5+ SAMPLE Patient Incident Report in PDF
17 hours ago 5+ SAMPLE Patient Incident Report in PDF. Rating : According to the World Health Organization, every year in the United States, up to 440,000 individuals die as a result of hospital errors, which include injuries, accidents, and infections, among other things. Many of those deaths could have been avoided if medical facilities had kept better records of their encounters with patients. >> Go To The Portal
Consider the following examples as situations in which an incident report should be filed:
- You’re working as a nurse on an acute inpatient psych unit when one of the patients begins to act violently and attacks...
- You’re ambulating a patient in the hallway and securely holding onto their gait belt when the patient abruptly falls to...
Full Answer
What is an example of an incident report?
If there is an injury, illness or damage as a result of the hazard, that is an incident and should be reported as such. For example… If no one changes a burned out lightbulb leading to dimly lit conditions in an area, that is a hazard.
How to write an incident report?
Writing Incident Reports-Tips and Examples How to write a helpful and professional incident report Be specific, detailed, factual, and objective. Language: This information can be used by many institutional and external partners so make sure to use language that you wouldn’t mind President Phipps reading.
What is a hospital incident report?
The man has not been identified. Medical staff at the hospital told investigators that the man's injuries were not consistent with a traffic accident. The incident report indicates that the man was injured by a gunshot. However, the official cause of death ...
How to write an effective incident report [templates]?
How To Write An Effective Incident Report
How do you write a patient incident report?
What to Include In a Patient Incident ReportDate, time and location of the incident.Name and address of the facility where the incident occurred.Names of the patient and any other affected individuals.Names and roles of witnesses.Incident type and details, written in a chronological format.More items...•
What are some examples of healthcare incidents?
A healthcare incident refers to an unintended or unexpected event that harms a patient or caregiver—or has the potential to harm them....2. Incidents related to the dispense of medication include:Wrong dose of prescription indicated.Wrong medication supplied.Incomplete or incorrect medication handoffs.
What are the 4 types of incident reports?
Common Types of Incident ReportsWorkplace. Workplace incident reports detail physical events that happen at work and affect an employee's productivity. ... Accident or First Aid. ... Safety and Security. ... Exposure Incident Report.
How do you write an incident report in nursing example?
What Information Do You Put in an Incident Report?Detailed description of the event with events listed chronologically.Witnesses or injured party statements.Injuries sustained by the person(s) as a result of the incident or the outcome.Actions taken immediately after the incident occurred.Treatments administered.More items...•
What are examples of incidents?
The definition of an incident is something that happens, possibly as a result of something else. An example of incident is seeing a butterfly while taking a walk. An example of incident is someone going to jail after being arrested for shoplifting.
What are incident reports in healthcare?
Incident reporting in healthcare refers to collecting healthcare incident data with the goal to improve patient safety and care quality. Done well, it identifies safety hazards and guides the development of interventions to mitigate risks, thereby reducing harm.
What are the 3 types of incidents?
3 Types of Incidents You Must Be Prepared to Deal WithMajor Incidents. Large-scale incidents may not come up too often, but when they do hit, organizations need to be prepared to deal with them quickly and efficiently. ... Repetitive Incidents. ... Complex Incidents.
What six points should be included in an incident report?
In this post, we'll answer those questions and more by outlining the six key elements that every good incident report should contain....Holistic also means that the incident report form covers the four main types of incidents.Near misses. ... No harm events. ... Adverse events. ... Sentinel events.
What makes a good incident report?
Effective Incident Reports identify the facts and observations. They avoid inclusion of personal biases; they do not draw conclusions/predictions, or place blame. Effective Incident Reports use specific, descriptive language and identified the action(s) taken by staff as a result of the unusual incident.
When should a nurse write an incident report?
The rule of thumb is that any time a patient makes a complaint, a medication error occurs, a medical device malfunctions, or anyone—patient, staff member, or visitor—is injured or involved in a situation with the potential for injury, an incident report is required.
What is the most common type of incident reporting event?
medication incidentsThe most common types were medication incidents (29%), falls (14%), operative incidents (15%) and miscellaneous incidents (16%); 59% seemed preventable and preventability was not clear for 32%. Among the potentially preventable incidents, 43% involved nurses, 16% physicians and 19% other types of providers.
