AORN Guidelines for Perioperative Practice - AORN
18 hours ago AORN’s Guidelines for Perioperative Practice are the gold-standard in evidence-based recommendations to deliver safe perioperative patient care and achieve workplace safety. Developed by an interdisciplinary panel of clinical experts, and approved by the ECRI Guideline Trust, they will help decrease surgical errors, provide quality measurements, and keep your … >> Go To The Portal
Three general themes were found to be important for perioperative nurses' documentation practices: (1) the documentation tool must be adapted to the clinical practice; (2) nurses document to improve patient safety and protect themselves legally; and (3) traditions and conditions for documentation. Conclusion:
Full Answer
What is included in a perioperative risk assessment?
This includes preoperative risk assessment and cardiovascular testing, as well as (when indicated) perioperative pharmacological (including anesthetic) management and perioperative monitoring that includes devices and biochemical markers. This CPG is intended to inform all the medical professionals involved in the care of these patients.
Are there recommendations for perioperative cardiovascular evaluation and management for noncardiac surgery?
Current recommendations for perioperative cardiovascular evaluation and management for noncardiac surgery are based largely on clinical experience and observational studies, with few prospective RCTs.
Does hospital volume affect Perioperative Safety after bariatric surgery?
The benefits and safety with the use of an ERAS protocol have been shown after all of the most common bariatric surgeries [ 5, 194 ]. There are limited data on the effect of hospital volume on perioperative safety in an ERAS environment [ 197 ].
What is the OTN's experience of responsibility in Perioperative Practice?
RESULTS The results revealed the OTN's experiences of responsibility for patient's care in perioperative practice as two main themes: “the formal external responsibility” and “personal ethical value”.
What are the important components of preoperative patient evaluation?
A history and physical examination, focusing on risk factors for cardiac and pulmonary complications and a determination of the patient's functional capacity, are essential to any preoperative evaluation.
What is OSA protocol?
Positive airway pressure (PAP) treatment is recommended for severe OSA and symptomatic mild-to-moderate OSA. Individuals with OSA should use PAP treatment at all times when sleeping. PAP treatment should be continued even if usage is less than 4 hours a night.
When is preoperative EN indicated?
A preoperative complete blood count is indicated for patients at risk of anemia based on their history and physical examination findings, and those in whom significant perioperative blood loss is anticipated.
What is a pre anesthesia evaluation?
A pre-anesthesia evaluation is conducted to assess the risks and develop the plan for anesthesia. This evaluation specifically identifies the risks of the anesthesia encounter and is the sole purview of an anesthesia professional.
How do you read CPAP data?
0:332:31Air rotate the control wheel to highlight info and press down on the control wheel to select infoMoreAir rotate the control wheel to highlight info and press down on the control wheel to select info rotate the control wheel to highlight compliance v.i.c.
When is CPAP indicated?
All patients with an apnea-hypopnea index (AHI) greater than 15 are considered eligible for CPAP, regardless of symptomatology. For patients with an AHI of 5-14.9, CPAP is indicated only if the patient has one of the following: excessive daytime sleepiness (EDS), hypertension, or cardiovascular disease.
What is pre-operative assessment of a patient?
The pre-operative assessment is an opportunity to identify co-morbidities that may lead to patient complications during the anaesthetic, surgical, or post-operative period. Patients scheduled for elective procedures will generally attend a pre-operative assessment 2-4 weeks before the date of their surgery.
What is the difference between preoperative and perioperative?
The word “perioperative” is used to encom- pass all three phases. The perioperative nurse provides nursing care during all three phases. 2. The preoperative phase begins when the patient, or someone acting on the patient's behalf, is informed of the need for surgery and makes the decision to have the procedure.
What is preoperative checklist?
What is pre-verification checklist? It is a checklist that is required to be asked and assessed as part of your safe care before going for surgery. What will I expect? Your nurse in the Preoperative Holding or Prep area on the day of surgery will make sure that all your requirements are done before surgery.
