Meaningful Use and the Patient Portal: Patient enrollment, use …
16 hours ago 3 rows · The Centers for Medicare and Medicaid Services (CMS) financial incentives for “meaningful ... >> Go To The Portal
In order to qualify for CMS The Centers for Medicare & Medicaid Services, previously known as the Health Care Financing Administration, is a federal agency within the United States Department of Health and Human Services that administers the Medicare program and works in partnership with state government…Centers for Medicare and Medicaid Services
Full Answer
How do you benefit from your patient portal?
Benefits of the Patient Portal. Communication Exchange. The first and one of the most important benefits of a patient portal is the increase in communication capability. Online Bill Management. Now providers can get more on-time payments and increased revenue with online bill management for patients.
How to get your patients to use your patient portal?
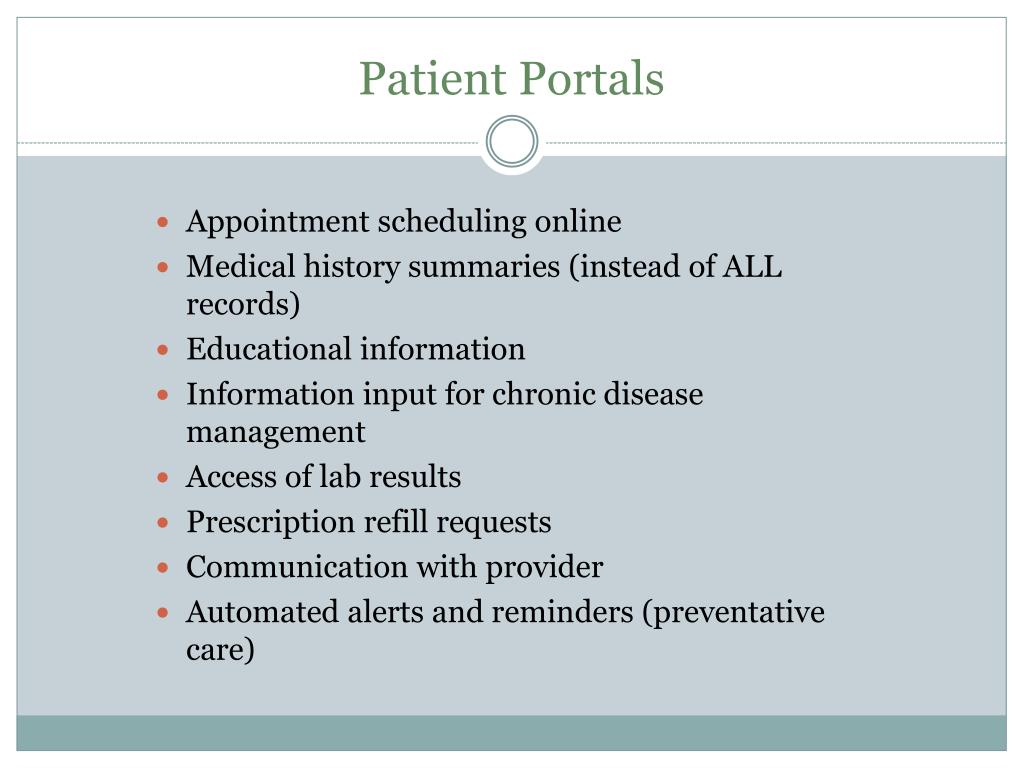
With a patient portal, you can:
- Make appointments (non-urgent)
- Request referrals
- Refill prescriptions
- Check benefits
- Update insurance or contact information
- Make payments to your provider's office
- Complete forms
- Ask questions through secure e-mail
What are the benefits of a patient portal?
eventually benefit the interactive patients engagement accessibility solutions in the market. • Access to the patient portal may improve patient engagement and change the way healthcare is delivered, healthcare improvements are associated with specific ...
What is the value of a patient portal?
