal to Preventive Medicine. While Preventive Medicine focuses on publishing articles that appeal more broadly to the preventive medicine and health promotion communities, Preventive Medicine Reports publishes papers that have a …
Metrics
The average number of weeks it takes to reach from manuscript acceptance to the first appearance of the article online (with DOI).
Partner journals
Founded in 1972 by Ernst Wynder, Preventive Medicine is an international scholarly journal that publishes original articles on the science and practice of disease prevention, health promotion, and public health policymaking. Preventive Medicine aims to reward innovation. It will favor insightful …
Preventive Medicine Reports is a companion journal to Preventive Medicine
Founded in 1972 by Ernst Wynder, Preventive Medicine is an international scholarly journal that publishes original articles on the science a …
Authorship
The primary corresponding authors at country/region level in the last five years.
Author Resources
Whether you are planning a research project or working on your next manuscript, Elsevier's author resources are there to help.
Your Research Data
Make your research data available, accessible, discoverable, and usable.
Why are patient reports important?
Why Patient Reports Are Needed. Patient medical reports serve as evidences that the patient has been given proper medications or treatments. Doctors or physicians are doing the best they could in order to supply the needs of each and every patient, regardless if they are in a critical condition or not.
What is the relevant information needed for a patient complaint?
In a patient complaint, the relevant information that are needed are as follows: The description of the situation. The effect on privacy.
What is healthcare personnel?
Healthcare personnel in hospitals or medical centers ensure that they provide the needs of the patients (pertaining to the treatments or medications needed) and their individual relatives (pertaining to the answers or provision of exact details from the medical results). It goes without saying that everyone wants an accurate general information ...
What to do if you happen to be a relative of an injured person?
As the relative. If in case that you happened to be a relative of the injured person, the first thing to do is to calm down.
What to do if you don't have first aid experience?
If in case that you do not have a first aid experience, contact someone who has. Do not act like you know what to do. If immediate response is needed, call for some immediate help from the hospital release or the police. Do not ask help from those people who do not have the capabilities to help.
Do hospitals keep records of patients?
Therefore, it is mandatory that the medical clinic, center, or hospital keeps a record of their patients. These patient reports also help the doctors and the relatives of the patient to know what is or are behind the patients’ results of their individual health assessment.
Can results from medical assessments be given due to deficiency of relevant information?
Otherwise, results from medical assessments cannot be given due to deficiency of relevant information.
Why do we use resolved patient incident reports?
Using resolved patient incident reports to train new staff helps prepare them for real situations that could occur in the facility. Similarly, current staff can review old reports to learn from their own or others’ mistakes and keep more incidents from occurring. Legal evidence.
How long after incident should you report a patient?
Patient incident reports should be completed no more than 24 to 48 hours after the incident occurred. You may even want to file the report by the end of your shift to ensure you remember all the incident’s important details. RELATED: Near Miss Reporting: Why It’s Important.
Why is it important to review patient incidents?
Reviewing incidents helps administrators know what risk factors need to be corrected within their facilities , reducing the chance of similar incidents in the future.
Why is it important to know that an incident has occurred?
Knowing that an incident has occurred can push administrators to correct factors that contributed to the incident. This reduces the risk of similar incidents in the future. Quality control. Medical facilities want to provide the best care and customer service possible.
Why choose a platform that is web-enabled for quick reporting?
You’ll never miss important details of a patient incident because you can file your report right at the scene. A platform with HIPAA-compliant forms built in makes your workflow more efficient and productive, ensuring patient incidents are dealt with properly.
What to include in an incident report?
Every facility has different needs, but your incident report form could include: 1 Date, time and location of the incident 2 Name and address of the facility where the incident occurred 3 Names of the patient and any other affected individuals 4 Names and roles of witnesses 5 Incident type and details, written in a chronological format 6 Details and total cost of injury and/or damage 7 Name of doctor who was notified 8 Suggestions for corrective action
How long does it take to file a patient incident report?
Patient incident reports should be completed no more than 24 to 48 hours after the incident occurred.
Popular Posts:
- 1. patient portal united healthcare
- 2. palo alto medical foundation patient login
- 3. cchit patient portal engagement
- 4. case report consent of patient
- 5. aegis patient portal covid
- 6. dr william farrar patient portal
- 7. mount sinai drs long island patient portal
- 8. mayo health patient portal
- 9. patient pht report study diary
- 10. redwood dental patient portal