What are the steps in pre operative preparation?
The preoperative preparations include the following:Medical history and physical examination. ... Laboratory tests. ... Blood type and crossmatch. ... Chest x-ray. ... Electrocardiogram (ECG). ... Diagnostic procedures. ... Written instructions. ... Informed consent.More items...•
Why is pre operative assessment important?
Preoperative tests give your nurse or doctor more information about: whether you have any medical problems that might need to be treated before surgery. whether you might need special care during or after surgery. the risk of anything going wrong, so that they can talk to you about these risks.
What is pre operative nursing care?
Preoperative care: Care given before surgery when physical and psychological preparations are made for the operation, according to the individual needs of the patient. The preoperative period runs from the time the patient is admitted to the hospital or surgicenter to the time that the surgery begins.
Standardize Your Clinical Practice
AORN’s Guidelines for Perioperative Practice provide a standardized perioperative foundation to help deliver safe patient care and achieve workplace safety.
Guidelines
Guidelines for Perioperative Practice provide evidence-based recommendations to deliver safe perioperative patient care and achieve workplace safety.
Clinical Resources
AORN’s clinical resources will help your entire system manage daily clinical issues and improve educational efforts for better long-term patient outcomes.
What is regional analgesic?
Regional analgesic techniques should be considered to reduce or eliminate the requirement for systemic opioids in patients at increased perioperative risk from OSA. If neuraxial analgesia is planned, weigh the benefits (improved analgesia, decreased need for systemic opioids) and risks (respiratory depression from rostral spread) of using an opioid or opioid–local anes-thetic mixture rather than a local anesthetic alone. If patient-controlled systemic opioids are used, continuous background infusions should be avoided or used with extreme caution. To reduce opioid requirements, nonsteroidal antiinflammatory agents and other modalities (e.g., ice, transcutaneous electrical nerve stimulation) should be considered if appropriate. Cli-nicians are cautioned that the concurrent administration of
What is preoperative preparation?
Preoperative preparation is intended to improve or optimize an OSA patient’s perioperative physical status and includes (1) preoperative continuous positive airway pressure (CPAP) or noninvasive positive pressure ventilation (NIPPV), (2) preoperative use of mandibular advancement or oral appli-ances, and (3) preoperative weight loss.
What is open forum testimony?
Open-forum testimony obtained during development of the original Guidelines, Internet-based comments, letters, and editorials are all informally evaluated and discussed during the formulation of Guideline recommendations. When war-ranted, the Task Force may add educational information or cautionary notes based on this information.
What is the purpose of the OSA guidelines?
The purposes of these Guidelines are to improve the peri-operative care and reduce the risk of adverse outcomes in patients with confirmed or suspected OSA who receive seda-tion , analgesia , or anesthesia for diagnostic or therapeutic procedures under the care of an anesthesiologist.
What is a preoperative treatment for sleep apnea?
Preoperative treatment/optimization for obstructive sleep apnea (e.g., continuous positive airway pressure [CPAP], noninvasive positive pressure ventilation, mandibular appliances, and medical treatment)Consult the American Society of Anesthesiologists “Practice Guidelines for Management of the Dicult Airway”Limit procedures to facilities with full hospital services
What factors determine whether OSA is inpatient or outpatient?
Factors to be considered in determining whether outpatient care is appropriate include (1) sleep apnea status, (2) anatomical and physiologic abnormalities, (3) status of coexisting diseases, (4) nature of surgery, (5) type of anesthesia, (6) need for postop-erative opioids, (7) patient age, (8) adequacy of postdischarge observation, and (9) capabilities of the outpatient facility. The availability of emergency dicult airway equipment, respira-tory care equipment, radiology facilities, clinical laboratory facilities, and a transfer agreement with an inpatient facility should be considered in making this determination.
What are the guidelines for perioperative management of OSA?
