Best Practices of Postpartum Discharge Teaching
15 hours ago Observe and ask the patient to report any signs of fever such as chills and elevated body temperature, body pain, inability to eat, pelvic pain, and uterine tenderness. If left untreated, these symptoms indicate systemic involvement, which could result in bacteremia, shock , … >> Go To The Portal
What is postpartum teaching and why is it important?
Postpartum teaching is an essential aspect of nursing care during the hospital stay following childbirth.
What do I need to know about postpartum care?
The woman would also need a postpartum course such as her activity level after birth, any difficulties or pain felt, and if she is successful with infant feeding to determine any need for anticipatory guidance in home care.
How can I prepare for my postpartum checkup?
Refer to the discharge instructions from your physician or call your doctor’s office. Good nutrition and adequate fluids are necessary for tissue repair, healing, breastfeeding and general health. Refrain from any weight-reducing diets until after your postpartum checkup. Most women lose eight to 10 pounds just from delivery.
Why integrate postpartum discharge teaching into the prenatal plan of care?
It is recommended to integrate postpartum discharge teaching into the prenatal plan of care to ensure the opportunity for repetition and retention of important information. It is also critical to identify patient challenges early on and prepare for them in advance.

What should I report postpartum?
Life-threatening conditions that can happen after giving birth include infections, blood clots, postpartum depression and postpartum hemorrhage. Warning signs to watch out for include chest pain, trouble breathing, heavy bleeding, severe headache and extreme pain.
What do you monitor in postpartum?
The comprehensive postpartum visit should include a full assessment of physical, social, and psychological well-being, including the following domains: mood and emotional well-being; infant care and feeding; sexuality, contraception, and birth spacing; sleep and fatigue; physical recovery from birth; chronic disease ...
Which of the following would you emphasize in the teaching plan for a postpartum woman who is reluctant to begin taking warm sitz baths?
Which information would the nurse emphasize in the teaching plan for a postpartal woman who is reluctant to begin taking warm sitz baths? Sitz baths increase the blood supply to the perineal area.
Which of the following findings would be expected when assessing the postpartum client?
Which of the following findings would be expected when assessing the postpartum client? Fundus 1 cm above the umbilicus 1 hour postpartum. Within the first 12 hours postpartum, the fundus usually is approximately 1 cm above the umbilicus. The fundus should be below the umbilicus by PP day 3.
What assessments are vital for the nurse to perform on the postpartum patient?
BREASTS. The breasts are assessed for: ... UTERUS. The fundus is assessed for: ... BOWEL. Assessment of the bowel is important in all postpartum patients. ... BLADDER. Assessment of urination and bladder function includes: ... LOCHIA. ... EPISIOTOMY/PERINEUM. ... LOWER EXTREMITIES. ... CESAREAN SECTION ISSUES.More items...
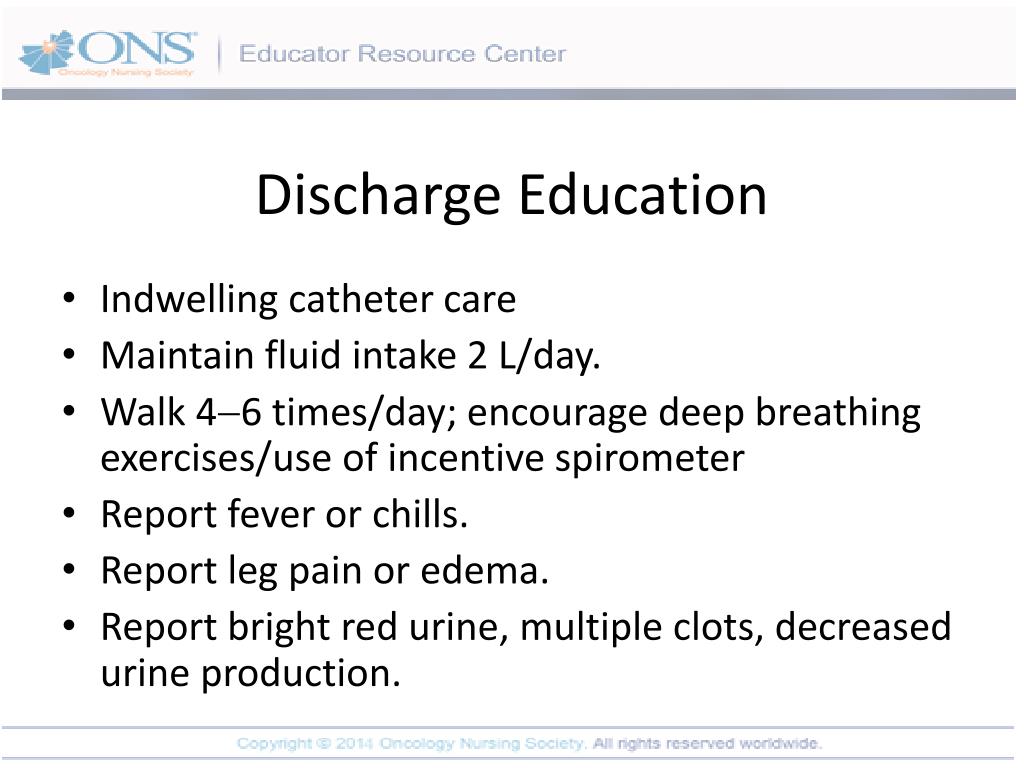
Which information would the nurse include in the discharge teaching of a postpartum client?