Portals can yield actual value for providers by boosting clinical and financial outcomes. They have the potential to drive patient engagement, patient satisfaction, loyalty, retention, and health outcomes. This is how it can be done.

Is meaningful use still in effect 2021?
This question comes up a lot. We've got a simple answer: No, it's not – but the name is. The EHR Incentive Program, commonly known as Meaningful Use (MU), has been considered over or has “died” many times, but it is still around.
What are the 3 stages of meaningful use?
Stages of Meaningful Use The meaningful use objectives will evolve in three stages: Stage 1 (2011-2012): Data capture and sharing. Stage 2 (2014): Advanced clinical processes. Stage 3 (2016): Improved outcomes.
Is meaningful use still in effect 2020?
'Meaningful use' has been replaced with 'advancing care information. ' The US Department of Health and Human Services established three stages to measure use of EHRs in a "meaningful manner": Stage 1 of meaningful use focused on acquiring a baseline of information on patients.
What replaced meaningful use?
Meaningful use will now be called "Promoting Interoperability" as CMS focuses on increasing health information exchange and patient data access.
What are the 5 main objectives of meaningful use?
MIPS Builds on Meaningful Use Improve quality, safety, efficiency, and reduce health disparities. Engage patients and family. Improve care coordination, and population and public health. Maintain privacy and security of patient health information.
What is the meaningful use criteria?
“Meaningful Use Criteria” refers to specific features of an EHR system that providers will be required to utilize in their practice or organization if they are to qualify for the incentives listed in the HITECH Act.
Is CMS meaningful use still in effect?
2015. The Medicare Access and CHIP Reauthorization Act of 2015 (MACRA) was signed into law on April 16, 2015. In October 2015, CMS released the Modifications to Meaningful Use in 2015 through 2017 final rule³, which modified Stage 2 requirements to streamline reporting requirements on measures.
Is meaningful use required?
To fulfill the requirements for Meaningful Use, eligible professionals must successfully complete the 3 main components of the program: 1) use certified EHR, 2) meet core and menu set objectives, and 3) report clinical quality measures.
What is the future of meaningful use?
The reality is that Meaningful Use will continue to exist, as planned, as will the Physician Quality Reporting System (PQRS) and Value-Based Modifier (VBM) program. Healthcare providers and administrators must continue to swim in the alphabet soup of regulatory programs through the end of 2018.
What are the 4 purposes of meaningful use?
They were: Improve quality, safety, efficiency, and reduce health disparities. Increase patient engagement. Improve care coordination.
Which MIPS category replaced meaningful use?
Advancing Care Information (ACI)The Advancing Care Information (ACI) category of MIPS replaces the Medicare EHR Incentive Program (Meaningful Use). This category will reflect how well clinicians use EHR technology, with a special focus on objectives related to interoperability and information exchange.
What is meaningful use stage1?
Meaningful use stage 1 is the first phase of the United States federal government's meaningful use incentive program, which details the requirements for the use of electronic health record (EHR) systems by hospitals and eligible health care professionals.
What is Stage 2 Meaningful Use?
In order to qualify for CMS Meaningful Use Stage 2 incentives, eligible providers need to ensure that at least 5% of their patients use the provider’s “patient portal.” This means that patients must send an online message to their clinician, or patients need to view, download or transmit health information via the portal.
Do physicians have adequate programs in place to introduce patients to such online resources?
The survey concluded that “many physicians do not have adequate programs in place to introduce patients to such online resources, and are not engaging their patients post-appointment. By investing more resources and time into such initiatives, physicians will likely be able to raise their patient portal engagement rates, meet Meaningful Use Stage 2 requirements, and cultivate greater acceptance of online portals in their patient populations.”
Do primary care physicians follow up with patients?
What’s more surprising is that almost half of primary care physicians didn’t follow-up with their patients following an office visit. For those who had a follow-up encounter, less than 10% was through a patient portal. For general communication, patients prefer to be contacted by phone; email is the second choice. The same holds true for receiving lab results or diagnoses.
