Emergency Medical Treatment & Labor Act (EMTALA)
21 hours ago · Section 1867 of the Social Security Act imposes specific obligations on Medicare-participating hospitals that offer emergency services to provide a medical screening examination (MSE) when a request is made for examination or treatment for an emergency medical … >> Go To The Portal
When a patient is transferred under EMTALA What are the responsibilities of the receiving hospital?
Receiving hospitals have a duty to report any inappropriate transfer received from a transferring institution. A hospital that suspects it may have received an improperly transferred individual (transfer of an unstable individual with an EMC who was not provided an appropriate transfer according to 42 C.F.R.
Which statement is an EMTALA violation?
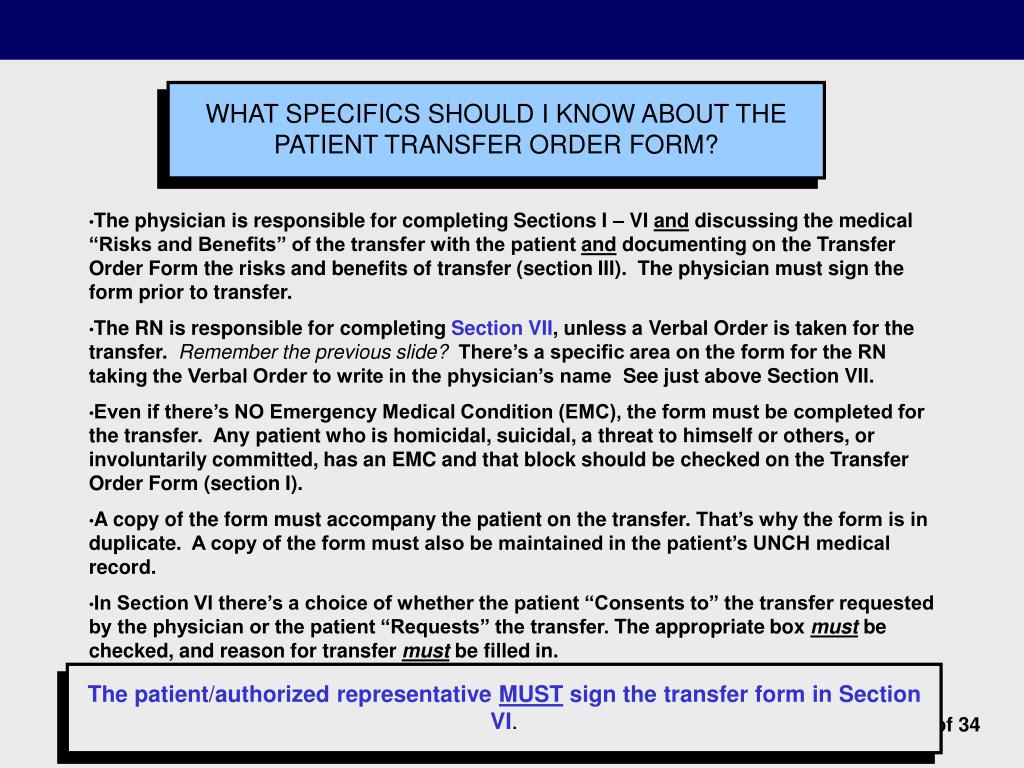
(Transferring a patient without copies of the medical record, including imaging, is an EMTALA violation.) Correspondingly, the law mandates that the receiving hospital accept the patient, as long as it has the appropriate resources to care for the patient.
Which of the following is an example of a violation of the Emergency Medical Treatment and Active Labor Act?
Which of the following is an example of a violation of the Emergency Medical Treatment and Active Labor Act (EMTALA)? A patient with low blood pressure and tachycardia is transferred to another hospital without intravenous access or supplemental oxygen.
What is an EMTALA log?
Policy: The hospital will maintain a Central Log containing information on each individual who comes on the hospital campus requesting assistance or whose appearance or behavior would cause a prudent layperson observer to believe the individual needed examination or treatment, whether he or she left before a medical ...
What are the most common EMTALA violations hospitals are cited for?
WebMD and Georgia Health News found that the most common EMTALA violations were for failing to conduct thorough medical screening exams, accounting for more than 1,300 of the violations.
Which of these is a potential penalty for an EMTALA violation?
What are the penalties for violating EMTALA? > Termination of the hospital or physician's Medicare provider agreement.
What are EMTALA obligations?
The Emergency Medical Treatment and Labor Act (EMTALA) requires hospitals with emergency departments to provide a medical screening examination to any individual who comes to the emergency department and requests such an examination, and prohibits hospitals with emergency departments from refusing to examine or treat ...
What are the requirements of the Emergency Medical Treatment and Active Labor Act that hospitals must meet?
The Emergency Medical Treatment and Active Labor Act (EMTALA) and Its Effects. Ensuring a patient is stabilized requires that, within reasonable medical certainty, no material deterioration in the patient's condition should occur during transfer or upon discharge from the hospital.