What is the nurse's responsibility regarding incident reporting?
Nurses have a duty to report any error, behaviour, conduct or system issue affecting patient safety. This accountability is found in section 6.5 of the Code of Conduct. Medications and devices prescribed to patients can cause unforeseen and serious complications.
How Effective Are Incident-Reporting Systems for Improving Patient Safety?
It is possible to acquire information on patient safety occurrences through the use of incident-reporting systems (IRSs). Even if they come with a...
When to Report an Incident to the Police?
The general rule of thumb is that an incident report should be completed as quickly as possible after an occurrence happens. Minor injuries should...
How Are Patient Safety Event Reporting Systems used?
Hospitals are replete with patient safety event reporting systems, which serve as a cornerstone of efforts to detect patient safety incidents and q...
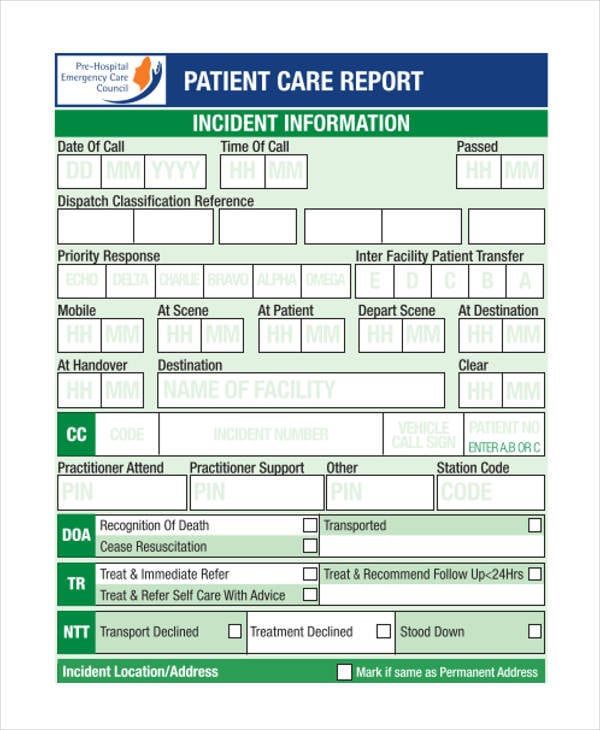
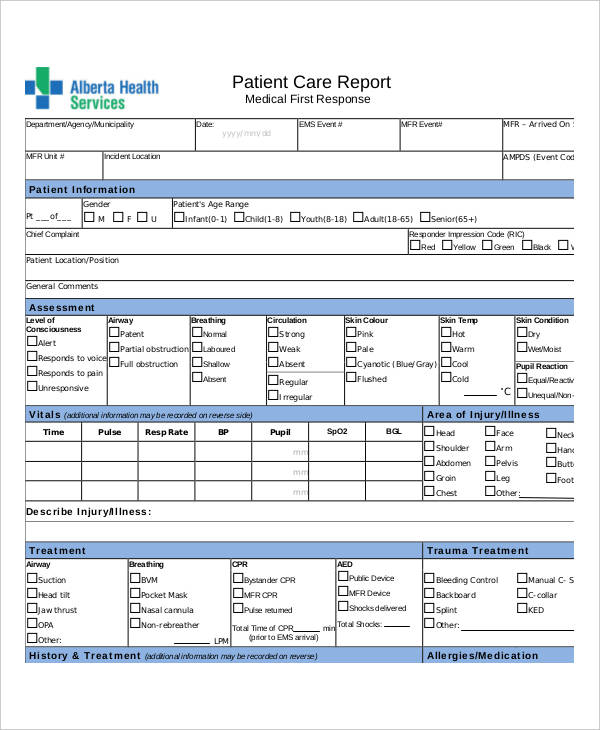
What is a patient care report?
A patient care report is a document made mostly by the EMS or EMTs. This documented report is done after getting the call. This consists of the inf...
What should not be written in a patient care report?
What should be avoided in a patient care report is making up the information that is not true to the patient. This is why you have to be very caref...
Who is in charge of reading the patient care report?
The person or the people who will be reading the report are mostly medical authorities. When you are going to be passing this kind of report, make...