What is CMS' role in protecting patient information?
CMS is taking additional steps to provide payers and patients opportunities and information to protect patient data and make informed decisions about sharing patient health information with third parties. For instance, as part of this final rule a payer may ask third-party application developers to attest to certain privacy provisions, such as whether their privacy policy specifies secondary data uses, and inform patients about those attestations. CMS is also working with payers to provide information they can use to educate patients about sharing their health information with third parties, and the role of federal partners like the Office for Civil Rights (OCR) and the Federal Trade Commission (FTC) in protecting their rights.
What is CMS 9115-F?
Overview#N#The Interoperability and Patient Access final rule (CMS-9115-F) delivers on the Administration’s promise to put patients first, giving them access to their health information when they need it most and in a way they can best use it. As part of the Trump Administration’s MyHealthEData initiative, this final rule is focused on driving interoperability and patient access to health information by liberating patient data using CMS authority to regulate Medicare Advantage (MA), Medicaid, CHIP, and Qualified Health Plan (QHP) issuers on the Federally-facilitated Exchanges (FFEs).
What is CMS data exchange?
Payer-to-Payer Data Exchange: CMS-regulated payers are required to exchange certain patient clinical data (specifically the U.S. Core Data for Interoperability (USCDI) version 1 data set) at the patient’s request, allowing the patient to take their information with them as they move from payer to payer over time to help create a cumulative health record with their current payer. Having a patient’s health information in one place will facilitate informed decision-making, efficient care, and ultimately can lead to better health outcomes. These payers are required to implement a process for this data exchange beginning January 1, 2022 (for QHP issuers on the FFEs, plan years beginning on or after January 1, 2022).
What is provider directory API?
Provider Directory API: CMS-regulated payers noted above (except QHP issuers on the FFEs) are required by this rule to make provider directory information publicly available via a standards-based API. Making this information broadly available in this way will encourage innovation by allowing third-party application developers to access information so they can create services that help patients find providers for care and treatment, as well as help clinicians find other providers for care coordination, in the most user-friendly and intuitive ways possible. Making this information more widely accessible is also a driver for improving the quality, accuracy, and timeliness of this information. MA organizations, Medicaid and CHIP FFS programs, Medicaid managed care plans, and CHIP managed care entities are required to implement the Provider Directory API by January 1, 2021. QHP issuers on the FFEs are already required to make provider directory information available in a specified, machine-readable format.
What is patient access API?
Patient Access API: CMS-regulated payers, specifically MA organizations, Medicaid Fee-for-Service (FFS) programs, Medicaid managed care plans, CHIP FFS programs, CHIP managed care entities, and QHP issuers on the FFEs, excluding issuers offering only Stand-alone dental plans (SADPs) and QHP issuers offering coverage in the Federally-facilitated Small Business Health Options Program (FF-SHOP), are required to implement and maintain a secure, standards-based (HL7 FHIR Release 4.0.1) API that allows patients to easily access their claims and encounter information, including cost, as well as a defined sub-set of their clinical information through third-party applications of their choice. Claims data, used in conjunction with clinical data, can offer a broader and more holistic understanding of an individual’s interactions with the healthcare system, leading to better decision-making and better health outcomes. These payers are required to implement the Patient Access API beginning January 1, 2021 (for QHP issuers on the FFEs, plan years beginning on or after January 1, 2021).
When is the provider directory API required for MA?
MA organizations, Medicaid and CHIP FFS programs, Medicaid managed care plans, and CHIP managed care entities are required to implement the Provider Directory API by January 1, 2021. QHP issuers on the FFEs are already required to make provider directory information available in a specified, machine-readable format.
When will CMS start reporting?