What does the Emergency Medical Treatment and Active Labor Act EMTALA mandate for a patient who presents to the ED having labor contractions?
The Emergency Medical Treatment and Labor Act (EMTALA) is a federal law that requires anyone coming to an emergency department to be stabilized and treated, regardless of their insurance status or ability to pay, but since its enactment in 1986 has remained an unfunded mandate.
Which of the following should be included in the central log to satisfy EMTALA requirements?
The central log should document the patient's name, the date and time of arrival, the time the patient was seen, and the disposition and time of disposition. The central log should also include patients that came to the Emergency Department but left prior to being seen.
What triggers EMTALA?
EMTALA is triggered whenever a patient presents to the hospital campus, not just the physical space of the ED, that is, within 250 yards of the hospital. Hospital-owned or operated ambulances have an EMTALA obligation to provide medical screening examination and stabilization.
What agency is primarily responsible for enforcing EMTALA?
CMS and the OIG are jointly responsible for enforcing EMTALA. CMS initiates EMTALA investigations in response to complaints of alleged violations.
Where is Emtala heard?
Because EMTALA is a federal statute, such cases are usually heard in federal courts. These include the federal district courts, the US Court of Appeals, and finally (in only one EMTALA-related case to date) the US Supreme Court. EMTALA imposes 3 distinct legal duties on hospitals.
How many uninsured patients were in the ED in 1996?
According to the American Hospital Association (AHA), in 1996 about 16% of ED patients were uninsured (29). The ED is the portal of entry for as many as 3 of every 4 uninsured patients admitted to the nation's hospitals (30). Traditionally, uncompensated care was recouped by charging more for services for the insured.
What is appropriate transfer?
(A) in which the transferring hospital provides the medical treatment within its capacity which minimizes the risks to the individual's health and , in the case of a woman in labor, the health of the unborn child ;
What is an emergency medical condition?
(A) a medical condition manifesting itself by acute symptoms of sufficient severity (including severe pain) such that the absence of immediate medical attention could reasonably be expected to result in— .
How much is a fine for a negligent hospital?
Participating hospitals and physicians who negligently violate the statute are subject to a civil monetary penalty not to exceed $50,000 (or $25,000 for hospitals with <100 beds) for each violation. Because a single patient encounter may result in >1 violation, fines can exceed $50,000 per patient.
When was the Emergency Medical Treatment and Active Labor Act passed?
This article has been cited byother articles in PMC. The Emergency Medical Treatment and Active Labor Act (EMTALA) was passed by the US Congress in 1986 as part of the Consolidated Omnibus Reconciliation Act (COBRA), much of which dealt with Medicare issues. The law's initial intent was to ensure patient access to emergency medical care ...
Does a hospital have to be on call list?
Generally, any service that the hospital routinely offers must be represented on the list. Thus, if the hospital does not do orthopaedic surgery or have a psychiatric unit, then these physicians need not be on the call list. Since virtually all services are performed at BUMC, the on-call list is extensive.
What is an EMTALA?
According to the law, EMTALA applies when an individual "comes to the emergency department.". CMS defines a dedicated emergency department as "a specially equipped and staffed area of the hospital used a significant portion of the time for initial evaluation and treatment of outpatients for emergency medical conditions.".
How much is a fine for a violation of EMTALA?
Physician fines $50,000 per violation, including on-call physicians. The hospital may be sued for personal injury in civil court under a "private cause of action". A receiving facility, having suffered financial loss as a result of another hospital's violation of EMTALA, can bring suit to recover damages.
What happens if an emergency medical condition is not treated?
If an emergency medical condition exists, treatment must be provided until the emergency medical condition is resolved or stabilized. If the hospital does not have the capability to treat the emergency medical condition, an "appropriate" transfer of the patient to another hospital must be done in accordance with the EMTALA provisions.
What is the Emergency Medical Treatment and Labor Act?
The Emergency Medical Treatment and Labor Act (EMTALA) is a federal law that requires anyone coming to an emergency department to be stabilized and treated, regardless of their insurance status or ability to pay, but since its enactment in 1986 has remained an unfunded mandate. The burden of uncompensated care is growing, closing many ...
How much bad debt did EMTALA have in 2001?
Physicians in other specialties provide, on average, about six hours a week of care mandated by EMTALA, and on average incurred about $25,000 of EMTALA-related bad debt in 2001.
Who must report an unstable patient to CMS?
A hospital must report to CMS or the state survey agency any time it has reason to believe it may have received an individual who has been transferred in an unstable emergency medical condition from another hospital in violation of EMTALA.
Is an outpatient clinic obligated under EMTALA?
This means, for example, that hospital-based outpatient clinics not equipped to handle medical emergencies are not obligated under EMTALA and can simply refer patients to a nearby emergency department for care.
What is EMTALA in medical terms?
EMTALA (Emergency Medical Treatment and Active Labor Act) Obligations: A Case Report and Review of the Literature.
What is reverse dumping in EMTALA?