What to include in an incident report?
Every facility has different needs, but your incident report form could include: 1 Date, time and location of the incident 2 Name and address of the facility where the incident occurred 3 Names of the patient and any other affected individuals 4 Names and roles of witnesses 5 Incident type and details, written in a chronological format 6 Details and total cost of injury and/or damage 7 Name of doctor who was notified 8 Suggestions for corrective action
Why do we use resolved patient incident reports?
Using resolved patient incident reports to train new staff helps prepare them for real situations that could occur in the facility. Similarly, current staff can review old reports to learn from their own or others’ mistakes and keep more incidents from occurring. Legal evidence.
Why is it important to review patient incidents?
Reviewing incidents helps administrators know what risk factors need to be corrected within their facilities , reducing the chance of similar incidents in the future.
Why is it important to know that an incident has occurred?
Knowing that an incident has occurred can push administrators to correct factors that contributed to the incident. This reduces the risk of similar incidents in the future. Quality control. Medical facilities want to provide the best care and customer service possible.
How long does it take to file a patient incident report?
Patient incident reports should be completed no more than 24 to 48 hours after the incident occurred.
Why is it important to document an incident?
Even if an incident seems minor or didn’t result in any harm, it is still important to document it. Whether a patient has an allergic reaction to a medication or a visitor trips over an electrical cord, these incidents provide insight into how your facility can provide a better, safer environment.
How many hospital incidents go unreported?
According to a study by the US Department of Health and Human Services, 86 per cent of hospital incidents go unreported. Even more staggering, though, is the reason behind this. Staff did not consider 62 per cent of incidents as reportable, due to unclear incident reporting requirements.
What Is a Patient Care Report?
We often hear of care reports based on by medical teams or by medical authorities. Yet, we are not sure how this differs from the kind of report that is given to us by the same people. So this is the time to make it as clear as possible.
How to Write a Patient Care Report?
Where do you even begin when you write a patient care report? A lot of EMS or EMTs do know how to write one since they are trained to do so.
What is a patient care report?
A patient care report is a document made mostly by the EMS or EMTs. This documented report is done after getting the call. This consists of the information necessary for the assessment and evaluation of a patient’s care.
What should not be written in a patient care report?
What should be avoided in a patient care report is making up the information that is not true to the patient. This is why you have to be very careful and very meticulous when writing these kinds of reports. Every detail counts.
Who is in charge of reading the patient care report?
The person or the people who will be reading the report are mostly medical authorities. When you are going to be passing this kind of report, make sure that you have all the information correctly. One wrong information can cause a lot of issues and problems.
What is incident report?
1. An Incident Report Must Be Accurate and Specific. When you write an incident report, you must be specific and accurate about the details, not merely descriptive. For example, instead of writing "the old patient", it is more accurate to describe him as "the 76-year old male patient".
How to organize an incident report?
How a report is organized depends on the complexity of the incident and the type of report being written. Usually, writing in chronological order is the simplest way to organize a report. However, an inspection incident report may be written by enumerating details according to findings. 5. A Good Incident Report Must Be Clear.
What is the best way to write an incident report?
It is also best to write in an active voice, which is more powerful and interesting than the passive voice. 2. A Good Incident Report Must Be Factual and Objective.
What abbreviations should be used in an incident report?
A Good Incident Report Must Only Include Proper Abbreviations. The use of abbreviations may be appropriate in certain cases, such as the use of Dr. Brown and Mr. Green, instead of writing Doctor or Mister.
Do you have to include your opinion in a report?
If you must include an opinion in your report, it is best to state it with the similar description that appears on some incident report samples: "In my opinion, there were too many people in the overloaded bus. In fact, there were 80 persons inside, when a bus of this size is only allowed to carry 70 individuals."
Do you need an incident report in court?
Your incident report may be needed in court someday and you should be prepared to be questioned based on your report. So the more details you have on your report, the less you have to depend on your memory and the more credible you are.
What Is a Nursing Incident Report?
We know what an incident report is and what it looks like. But do we have any idea as to what a nursing incident report is and what it looks like? Is there even any difference between these two kinds of reports? A nursing incident report is a kind of report that is filled out by nurses or anyone in the health care or medical field.
