Possible Causes and Evaluation of a Persistent Cough
26 hours ago · If you smoke or have smoked, chronic cough could be due to a chronic lung condition called COPD (sometimes called emphysema or chronic bronchitis). If you're over 35, have ever smoked and have chronic cough, bring up sputum regularly, get bronchitis in winter, and get wheezy or out of breath, COPD may be to blame. >> Go To The Portal
Chronic cough is a persistent cough lasting eight weeks or more. Many report it to be a dry cough with an irritation or tickling sensation; this is quite common but can be distressing. The cough can be triggered by talking, laughing, certain strong smells/irritants and/or changes in temperature.
Full Answer
What does a persistent cough mean on the NHS?
The NHS website defines a persistent cough as “coughing a lot for more than an hour, or three or more coughing episodes in 24 hours”.
How do you evaluate a patient with chronic cough?
The evaluation of a patient with chronic cough should include an assessment of health status in clinical practice and research. The Leicester Cough Questionnaire is a well validated cough specific quality of life questionnaire that can be used to assess longitudinal changes in patients with chronic cough.
What are the side effects of having a persistent cough?
Annoying effects of coughing, such as loss of sleep, sore chest muscles, and leaking urine can affect your quality of life and interfere with your daily activities. If your cough is lingering, you might also be wondering if it could be something worse than a cold or allergies. What does it mean if you have a cough that just won't go away?
What are the recommendations for the management of cough in adults?
Recommendations for the management of cough in adults. The type of corticosteroid used in a trial and the duration of treatment is unclear; expert opinion is that cough is unlikely to be due to eosinophilic airway inflammation if there is no response to treatment with prednisolone 30 mg/day for 2 weeks.
What do you report about a cough?
In general, call your healthcare provider if you have a cough that will not go away and these symptoms:Wheezing (noise when you breathe out).Fever over 101.5 Fahrenheit or fever that lasts more than a day or two.Chills.Phlegm (thick mucus, also called sputum), especially phlegm that is yellow, green, or bloody.
What is a persistent cough symptoms coronavirus?
A persistent cough is widely known as one of the three 'classic' symptoms of COVID-19, along with fever and loss of smell, although only around four in ten people who are ill with COVID-19 will have a persistent cough. In this context, persistent means coughing many times a day, for half a day or more.
What does a persistent cough indicate?
A persistent cough may be a sign of postnasal drip, acid reflux, asthma or an infection like the common cold, the flu, bronchitis or pneumonia. A cough is considered chronic or persistent when it lasts longer than eight weeks in adults or four weeks in children.
How do you assess a chronic cough?
Diagnostic Evaluation. The patient's history and findings on physical examination provide a basis for the diagnostic evaluation of chronic cough. The physician should question the patient about production of phlegm, character of phlegm produced, exacerbating factors, time relationships, and associated symptoms.
What type of cough is COVID?
A dry cough is one of the most common coronavirus symptoms, but some people may have a cough with phlegm (thick mucus).
Does COVID start with a cough?
Most people with COVID-19 have a dry cough they can feel in their chest.
What causes a persistent dry cough?
Dozens of conditions can cause a recurrent, lingering cough, but the lion's share are caused by just five: postnasal drip, asthma, gastroesophageal reflux disease (GERD), chronic bronchitis, and treatment with ACE inhibitors, used for high blood pressure and heart failure.
When should you worry about a persistent cough?
"If you have a cough that lasts beyond eight weeks, start by consulting your primary care doctor," recommends Dr. Safdar. "He or she can assess your symptoms and work toward identifying the underlying cause of your cough and how best to treat it."
What are the types of cough?
Types of coughs: What do they mean?Dry cough.Wet cough.Whooping cough.Choking.Chronic cough.In children.Seeing a doctor.Summary.
What should I ask a coughing patient?
Chronic CoughHow long have you had the cough?Did your cough start with an illness or a lung infection?Do you cough all of the time, or only during or after activity?Do you cough after meals?What time of the day is your cough the worst?Do you cough up mucus? ... Do you have chest discomfort with your cough?More items...
What characteristics of a cough and sputum should be assessed and documented during data collection?
Patients with sputum production should be asked about its frequency and description of the physical characteristics of the sputum including the amount (with each coughing spell and daily total), color, consistency, ease of its expectoration, taste, and smell.
Why do nurses do respiratory assessments?
As a nurse you need to know optimum respiratory function and be able to recognise signs of deterioration to care for your patient safely. A respiratory assessment is the first step towards identifying if, and how soon, you need a doctor to review your patient, or if you need to make a MET call.
What does a COVID cough feel like?
A common symptom of COVID-19 is a dry cough, which is also known as an unproductive cough (a cough that doesn't produce any phlegm or mucus). Most people with dry cough experience it as a tickle in their throat or as irritation in their lungs.
