10+ Patient Care Report Examples [ EMS, EMT, …
10 hours ago A lot of people believe that only nurses or health care workers can write reports.Most specifically patient care reports or anything that may be related to an incident report that often happens in hospitals or in some health care facilities. It would seem that when you hear the words patient and care with the word report mixed to it, you would immediately think, oh nurses are mostly … >> Go To The Portal
[TRANSPORT] Patient was transported without incident and without delay. Patient was transported to emergency department. Patient moved from stretcher to emergency department cot via with help of crew to steady as they moved. IV line still patent, no swelling or discoloration at insertion site. All of patient’s belongings were turned over to the hospital staff and/or patient. Patient care and report given to emergency department nurse. The patient has a Power of Attorney. The Power of Attorney is the patient’s Father. The person taking over patient care did not have any questions. The person taking over care received a patient report that included the patient’s medications, treatments, medical history and billing information.
Full Answer
How should EMS providers write patient care reports?
The days of hand-writing a patient care reports are nearly gone (or at least should be gone), but some EMS providers are stuck into their old ways of writing just enough of a narrative to fill the box, nothing more and nothing less. To best communicate the patient's story and paint a vivid picture, tell it like it happened.
What is the best format for writing a patient narrative?
This is just the start of a story, not the entire narrative. This narrative adequately describes the patient and an initial impression. SOAP, CHART single paragraph (and only a single paragraph) and chronological are common formats for patient care.
Can an EMS provider select “yes” or “no” in a clinical narrative?
However, simply clicking a box or making a selection from a drop-down menu cannot be a substitute for your words in the form of a clear, concise, accurate and descriptive clinical narrative. An EMS provider can select “yes” to the checkbox that the patient experienced chest pain, however that is not enough information.
What is a patient care report?
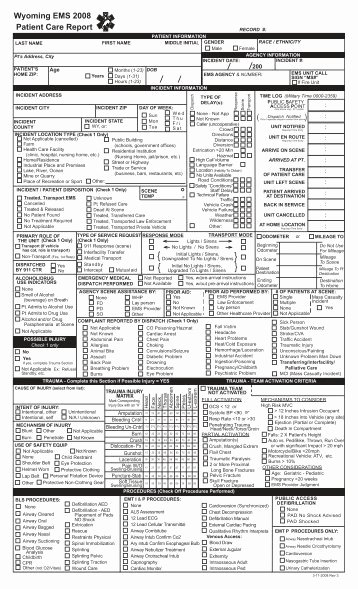
A patient care report is a document written by medical professionals to report about the patient’s wellbeing, care and status. This document consists of the result of the assessment and the evaluation of the patient being done by the EMTs or the EMS.

How do you write a patient care report for a narrative?
Present the facts in clear, objective language. Other important details to include are SAMPLE (Signs and Symptoms, Allergies, Medications, Past medical history, Last oral intake, and Events leading up to present injury) and OPQRST (Onset, Provocation, Quality of the pain, Region and Radiation, Severity, and Timeline).
How do I write an EMS patient care report?
EMS providers just need to pull the information together and write it down in a way that paints a picture....Follow these 7 Elements to Paint a Complete PCR PictureDispatch & Response Summary. ... Scene Summary. ... HPI/Physical Exam. ... Interventions. ... Status Change. ... Safety Summary. ... Disposition.
What should be included in a patient care report?
What Patient Care Reports Should IncludePresenting medical condition and narrative.Past medical history.Current medications.Clinical signs and mechanism of injury.Presumptive diagnosis and treatments administered.Patient demographics.Dates and time stamps.Signatures of EMS personnel and patient.More items...•
How do you write a PCR narrative in EMS?
The following five easy tips can help you write a better PCR:Be specific. ... Paint a picture of the call. ... Do not fall into checkbox laziness. ... Complete the PCR as soon as possible after a call. ... Proofread, proofread, proofread.
What is a patient care report in EMS?
The primary purpose of the Patient Care Report (PCR) is to document all care and pertinent patient information as well as serving as a data collection tool. The documentation included on the PCR provides vital information, which is necessary for continued care at the hospital.
How do you write a paramedic narrative?
1:2715:27I want you to think in your head that the documentation is just as important as the care we give ourMoreI want you to think in your head that the documentation is just as important as the care we give our patients okay if your care is great your documentation that'll be great because if your
What the patient care report represents?
Patient care report or “PCR” means a computerized or written report that documents the assessment and management of the patient by the emergency care provider in the out-of-hospital setting. “ Pharmacy-based” means that ownership of the drugs maintained in and used by the service program.
What does soap mean in EMS?
Subjective, Objective, Assessment and PlanIntroduction. The Subjective, Objective, Assessment and Plan (SOAP) note is an acronym representing a widely used method of documentation for healthcare providers. The SOAP note is a way for healthcare workers to document in a structured and organized way.[1][2][3]
What is a PCR in writing?
The PARCC Summative Assessments in Grades 3-11 will measure writing using three prose constructed response (PCR) items. In the classroom writing can take many forms, including both informal and formal.
How do you write a narrative document?
10 TIPS FOR WRITING EFFECTIVE NARRATIVE NURSE'S NOTESBe Concise. ... Note Actions Once They are Completed. ... When Using Abbreviations, Follow Policy. ... Follow SOAIP Format. ... Never Leave White Space. ... Limit Use of Narrative Nurse's Notes to Avoid Discrepancies. ... Document Immediately. ... Add New Information When Necessary.More items...•
What is a component of the narrative section of a patient care report?
The narrative section of the PCR needs to include the following information: Time of events. Assessment findings. emergency medical care provided. changes in the patient after treatment.
How do you make a narrative CHART?