Digital Contact Information: CMS will begin publicly reporting in late 2020 those providers who do not list or update their digital contact information in the National Plan and Provider Enumeration System (NPPES). This includes providing digital contact information such as secure digital endpoints like a Direct Address and/or a FHIR API endpoint. Making the list of providers who do not provide this digital contact information public will encourage providers to make this valuable, secure contact information necessary to facilitate care coordination and data exchange easily accessible.
What is Meaningful Use?
In 2018, Meaningful Use (MU) became known as Promoting Interoperability Programs². Participants can attest to the Medicare Promoting Interoperability Programs or Medicaid Promoting Interoperability Programs.
How much is the EHR incentive?
Under Medicare¹⁴, the EHR incentive payment amount is equal to 75 percent* of an Eligible Professional’s Medicare physician fee schedule allowed charges submitted not later than two months after the end of the calendar year. *subject to an annual limit.
How long do you have to report to CMS for Medicare?
Participants of the Medicare Promoting Interoperability Program¹¹ (eligible hospitals and CAHs) are required to report for any continuous 90-day period attesting to CMS.
When did CMS start EHR incentive?
The Centers for Medicare & Medicaid Services (CMS) established the EHR Incentive Programs (also known as meaningful use) in 2011. The EHR Incentive Program encourages Eligible Professionals (EPs), Critical Access Hospitals (CAHs), and eligible hospitals to execute, manage, and prove meaningful use of Certified Electronic Health Record Technology (CEHRT).
What is the final score for MIPS?
The MIPS eligible clinician’s final score range is 0 to 100 and determines their payment adjustment.
What is MIPS in healthcare?
Merit Based Incentive Payments System (MIPS) is a payment track created under MACRA. It aims to link payments to the quality of care provided, improve care processes and health outcomes, increase the use of healthcare information, and reduce the cost of care.
What is the 21st century cures act?
The 21st Century Cures Act aims to ensure that all parties (patients, caregivers, and healthcare providers) have appropriate access to electronic health information. The Act also promotes access to electronic health information in a secure and straightforward manner. Patients should be able to access their electronic medical records free of charge. Providers should have the freedom to choose easy to use, reasonably priced health IT tools to facilitate the best care for their patients.
What is the ONC 2015 edition?
As of 2019, all EPs must use EHRs that are certified to the ONC 2015 Edition cancer reporting standards in order to use cancer reporting as one of their public health measures for incentive payments. which includes cancer. as a public health registry reporting measure.
What is the HITECH Act?
The HITECH Act supports the concept of meaningful use (MU) of electronic health records (EHR), an effort led by the Centers for Medicare & Medicaid Services (CMS) and the Office of the National Coordinator for Health IT (ONC). HITECH proposes the meaningful use of interoperable electronic health records throughout the United States’ health care ...
What is the Promoting Interoperability Program?
Promoting Interoperability Program (Formerly Meaningful Use) Overview. The American Recovery and Reinvestment Act, enacted in February 2009, includes many measures to modernize our nation’s infrastructure, one of which is the Health Information Technology for Economic and Clinical Health (HITECH) Act. External.
Why is population based cancer surveillance important?
Population-based cancer surveillance is critical for cancer control activities aimed at reducing cancer morbidity and mortality, the second leading cause of death in the United States and the leading cause of death in Canada.
Meaningful Use
To qualify for incentive payments through the Centers for Medicare & Medicaid Services EHR Incentive Programs, eligible providers and hospitals must demonstrate meaningful use of an electronic health record (EHR).
For More Information
For more information on meaningful use and how achieving meaningful use can help you improve health care quality and patient outcomes, see the following resources.
What is a patient portal?
A patient portal is a secure online website, managed by a health care organization, that provides patients access to their personal health information [1-3]. Portals were developed to provide patients with a platform through which to claim ownership over their health care. For patients that adopt health care portals, usage of the portal has been shown to positively impact health outcomes [1]. Despite their introduction in the late 1990s to augment patient engagement [2], widespread adoption of patient portals was not seen until 2006 [2,4]. As of 2018, a reported 90% of health care organizations offer patients portal access, with the remaining 10% reporting plans to adopt this tool [5].