How to Write a Nursing Incident Report?
Being able to know what can and cannot be written in a nursing incident report is important. Take note that this document is a formal written report, and must be treated as such all the time. So to not make any mistakes when writing your incident report, here are five simple tips to guide you when you are writing your nursing incident report.
What is a nursing incident report?
A nursing incident report is a kind of report that a nurse or any health care worker writes to report an incident. This report gives a good bird’s eye view of how the incident happened and what can be done to resolve it.
Why is it so important to write about the incident in detail?
The reason it is necessary to write the incident in detail is to make sure that you have written out what really happened. Not fabricating anything in the report and to make sure that anyone who was there is also aware of what happened. That they can assure the one reading your report that it really happened.
What is something that should be avoided when writing a nursing incident report?
Forgetting to place the evidence or the proof of what happened. As well as not rearranging in chronological order as to how it happened. Details are an important part of the incident report.
What Is a Nursing Incident Report?
A Nursing Incident Report is a document may it be a paper or a typewritten one that provides detailed information and account of the chain of events leading up to and following an unforeseen circumstance in a healthcare setting or facility especially in the nursing side.
What Are the Information Needed in a Nursing Incident Report?
An incident report should be completed every time that an accident or any mishaps in giving care to the patient or any instances or possibilities of deviating from the normal operation and routine of the facility and/or from the patient.
What Is the Desired Outcome of Writing a Nursing Incident Report?
In writing an incident report a positive outcome should always be manifested but that depends on the event of the accident. There are times that the outcomes are deviated from what we expect and manifest. For pessimistic situations that will not happen in the future, a good, desired outcome must be manifested in writing a nursing incident report.
What Is the Difference Between a Nursing Incident Report and Medical Incident Report?
Incidents happen from time to time. We cannot deny the fact that accidents of different kinds may occur or happen unexpectedly. Such cases may happen inside a hospital facility. It can happen in the operating room, wards, nurses’ station, laboratories, and even emergency rooms.
Purpose of a Nursing Incident Report
Nursing incident reports are used to initiate communication in sequencing events about the important safety information to the hospital administrators and keep them updated on aspects of patient care. Writing an incident report has its own purpose that will provide us a clearer understanding of how it works and how it is done.
How to Write a Nursing Incident Report
This is to confirm that an accident or incident has occurred that requires an incident report. Clinical reasoning and judgment must be possessed by a clinical health practitioner or any healthcare professional. It is a skill that is needed to be learned in a span of time.
What to Expect After Writing an Incident Report?
Information in the nursing incident report will be analyzed and comprehended to identify the root cause of the incident. This is subject to changes that need to be made in the facility or to facility processes to prevent recurrence of the incident and promote overall safety and quality of care.
What are healthcare incidents, and what causes them?
A healthcare incident refers to an unintended or unexpected event that harms a patient or caregiver—or has the potential to harm them. Incidents or errors occur for various reasons or root causes, such as system design flaws, lack of administrative oversight, poor training, digression from protocols, miscommunication, and more.
What are examples of incidents in healthcare?
Unfortunately, one doesn’t need to look far to find examples of incidents in healthcare. That’s because the industry is incredibly complex and fast-paced. It’s easy to make honest mistakes. For example:
What are the most commonly-reported hospital incidents?
Medication-related incidents are the most commonly reported incidents in healthcare. This includes administering the wrong dose, giving medication to the wrong patient, or omitting the dose.
Incidents: Insight to patient safety risks
Learning why incidents occur can help organizations make improvements to prevent them from happening again. But first, the healthcare system must prioritize incident reporting by providers, staff, and patients. In fact, risk management and patient safety rely on healthcare’s collective:
Are there incident severity levels?
The World Health Organization (WHO) classifies healthcare incidents according to the levels of severity (i.e., mild, moderate, severe, or death) based on the severity of the symptoms or loss of function, the duration of the symptoms, and/or the interventions required as a result of the incident.
What is incident management?
Incident management refers to the process of analyzing incidents and identifying the causes. Incident management entails more than simply filling out an incident report to track events and prevent them from occurring again. Incident management is also increasingly about handling data for quality improvement that affects reimbursement.