These Guidelines do not focus on patients with the following conditions: (1) pure central sleep apnea, (2) abnormalities of the upper or lower airway not associated with sleep apnea (e.g., deviated nasal septum), (3) daytime hyper-somnolence from other causes, (4) patients younger than 1 yr, and (5) obesity in the absence of sleep apnea.
What is a CPG in perioperative care?
The focus of this CPG is the perioperative cardiovascular evaluation and management of the adult patient undergoing noncardiac surgery. This includes preoperative risk assessment and cardiovascular testing, as well as (when indicated) perioperative pharmacological (including anesthetic) management and perioperative monitoring that includes devices and biochemical markers. This CPG is intended to inform all the medical professionals involved in the care of these patients. The preoperative evaluation of the patient undergoing noncardiac surgery can be performed for multiple purposes, including 1) assessment of perioperative risk (which can be used to inform the decision to proceed or the choice of surgery and which includes the patient’s perspective), 2) determination of the need for changes in management, and 3) identification of cardiovascular conditions or risk factors requiring longer-term management. Changes in management can include the decision to change medical therapies, the decision to perform further cardiovascular interventions, or recommendations about postoperative monitoring. This may lead to recommendations and discussions with the perioperative team about the optimal location and timing of surgery (eg, ambulatory surgery center versus outpatient hospital, or inpatient admission) or alternative strategies.
What are the recommendations for perioperative cardiovascular evaluation and management for noncardiac surgery?
Current recommendations for perioperative cardiovascular evaluation and management for noncardiac surgery are based largely on clinical experience and observational studies, with few prospective RCTs. The GWC recommends that future research on perioperative evaluation and management span the spectrum from RCTs to regional and national registries to focus on patient outcomes. Development and participation in registries (such as the American College of Surgeons NSQIP, American Society of Anesthesiologists, and NACOR [National Anesthesia Clinical Outcomes Registry]) for patients undergoing noncardiac surgery will advance knowledge in the following areas:
How long after DES implantation can you have elective surgery?
Elective noncardiac surgery after DES implantation may be considered after 180 days if the risk of further delay is greater than the expected risks of ischemia and stent thrombosis.234,238(Level of Evidence: B)
How long after balloon angioplasty can you have elective surgery?
Elective noncardiac surgery should be delayed 14 days after balloon angioplasty (Level of Evidence: C) and 30 days after BMS implantation.231–233(Level of Evidence B)#N#Elective noncardiac surgery should optimally be delayed 365 days after drug-eluting stent (DES) implantation.234–237(Level of Evidence: B)
When to use hemodynamic assist devices?
Use of hemodynamic assist devices may be considered when urgent or emergency noncardiac surgery is required in the setting of acute severe cardiac dysfunction (ie, acute MI, cardiogenic shock) that cannot be corrected before surgery. (Level of Evidence: C)
How long before surgery should you start beta blockers?
In patients in whom beta-blocker therapy is initiated, it may be reasonable to begin perioperative beta blockers long enough in advance to assess safety and tolerability, preferably more than 1 day before surgery.241,258–260(Level of Evidence: B) SR
What is HF in medical terms?
Patients with clinical heart failure (HF) (active HF symptoms or physical examination findings of peripheral edema, jugular venous distention, rales, third heart sound, or chest x-ray with pulmonary vascular redistribution or pulmonary edema) or a history of HF are at significant risk for perioperative complications, and widely used indices of cardiac risk include HF as an independent prognostic variable. 37, 48, 49
Introduction
- Perioperative management consists of preoperative patient evaluation as well as intraoperative and postoperative patient monitoring and care. The perioperative period is the time period of a patient’s surgical procedure.