When should I be concerned about a COVID cough?
If your cough is ongoing and you did not require hospitalisation during your COVID infection you should seek advice from your GP.
When does a COVID cough go away?
An April 2021 study in The Lancet Respiratory Medicine found that cough lasts an average of 19 days for most people with COVID-19 and up to four weeks in about 5 percent of patients.
Can you have a cough without fever with COVID?
A fever is one of the common symptoms of COVID-19, but you can be infected with the coronavirus and have a cough or other symptoms with no fever, or a very low-grade one — especially in the first few days. Keep in mind that it is also possible to have the coronavirus with minimal symptoms or even no symptoms at all.
How many people have a persistent cough?
As many as one in five of us have a persistent cough, which usually doesn't have a serious cause but can be exhausting - especially if it stops us sleeping.
What causes a coughing cough?
Solutions include anti-acid medicine, losing weight, avoiding eating late at night, and not wearing tight belts or trousers. Propping the head of the bed up a bit (with a brick under the top legs) can also help.
Why does my cough get worse at night?
You may also find that your cough gets worse at night - this is because when you're upright during the day, the mucus from your nose trickles down the back of your throat and you swallow it.
How long does it take for a cold to settle?
Most coughs that accompany a cold will settle in one to two weeks. It's not uncommon to be infected with more than one virus at the same time, so symptoms may overlap and last longer from start to finish. They're almost all caused by viruses, so antibiotics don't do any good at all. In fact, we can't 'cure' them, but there are a lot of things that you can do to help relieve the symptoms.
What are the symptoms of heart failure?
Other pointers to heart failure include shortness of breath on exercise or lying flat; swollen ankles and waking up in the night gasping for breath. The outcome for heart failure patients has improved dramatically in recent years with the advent of new medical treatments.
How to diagnose COPD?
It can be diagnosed easily by a test called spirometry, which involves blowing into a special machine.
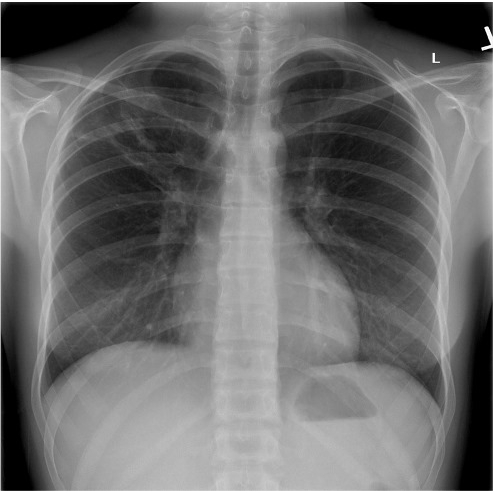
How long does it take to get a chest X-ray?
They recommend you should have a chest X-ray within two weeks if you're over 40 and have two symptoms out of cough, shortness of breath, tiredness, chest pain, weight loss or loss of appetite. If you're over 40 and have ever smoked, just one of these symptoms should trigger a referral for chest X-ray.
Who should evaluate cough?
Anyone with a persistent cough should be evaluated by a health care provider.
How long does a cough last?
The long-lasting cough does not mean your infection is still active. After the infection has cleared, your airways can remain irritated during the healing process. The cough (and wheeze) should resolve within a couple months. Sometimes it will last even longer.
What causes a cough that lasts 3 weeks?
Less often, the initial problem was a bacterial infection, such as pertussis (whooping cough) or mycoplasma. In the later stages of one of these bacterial infections, antibiotics are not usually very helpful. If your cough has already lasted 3 weeks or more, contact your doctor.
What does it mean when you cough without wheezing?
Doctors often refer to this persistent cough (with or without wheezing) as "temporary asthma" or "asthmatic bronchitis.". Usually a cough that persists following an upper respiratory illness starts as a viral infection. The long-lasting cough does not mean your infection is still active.
What is the best way to treat chronic bronchitis?
COPD can include chronic bronchitis (airway damage), emphysema (air sac damage), or both problems. The best way to treat chronic bronchitis is to quit smoking.
How to diagnose asthma?
In order to diagnose asthma, your doctor may want to do a breathing test to measure how well you move air through your airways. These tests are named "spirometry" tests.
What causes a coughing cough?
Sometimes bronchitis or other upper respiratory infections result in a long-lasting cough.
What causes a longer lasting cough?
Other infections which may cause a longer-lasting cough, such as tuberculosis (TB).
How long does a subacute cough last?
Subacute, if it lasts for three to eight weeks. Chronic, meaning it lasts for longer than eight weeks. Cough affects us all if we need to clear our airways. Acute cough usually improves after one week. The most common cause is a viral infection which causes a runny nose and cough. Viral infections can affect anyone.