Under EMTALA, the "reverse-dumping" provision prevents hospitals from refusing patients who require specialized capabilities or facilities if the hospital has the capacity to treat them. Despite this provision, patients continue to be transferred to distant tertiary care centers.
When was the Emergency Medical Treatment and Active Labor Act enacted?
Abstract. Background: The Emergency Medical Treatment and Active Labor Act (EMTALA) was enacted in 1986 in the United States to address "patient dumping," or refusing to provide emergency care to patients and instead transferring them to other hospitals. Under EMTALA, the "reverse-dumping" provision prevents hospitals from refusing patients who ...
Is EMTALA difficult to accept?
Under EMTALA, it is difficult for tertiary care centers to argue lack of specialized capabilities or capacity to accept patients, and neither hospitals nor physicians are compensated for the charges of providing care to uninsured or underinsured patients.
What are the commonalities of EMTALA?
Rather, what they have in common is the violation of one or more basic requirements of EMTALA – screening, stabilization and appropriate transfer.
What is a patient who presented to the ED via law enforcement with psychosis and homicidal
A patient presented to the ED via law enforcement with psychosis and homicidal ideation and was involuntarily committed. The patient did not receive psychiatric examination or treatment by available psychiatrists and was not admitted to the psychiatric unit for stabilizing treatment.
What happened to the EMC in Tennessee?
A Tennessee hospital entered into a $25,000 settlement agreement with OIG regarding allegations that it failed to stabilize an EMC for a 58-year-old patient who presented to the ED for blurred vision and dizziness. After failing to provide an appropriate EMC, an ED nurse directed the patient to a local eye doctor and failed to provide medical treatment to stabilize the patient's EMC, a cerebral infarction.
How old was the patient in the OIG?
The patient was a 35-year-old male with chest pain and shortness of breath who presented to the ED accompanied by his girlfriend.
Can a testicle be transferred to another hospital?
However, the on-call urologist at Hospital “B” refused to accept the transfer of the patient, recommending instead that the patient be transferred to another facility.
What is the treatment for EMTALA violation?
Treatment may include establishing IV access and administering oxygen. Failure to do so would be an EMTALA violation. Once the decision is made to transfer a patient, the transferring doctor must identify and document the name of the receiving facility and receiving doctor.
What is EMTALA law?
The EMTALA law applies when a person goes into an emergency department (ED) or labor and delivery department, and asks to be examined or treated for an “emergency medical condition (EMC).”. It also applies if someone else asks for care for that person on that person’s behalf.
What is the purpose of the Emergency Medical Treatment and Active Labor Act?
The Emergency Medical Treatment and Active Labor Act (EMTALA) enacted by congress in 1986, was put in place to ensure patient access to emergency care regardless of ability to pay. EMTALA was also intended to prevent “patient dumping”, which is the act of transferring an uninsured patient to another facility exclusively for financial reasons without regard to that patient’s medical condition. The information in this newsletter is a follow-up to the UPLNC blog from December 12, 2012.
Is sending a patient from one emergency department to another a violation of EMTALA?
PLEASE NOTE: Sending a patient from one emergency department to another is not necessarily a violation of EMTALA. This occurs commonly when the receiving hospital is expecting a bed to open in the inpatient floors but there is a delay in making that bed available.
What is the EMTALA law?
All About EMTALA: The Law That Runs the ED. EMTALA was meant to ensure emergency care for all. While it has provided that type of safety net, some unintended consequences have not been as positive. Enacted by Congress in 1986, the Emergency Medical Treatment and Labor Act (EMTALA) was designed to provide emergency care to all patients, ...
What are the responsibilities of EMTALA?
EMTALA defines 3 responsibilities of participating hospitals (defined as hospitals that accept Medicare reimbursement): 1. Provide all patients with a medical screening examination (MSE) Stabilize any patients with an emergency medical condition. Transfer or accept appropriate patients as needed. Responsibilities of Hospitals and Providers.
How much is EMTALA fine?
Fines can reach $100,000 per violation , and hospitals may be held liable for civil lawsuits, either from patients or from transferring or receiving hospitals. Consequences.
When was the Emergency Medical Treatment and Labor Act passed?
Enacted by Congress in 1986, the Emergency Medical Treatment and Labor Act (EMTALA) was designed to provide emergency care to all patients, regardless of insurance status or ability to pay. But some of the unintended consequences of EMTALA have not been as positive. EMTALA defines 3 responsibilities of participating hospitals ...
Does the ACA eliminate uncompensated care?
The ACA was designed to eliminate uncompensated care , but the reluctance of some states to expand Medicaid has hampered those efforts, and states that have expanded Medicaid have seen a bigger drop in uncompensated care than those that haven't. 7.
Is Medicaid expansion a threat to hospitals?
Resistance to Medicaid expansion is not the only threat to hospital finances due to uncompensated care. 8 Many insurers are now implementing policies to reduce reimbursement for ED visits retroactively deemed to be non-emergent. In an age where 40% of health insurance plans are considered high deductible, 9 this policy threatens to increase ...