Which information should the nurse include in the discharge teaching of a postpartum client? Exercises may be resumed immediately and should be done for the rest of the life because they help strengthen the muscle needed for urinary continence and may inhance sexual intercourse.
Which information should the nurse include in the teaching plan for a Primiparous client who asks about weaning her neonate?
Which information should the nurse include in the teaching plan for a primiparous client who asks about weaning her neonate? "Gradually eliminate one feeding at a time."
What are your nursing responsibility during the first hour of post partum period?
Care within the First 24 Hours Assess the labor and birth history such as the length of labor and if any analgesia or anesthesia was used to determine any necessary procedures to be done. Determine the infant's data and profile to help with planning the care of the newborn and promote bonding between the parents.
Which assessment on the third postpartum day would make the nurse evaluate a woman as having uterine Subinvolution?
Which assessment on the third postpartal day would make the nurse evaluate a woman as having uterine subinvolution? Her uterus is at the level of the umbilicus.
How do you do a postpartum assessment?
10:2520:07POSTPARTUM HEAD TO TOE ASSESSMENT/BUBBLE HEYouTubeStart of suggested clipEnd of suggested clipIf there's not a lot of blood on your pad you should still change your pad every two to three hoursMoreIf there's not a lot of blood on your pad you should still change your pad every two to three hours just like going to the bathroom. Postpartum. Women are at high risk for infection.
Which physical signs and symptoms might the postpartum patient experience following delivery?
Most new moms experience postpartum "baby blues" after childbirth, which commonly include mood swings, crying spells, anxiety and difficulty sleeping. Baby blues typically begin within the first two to three days after delivery, and may last for up to two weeks.
Which nursing action is needed when preparing for assessment of the fundus of a postpartum client?
Which nursing action is needed when preparing for assessment of the fundus of a postpartum client? Ask the client to urinate and empty her bladder.
What are the two methods used by nurses?
The two methods used by the nurses were (a) the traditional method (defined as one-to-one teaching between the nurse and new mother) and (b) a group discharge class (three or more new mothers taught by an experienced mother–baby nurse).
What is the satisfaction of nursing care?
One of the key attributes of satisfaction with nursing care is the provision of adequate patient education. Postpartum discharge planning begins from the moment a laboring woman is admitted to the hospital to birth her baby, as nurses assess her knowledge and identify areas of teaching appropriate for her.
What is the purpose of individual instruction after postpartum?
Individual instruction is also sought after postpartum, as the family will need to know how to care for the woman and the newborn after discharge. Teaching should not always be formal; it may come in the form of comments during classes or procedures.
When to assess pregnancy history?
Pregnancy history is assessed during the postpartum visit and if there are any difficulty with the bonding between the mother and the baby, and allow the woman to relate her labor and birth experiences. Assess the newborn history and if there are any concerns about the newborn that the woman has noticed.
What is home visit after discharge?
A home visit after the discharge is usually recommended to check on how the family is doing now that they have a newborn in the house. High-risk newborns, newborns born to adolescent mothers, and newborns with mothers who have abused drugs during pregnancy need to have a specially planned discharge and home visit.
Why is it important to make sure that the woman is in a stable condition after giving birth?
It is also essential to make sure that the woman is in a stable condition because the immediate postpartum is a critical stage for both the woman and her baby.
How long after discharge should you visit?
Calling or visiting 24 hours after discharge is the best way to evaluate whether the family has been able to grasp all instructions and integrate the newborn into the family.
How long after birth should you check on a newborn?
Remind the mother about the health maintenance visit of the newborn once she reaches 2 to 4 weeks old, and her return checkup 4 to 6 weeks after birth.
Why is it important for a woman to rest at home?
The woman can rest better at home and may eat better if she has cultural preferences regarding food. The newborn can also be exposed earlier to the routines of the family, and make it easier for her to adjust to extrauterine environment.
How to recover from a postpartum checkup?
Good nutrition and adequate fluids are necessary for tissue repair, healing, breastfeeding and general health. Refrain from any weight-reducing diets until after your postpartum checkup. Most women lose eight to 10 pounds just from delivery. It takes almost a full year to return to your pre-pregnancy weight. If you are breastfeeding, continue to take your prenatal vitamins. Eat a well-balanced diet that is high in protein (meat, fish, legumes), fiber (fruits, vegetables, whole grains), calcium (milk, yogurt, cheese, green leafy vegetables) and fluids. If you have a family history of food allergies or are concerned about food allergies for your baby while breastfeeding, consult your physician for guidance.
What to take if you are breastfeeding?