How to get rid of a cough from viral infection?
For acute coughs due to viral infections, simple remedies may be all that is needed. This might include inhaling steam, or honey and lemon to soothe your throat. If you feel unwell with a temperature or aches and pains, paracetamol or ibuprofen may help. The cough will go away with time on its own.
Why do I cough at night?
These conditions may be caused by infection with germs ( viruses, bacteria or fungi). Asthma. This causes wheeze, breathlessness and cough at night, in cold air and during exercise. An infection with a germ can make symptoms of asthma much worse. This is called an exacerbation of asthma.
How to stop coughing from smoking?
Don't smoke, or get help to stop smoking, because all common serious causes of chronic cough are more likely to affect smokers. Try to avoid dusty or smoky places. Use your asthma medication as advised. Avoid over-the-counter cough medicines .
What is the condition where air gets trapped outside the lung, inside the chest?
Pneumothorax. In this condition, air gets trapped outside the lung, inside the chest. Bronchiectasis. This is a condition where airways of the lungs are excessively widened and produce extra mucus.
Why does my nose cough?
This includes allergies, hay fever and nasal polyps as well as infections. Acid reflux. Acid in the stomach washes up the food pipe and spills into the airways. Asthma. Undiagnosed or under-treated asthma causes cough.
How long does a cough last?
In children, a cough lasting longer than four weeks is considered chronic. The most common causes in children are respiratory tract infections, asthma, and gastroesophageal reflux disease.
What causes a cough in adults?
The most common causes of chronic cough in adults are upper airway cough syndrome, asthma, and gastroesophageal reflux disease, alone or in combination. If upper airway cough syndrome is suspected, a trial of a decongestant and a first-generation antihistamine is warranted.
What is the evaluation of a chronic cough?
The evaluation of patients with chronic cough should include an assessment of health status and cough severity. Cough visual analogue scores are an alternative to cough specific quality of life questionnaires but are less well validated. (Audit)
Where to find the diagnostic algorithm for chronic cough?
A recommended diagnostic algorithm for the evaluation of an adult with chronic cough is displayed in Appendix 2 ( Parts 1 and 2) available online at http://www.thoraxjnl.com/supplemental.
What is cough due to?
4.4.5 Treatment of cough due to other common respiratory diseases . Cough may be a prominent and debilitating symptom in a number of common respiratory diseases including lower respiratory tract infections (acute tracheobronchitis and pneumonia) COPD, lung cancer, diffuse parenchymal lung disease, and bronchiectasis.
What causes a cough to be troublesome?
Most cases of troublesome cough reflect the presence of an aggravant (asthma, drugs, environmental, gastro‐oesophageal reflux, upper airway pathology) in a susceptible individual.
What is bronchial provocation testing?
Bronchial provocation testing should be performed in patients without a clinically obvious aetiology referred to a respiratory physician with chronic cough and normal spirometry. Bronchoscopy should be undertaken in all patients with chronic cough in whom inhalation of a foreign body is suspected.
What is the primary abnormality of cough?
In chronic cough a heightened cough reflex is the primary abnormality.
How long does a chronic cough last?
Chronic cough is defined as one lasting more than 8 weeks. It is reported by 10–20% of adults, commoner in females and obese. Cough accounts for 10% of respiratory referrals to secondary care. Most patients present with a dry or minimally productive cough.
What are the two most influential guidelines for the management of cough, and particularly CRC?
The two most influential guidelines for the management of cough, and particularly CRC, are: 1) those developed [4]and updated [2]by the ACCP, and 2) those developed by the ERS [3]. The definitions, classification, diagnosis and differential diagnosis, assessment of severity, and management (non-pharmacologic and pharmacologic) are similar in these guidelines, and we refer the reader to the original documents for a detailed description. In this review we focus on the management of CRC of known and unknown origin, describing all available approaches, but highlighting whether or not they are recommended by guidelines.
How common is chronic cough?
The prevalence of chronic cough has been estimated as up to 13% of the general population , and may be associated with significant impairment of quality of life, together with anxiety and depression [7], [8], [9]. This is especially common in patients who undergo numerous consultations and/or unsuccessful therapeutic trials before getting the diagnosis unexplained chronic cough or CRC. Therefore, there is increasing interest in understanding possible mechanisms for these clinical conditions.
What is the effectiveness of outpatient cough physiotherapy?
This study reported a significant reduction in cough frequency and an improvement in cough-related quality of life from the intervention, which consisted of education, counseling, cough control, breathing retraining, and vocal hygiene.
What is cough hypersensitivity?