The symplr approach
Preventable harm will continue to occur unless organizations take a proactive approach to mitigate risk. That’s where symplr can help. symplr’s patient safety and risk management software is a structured digital event management system that captures (near) incidents, provides analytics, manages workflows, and monitors improvements.
What is incident report?
An incident report is a formal recording of the facts related to a workplace accident, injury, or near miss. Its primary purpose is to uncover the circumstances and conditions that led to the event in order to prevent future incidents. Every incident report you file should contain a minimum of the following:
Why do you need to create an incident report?
Create an incident report as soon as your employees are safe, which includes seeking medical attention and implementing an immediate corrective action to prevent further danger or damage. By recording details immediately, you improve the accuracy of your report and the effects of your corrective actions.
Why is incident reporting important?
Their importance means you want to get as much relevant information as you can as quickly as possible.
What to do after documenting an incident?
After documenting the incident, you may have legal reporting requirements. Report and store the files according to recordkeeping requirements from regulatory bodies. It’s generally best practice to preserve the files for the duration of employment.
What are the two common mistakes you should avoid when reporting an accident?
But sometimes, safety teams can get in their own way and miss out on important details by making common mistakes. Blame-casting and just getting it done are two common incident reporting mistakes you should avoid. It is easy to go on a witch hunt when accidents happen.
What happens if you rush through a report?
In addition, if you rush through the report to “just get it done,” you may miss out on important details or lack clarity in wording. Irresponsible reporting can lead your team into even more danger, while detailed, clear reporting can lead to improved work conditions and better training.
How long does it take to complete a fact gathering report?
While it may take a few days to complete your report, it should take you only hours (or less) to start it. After an incident, secure the worksite for all crews and make sure injured employees are receiving medical care if needed. Start your fact gathering for your report immediately after this.
What is incident report?
An incident report is an electronic or paper document that provides a detailed, written account of the chain of events leading up to and following an unforeseen circumstance in a healthcare setting.
Why are incident reports important?
Incident reports are used to communicate important safety information to hospital administrators and keep them updated on aspects of patient care for the following purposes: Risk management. Incident report data is used to identify and eliminate potential risks necessary to prevent future mistakes.
How long does it take to complete an incident report?
To ensure the details are as accurate as possible, incident reports should be completed within 24 hours by whomever witnessed the incident. If the incident wasn’t observed (e.g., a patient slipped, fell, and got up on his own), then the first person who was notified should submit it.
What are some examples of reportable events in New York?
Examples: adverse reactions, equipment failure or misuse, medication errors.
What are the concerns of nurses?
Stressing over getting the report done or about what to include are common concerns for nurses — not to mention worrying about whether filing the report reflects badly on your performance. Mistakes happen all the time, and healthcare facilities are not immune.
What is an incident report?
A workplace incident report is a document that states all the information about any accidents, injuries, near misses, property damage or health and safety issues that happen in the workplace.
Why is a safety incident report important?
A safety incident report helps ensure nobody is subject to mistreatment because it contains information from the injured employee as well as eyewitnesses. This helps fill in missing pieces of information and figure out how the accident occurred exactly.
What is a general staff accident report?
It includes all the necessities to describe a workplace incident to ensure it is recorded correctly. This general form is ideal for any business type.
Why should an accident report be signed?
The accident report should be signed to acknowledge that it is everything that the employee remembers happening. This workplace incident report template includes the basic guidelines and best practices of what to include to make sure the report includes all the details it should.
What form do you fill out to keep a log of an OSHA incident?
If this is an OSHA recordable incident (accident) and the company is exempt from OSHA recordkeeping, the employer must also fill in OSHA Form 300 . This form enables both the employer and the agency to keep a log of the injuries or illnesses that happen in the workplace.
What should be noted when a workplace vehicle is involved?
If a workplace vehicle was involved, all information about the vehicle should be noted, and the possible reasons why it occurred if there is no clear answer. Employers should ensure vehicle safety guidelines are adhered to in order to prevent incidents in the workplace.
How long does it take to complete an accident report?
Typically, a workplace accident report should be completed within 48 hours of the incident taking place. The layout of an accident incident report should be told like a story, in chronological order, with as many facts as the witnesses can possibly remember.