Components of Perioperative Care
- Peri-operative Care consists of: 1. Pre-operative care 2. Intra-operative care 3. Post-operative care Perioperative care is targeted at ensuring that the patient is fit for anaesthesia and intended surgical procedure, as well as prevent complications after surgery. The focus on peri-operative care is based on the evidence that majority of complications and mortality following elective sur…
Goals of Perioperative Care
- The goals of peri-operative care include: 1. Prevent avoidable complications 2. Ensure early identification of complications and prompt treatment 3. Prevent avoidable mortality 4. Ensure quick recovery and return to activities 5. Ensure safe and smooth surgery 6. Ensure optimal patient outcomes
Pre-Operative Care
- The goal is to prevent and/or minimize the risk of adverse cardio-pulmonary events during and after surgery.
Clinical Evaluation
- Efforts should be made to identify the following by history and physical examination Cardiopulmonary disorders: 1. Cough 2. Chest infection 3. Bronchial asthma 4. Chronic obstructive airways disease 5. Hypertension 6. Cardiac failure Metabolic disorders: 1. Diabetes mellitus Haematologic disorders: 1. Sickle cell disease Allergy: 1. Drug allergies (e.g. penicillins, …
Investigations
- Cardiopulmonary: 1. Chest radiograph: especially for patients 60 years and above, and those with chest infection 2. Look for evidence of chest infection and cardiomegaly Electrocardiogram: 1. especially for patients over 60 years and those with heart disease or hypertension Pulmonary function tests may be necessary in patients with obstructive airways disease Metabolic: 1. Urin…
Correction of Abnormalities and Preparation For Surgery
- Cardiopulmonary: 1. Rehydrate patientbadequately, using appropriate fluids 2. Control blood pressure 3. Treat/control chest infections with appropriate antibiotics 4. Control obstructive airways disease Metabolic conditions and derangements: 1. Correct electrolyte deficits, especially hypokalaemia 2. Acidosis is usually corrected by adequate rehydration (provided the patient ha…
Consent For Surgery
- Details of the surgery should always be explained to the patient (or relatives) in very simple language before surgery 1. A signed consent should be obtained, in the presence of a witness (usually a nurse) 2. Obtaining consent should be done by the surgeon himself 3. It should include a mention of the possible/common complications 4. There are a number of evidence-based risk …
Intra-Operative Care
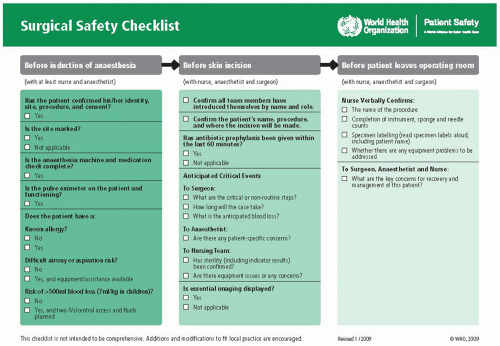
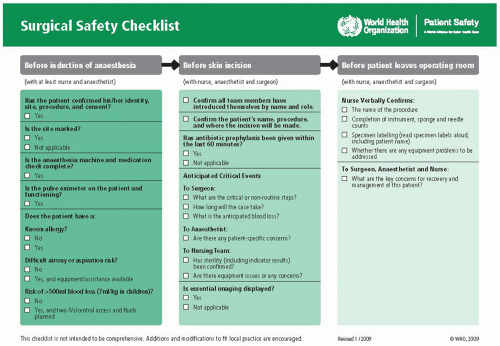
- The focus of intra-operative care is to ensure a safe and smooth surgical procedure. The entire team in the operating room, including surgical team, anaesthesia team and perioperative nursing team, should work together as a team and take responsibility for intra-operative care to ensure a smooth and safe operation. The World Health Organisation’s ‘Surgical Safety Checklist’ is a helpf…
Post-Operative Care
- An excellently performed operation can be marred by poor post-operative care and inadequate attention to patient’s post operative needs. Meticulous and efficient care in the postoperative period is paramount for adequate patient recovery and success of surgery. A well-planned and supervised postoperative care ensures a smooth recovery, and helps to prevent or limit postope…