What are the most commonly studied patient portal metrics?
Patient use was the most commonly studied patient portal metric, analyzed in 90% (78/87) of studies. Super user designations were only found in 24% (21/87) of studies, making this the least commonly studied metric. Table 2identifies the frequency with which each metric was included in each study, with totals for each metric [6-10,18,22-102]. There were 32 different combinations of study metrics, identified in Table 3, with the two most common metric combinations being patient use/adoption, frequency, and intensity (n=9) and patient use/adoption alone (n=9). The majority of studies (53/87, 61%) analyzed three or fewer metrics, with 3.11 as the average number of metrics reported. The definitions of these 271 metrics are summarized by study in Multimedia Appendix 1.
What is stratified user?
Users stratified in a way that distinguishes a high-utilization or high-activity group (eg, in terms of greater intensity, a categorically higher frequency, consistent duration of use, etc).
What is portal use?
Portal use by providers, care teams, or other staff. This use could be in terms of adoption, frequency, intensity, duration, or super user, per below; patient utilization grouped by provider practice/specialty also implies provider/practice adoption.
What are the coding purposes of super user?
For coding purposes, use/adoption, frequency, duration, intensity, and super user (or similar user stratification) were considered a priori themes from which to extract definitions; provider use emerged as a theme inductively. Super user, in this context, is synonymous with high utilizer and should not be confused with the information technology standard definition implying a user with elevated privileges. All metrics were coded as binary, indicating the presence of a measure for and/or definition of each respective metric. These data were coded and recorded in a spreadsheet containing the article citation information and columns for themes of interest for both portal use metric definitions and MU criteria. Extractors’ working definitions of metric types are summarized in Table 1.
How does portal utilization affect health outcomes?
Numerous studies have investigated the relationship between patient portal utilization and health outcomes, specifically indicating a link between increased portal use and increased rates of patient engagement [6-9]. Notably, engaged individuals more actively participate in the management of their health care [10] and report enhanced patient satisfaction [11], a finding increasingly critical in patients with chronic diseases [12]. Patient portal utilization has been linked to “significant decreases in office visits…, changes in medication regimen, and better adherence to treatment” [13], along with improved chronic disease management and disease awareness [8,9]. Interestingly, even the content of patient messages was recently found to be associated with estimated readmission rates in patients with ischemic heart disease [14]. In these ways, patient portals have been cited as essential components of the solution to the cost and quality health care crisis in the United States [2].
Can portal utilization be meaningful?
Understanding how patient portal use has been defined and operationalized may encourage more consistent, well-defined, and perhaps more meaningful standards for utilization, informing future portal development.
How can providers improve patient engagement?
Some key actions that providers should take to improve patient engagement is to implement proactive and engaging features as well as promote and expedite portal use . There are a variety of benefits providers gain from portals such as efficient and effective communication channels with patients, greater self-care initiative from patients, and higher patient satisfaction.
Why is it important to have more control over your own health?
Having patients be more aware and have more control over their own health is necessary to ensure better patient outcomes and quality of care. The Centers for Medicare & Medicaid Services (CMS) state on their website these intentions as their primary reason for emphasizing patient engagement in Stage 2 Meaningful Use requirements under the Medicare and Medicaid EHR Incentive Programs.
What is Stage 2 Meaningful Use?
Stage 2 Meaningful Use calls for more patient-centered care that includes providing patients with access to download and view their electronic health information through portals. Additionally, providers are encouraged to send patient follow-up reminders and preventive care correspondence.
Is patient portal expanding?
Currently, patient portals are expanding not only nationwide but also across the globe. A press release from Frost & Sullivan emphasizes the high adoption rate of patient portals in Africa.
Can older people access their health information through a portal?
Often, the older population may not be as tech-savvy with regard to accessing their health data through a patient portal. ONC suggests training these patients to use the tools and services available through a portal.