CHART narratives also follow a visual layout based on the letters in the acronym. Starting with the chief Complaint, the History of the present illness, along with the patient's past medical history, are outlined. Assessment findings are then documented, along with Rx (prescriptions) that the patient is prescribed.
What is a patient care report?
A patient care report is a document made mostly by the EMS or EMTs. This documented report is done after getting the call. This consists of the inf...
What should not be written in a patient care report?
What should be avoided in a patient care report is making up the information that is not true to the patient. This is why you have to be very caref...
Who is in charge of reading the patient care report?
The person or the people who will be reading the report are mostly medical authorities. When you are going to be passing this kind of report, make...
Do agencies have documentation guidelines?
Most agencies have specific documentation guidelines. (I've never worked at one that hasnt) I'd check with your training officer.
Does Pt have a headache?
Pt states that she woke up with low grade abd pain and mild nausea, both of which have increased in severity throughout the day; pt has vomited 3x in past 5 hours (normal stomach contents) and has developed a low-grade headache. Pt has taken OTC medications (Dayquil, Advil) and attempted to rest with no relief.
What Should Be Included In A Patient Report?
Several elements should be included in the format including background information, medical history, physical examination, specimens obtained, and treatment given.
What Is Emt Report?
EMT is an EMT specialization. A 15 minute read. Prehospital medical care reports or PCR (also electronically recorded pPCR) provide detailed records of individual patient contact, treatment, transportation, and cancellation throughout each EMS service’s territory.
What Is A Writing Pcr?
Page 1. Students writing from 3-11 will use three PCR items to measure their written composition in the PARCC Summative Assessments. Whether it’s informal or formal, writing in a classroom can take a range of forms.
How to determine if a medical necessity is met?
A primary way to determine if medical necessity requirements are met is with documentation that specifically states why you took the actions you did on a call. For example, simply documenting “per protocol” as the reason why an IV was started or the patient was placed on a cardiac monitor is not enough.
Why is an IV established on the patient?
This specifically explains why an IV was established on the patient and states facts that can be used to show medical necessity for the call. The same can be said for non-emergency transports between two hospitals. Simply documenting that the patient was transported for a “higher level of care” is not good enough.
What should a PCR tell?
The PCR should tell a story; the reader should be able to imagine themselves on the scene of the call.
Why do you write PCR when you call?
Writing the PCR as soon as the call is over helps because the call is still fresh in your mind . This will help you to better describe the scene and the condition the patient was in during your call.
Do ambulances have to be medically necessary to be reimbursed by Medicare?
Ambulance services, including the treatments and interventions provided to the patient – need to be medically necessary to be reimbursed by Medicare and other payers – and that is determined primarily by reviewing the PCR.
Is PCR important in EMS?
We can all agree that completing a patient care report (PCR) may not be the highlight of your shift. But it is one of the most important skills you will use during your shift. Of course, patient care is the No. 1 priority of an EMS professional, and it is important to remember that completing a timely, accurate and complete PCR is actually ...
How to communicate patient story?
To best communicate the patient's story and paint a vivid picture, tell it like it happened. (Photo courtesy Omni EMS Billing)
What is the plan portion of the narrative?
Lastly is the Plan portion of the narrative, which depicts what you did to treat your patient. Establishing an IV, giving medications, relaying what was done prior to your arrival and what you did on-scene versus in transport.
What happens when you arrive at the hospital?
As you arrive at the hospital (new paragraph), you continue or discontinue some of your initial interventions, then transport your patient into the emergency department. The patient is transferred to the emergency department bed and you complete your hand-off report. Necessary information is relayed, and you return to your ambulance with your necessary paperwork and crew.
What is a disclaimer section in a narrative?
As an addition to any form of narrative, it may be appropriate to add a disclaimer section that notates other various actions or findings from your call. What items were left with the patient at the hospital, who signed your HIPAA/privacy and billing documents and any time discrepancies that may be noted can also be explained in this section.
What is an on-scene document?
On-scene (next paragraph), document what you performed, what the patient told you about their condition and history, what injuries you assessed and what your overall differential diagnosis of the patient is.
How many sentences are in a patient encounter?
The entire patient encounter is summarized into a single paragraph, often five to six sentences long. This, in terms of today’s documentation standards for quality assurance and reimbursement, simply isn’t enough.
Why are sections broken into different paragraphs?
To keep the documentation visually appealing and readable, sections are often broken into different paragraphs to denote a change in environment. Starting with your dispatch notes, response findings and initial patient impression, you can then build into your next paragraph, which includes your on-scene events.
Be Specific
Paint A Picture of The Call
- The PCR must paint a picture of what happened during a call. The PCR serves: 1. As a medical record for the patient, 2. As a legal record for the events that took place on the call, and 3. To ensure quality patient care across the service. PCRs should go beyond merely stating that a patient was picked up at a certain location, transported to anothe...
Do Not Fall Into Checkbox Laziness
- EMS professionals have long been promised a PCR that basically writes itself. Electronic PCR softwareis a great tool and can improve the efficiency of PCR completion. However, simply clicking a box or making a selection from a drop-down menu cannot be a substitute for your words in the form of a clear, concise, accurate and descriptive clinical narrative. An EMS provide…
Complete The PCR as Soon as Possible After A Call
- Most states, and many EMS agencies themselves, often have time limits within which the PCR must be completed after the call ended – 24, 48 or 72 hours are common time limits. While it is always important to comply with time limits, there are benefits to getting your PCR completed as soon as possible – preferably right after the call is completed and before your shift ends. In a pe…
proofread, proofread, Proofread
- The easiest way to improve your PCR is to proofread before submitting it. We understand the dilemma, after writing the sixth PCR for the day, and having 10 minutes left in the shift, the last thing anyone wants to do is sit there and reread what they have just written. But that is exactly what needs to be done. Poor grammar and spelling is the easiest way to have your abilities calle…