If you are breastfeeding, continue to take your prenatal vitamins. Eat a well-balanced diet that is high in protein (meat, fish, legumes), fiber (fruits, vegetables, whole grains), calcium (milk, yogurt, cheese, green leafy vegetables) and fluids.
How long does it take for bowel movements to return after delivery?
Often mothers fear tearing their stitches or experiencing pain. Bowel function should return to normal three to four days after delivery. A diet high in fiber and fluids can help avoid constipation. Walking promotes bowel movements, passing gas and increased general circulation. Raising your feet onto a stool during a bowel movement can help decrease straining. For constipation, take an over-the-counter stool softener (Colace, Metamucil) or add prunes, prune juice or bran to your diet. If you have additional questions, please contact your doctor’s office.
How to get rid of a swollen intestine after delivery?
Start Kegel exercises immediately after delivery. This movement is similar to stopping the flow of urine. Squeeze for three seconds and release. Begin with 10 repetitions twice a day, gradually building up to 100 repetitions twice a day.
What are the benefits of exercise for babies?
The benefits of exercise include improved muscle tone, quicker healing and a more positive attitude. Fresh air and sunshine are refreshing for both you and your baby. Avoid heavy lifting, strenuous exercise and excessive stair climbing.
How to adjust to a new baby?
Other ways you and your family can adjust to a new baby are: 1 Rest/sleep when the baby sleeps. 2 Eat a well-balanced diet. Now is not the time for dieting or junk food. 3 Be flexible. It takes time to get to know your baby. 4 Let others help you. Accept offers to bring dinner, go to the market or do other necessary chores. 5 Spend special time with your other children and your partner. A new baby is an adjustment for them as well. 6 If you have other young children, put together a box/basket of age-appropriate special snacks, toys and activities that only comes out when you are feeding the baby. Make sure to include a book so you can all read together while the baby is being fed. 7 Talk to other parents who are going through some of the same experiences.
Can you take medication while breastfeeding?
Neither of these conditions reflects your feelings for your baby, your partner or your abilities as a mother. You cannot control these feelings, but they can be helped. There are medications that are safe to take while breastfeeding. Postpartum Support International: www.postpartum.net, 1-800-944-4PPD.
Why do women have postpartum depression?
Some women never experience it, but most do to some degree. Some reasons for it are anxiety and confusion over parenting, tiredness, engorged breasts, sore nipples, hormonal fluctuations, and lack of sleep.
What temperature should a bra be for breast feeding?
If an area develops on your breast that is tender, firm and reddened, especially if your temperature is over 100.5°F, call the office immediately.
What to do if you have no bowel movement?
If you have not had a bowel movement within a couple of days after leaving the hospital, you may want to use a mild laxative. If you are breast feeding, stool softeners, milk of magnesia, or a bulk agent like Metamucil are fine as they are not absorbed by your body and will not pass to your baby.
How to know if you have a period?
There are important signs and symptoms to watch for during the postpartum period. If any of the following occur, call the office right away: 1 Temperature greater than 100.5°F. 2 Pelvic pain greater than after-birth pains or menstrual cramps. 3 Any bleeding greater than a heavy period. Initially you may pass clots or bleed somewhat heavily for a few days, but it should not continue. It is rare, but postpartum hemorrhage can occur even weeks after delivery. If at any time you experience a reoccurrence of heavy bleeding, call the office immediately.
What is the best diet for breast feeding?
A healthy diet contains less red meat and more fish, poultry, and other lean meats. If you are breast-feeding all of the above apply with some additions. You need extra protein and dairy products, and prenatal vitamins with iron until you wean your baby.
How long does it take for a woman to get back to work after a baby?
Some women are back to full activity within one or two weeks, and others need six weeks. We hope these general guidelines will help. A new mother should resume her routine when it feels right. The only limitations are: No heavy lifting for two weeks to two months.
Can you bleed after delivery?
Initially you may pass clots or bleed somewhat heavily for a few days, but it should not continue. It is rare, but postpartum hemorrhage can occur even weeks after delivery. If at any time you experience a reoccurrence of heavy bleeding, call the office immediately.
What are the basic needs of a newborn?
Achieving even the most basic needs – eating and drinking healthfully – can be challenging when caring for a newborn. Holding, feeding, burping, rocking, changing, and swaddling leave little time to cook.
Is feeding a baby a full time job?
Feeding a new baby can be a full-time job. The initial days can be especially challenging as parents and baby figure out what works. Feeding choices – breast, bottle, or both -- do not have to be exclusive, nor do they need to be permanent. Some parents prefer one technique; others choose a hybrid-approach --
Popular Posts:
- 1. western md &ealth system patient portal
- 2. st louise clinic patient portal
- 3. health quest patient portal pet scan
- 4. dr lois carani patient portal
- 5. windsong radiology patient portal login
- 6. keystone family clinic patient portal
- 7. mt kison medical group patient portal
- 8. st marrys patient portal
- 9. dr mainero patient portal
- 10. yvmh patient portal