The European Respiratory Society (ERS) Task Force introduced the term ‘cough hypersensitivity syndrome’ in 2014, and defined it as a ‘clinical syndrome characterized by troublesome coughing triggered by low levels of thermal, mechanical or chemical exposure’ [11]. In pathological conditions, inflammation of central and/or peripheral components of the cough reflex may be triggered by innocuous stimuli resulting in excessive coughing due to neuroinflammation defined as ‘cough reflex hypersensitivity’. Assuming cough hypersensitivity syndrome represents a common mechanism responsible for troublesome persistent cough of known or unknown causes, peripheral and central neural pathways for cough signal and receptors become new target for treatment and may help to understand clinical aspects of ‘difficult to treat cough’.
How long does a cough last?
The initial assessment aims to classify duration and severity of the clinical presentation with guidelines from the American College of Chest Physicians (ACCP) listing three categories based upon duration: acute cough, lasting less than three weeks ; subacute cough, lasting between three and eight weeks; and chronic cough, lasting more than eight weeks [2], [3], [4]. In the acute phase, when life-threating features are present, such as acute worsening of dyspnea, increased sputum production, hemoptysis, fever, and weight loss, management of underlying etiologies is an urgent priority. Sub-acute or chronic cough may become a bothersome symptom that significantly impairs quality of life, sometimes persisting for months or years after treatment.
What is the respiratory response to cough?
Cough is a physiological response to mechanical and chemical stimuli due to irritation of cough receptors located mainly in the epithelium of the upp er and lower respiratory tract s, pericardium, esophagus, diaphragm, and stomach. A complex reflex arc through the vagus, phrenic, and spinal motor nerves to the expiratory musculature generates an inspiratory and forced expiratory effort to clear the airways [1]. Under pathological conditions of known and unknown etiologies, chronic refractory cough (CRC) may become a major medical problem because patients may need to undergo repeated examinations before reaching a diagnosis, and/or try several treatments with sometimes poor symptom control, worsening their quality of life and increasing economic burden.
Where is the csection of respiratory diseases?
cSection of Respiratory Diseases, Department of Medicine, University of Modena and Reggio Emilia, Modena, Italy
What is a persistent cough?
The NHS website defines a persistent cough as “coughing a lot for more than an hour, or three or more coughing episodes in 24 hours”.
Why is the RCGP calling for major improvements to the test and trace system?
The difficulty distinguishing between Covid- and non-Covid-related coughs is one reason why the RCGP is calling for major improvements to the test-and-trace system and for GPs to have access to Covid-19 tests to help differentiate between Covid-19 and other potentially serious conditions in high-risk patients.
Can autumn bugs cause coughing?
Tests are available, even though it is a challenge to get hold of them.”. Yet lots of autumn bugs can also trigger bouts of coughing, and shortages of tests may leave many of those with coughs wondering if it is really necessary to self-isolate.
Can the Guardian see your contact details?
Your contact details are helpful so we can contact you for more information. They will only be seen by the Guardian.
Can you talk when you have a cold?
Also, according to data from the Covid Symptoms Study app, if you have a cough related to a cold, it is unlikely to be so persistent that you cannot talk, keep you awake at night, or be associated with bad headaches and severe fatigue, as Covid-19 often seems to be.
Possible Causes
- There are many possible causes of a persistent cough. Most of the time, treatment can help alleviate the cough so you can sleep better, have more energy, and stop having chest soreness from coughing. Though the most common causes are not usually serious, sometimes a cough c…
When to See Your Healthcare Provider
- It is important to make an appointment with your doctor if you have a cough that persists. You should get immediate medical attention if you experience chest pain, shortness of breath or lightheadedness, or are coughing up blood. Questions you may be asked at your medical visit may include: 1. How long have you been coughing? 2. Has the cough been worsening? 3. Is the coug…
Diagnosis
- Depending on the severity of your cough, your healthcare professional will give you treatment to control your symptoms and make you feel more comfortable. They may also recommend tests to determine the cause. Blood tests may be done to look for any evidence of infection. You may have a chest X-ray or a chest computerized tomography (CT) scan.14If you have symptoms of sinusit…
Treatment
- Treatmentwill depend on the underlying cause, as well as the degree to which your cough is interfering with your day-to-day activities.
A Word from Verywell
- If you have a chronic cough, it is important that you get it checked out. Serious causes, such as cancer, have a better outcome when treatment is started early. Even if your cough is not from a serious cause, you will feel more comfortable—and get better sleep—once it's effectively treated.
Popular Posts:
- 1. northshore hospital patient portal glenview
- 2. pototmac pediatrics patient portal
- 3. columbus regional pediatrics patient portal
- 4. my lg health patient portal
- 5. patient portal problems results
- 6. nkch patient portal sign in
- 7. cloquet memorial hospital patient portal
- 8. arkansas urology patient portal login
- 9. genoa patient portal
- 10. southeaster patient portal