FREE 14+ Patient Report Forms in PDF | MS Word
1 hours ago In completing the patient report forms, below are the following important or essential information that should be provided. Otherwise, results from medical assessments cannot be given due to deficiency of relevant information. The patient’s personal information. The patient’s full name. The date of birth. >> Go To The Portal
What should be included in a patient assessment report?
This refers to the patient’s ability to move his muscles, from his eye to his arms and legs. The patient’s blood pressure, temperature, and pulse rate should also be indicated in the assessment report. Know the patient’s mental state.
What is a patient assessment form?
A patient assessment form is a type of medical assessment formthat is used by most medical institutions today as a means of keeping track of the development of a patient’s recovery. It is also a method of checking how well the patient is being treated during their time in the medical institution.
What is a patient report form?
Report Forms FREE 14+ Patient Report Forms in PDF | MS Word Healthcare personnel in hospitals or medical centers ensure that they provide the needs of the patients (pertaining to the treatments or medications needed) and their individual relatives (pertaining to the answers or provision of exact details from the medical results).
How to document a patient assessment (soap)?
How to Document a Patient Assessment (SOAP) 1 Subjective. The subjective section of your documentation should include how... 2 Objective. This section needs to include your objective observations,... 3 Assessment. The assessment section is where you write your thoughts on the salient issues and... 4 Plan. The final section is the plan,...
How do you write a patient report?
III. Patient case presentationDescribe the case in a narrative form.Provide patient demographics (age, sex, height, weight, race, occupation).Avoid patient identifiers (date of birth, initials).Describe the patient's complaint.List the patient's present illness.List the patient's medical history.More items...•
What is a patient assessment form?
A Patient Assessment Form is a document used when assessing a patient to determine the possible diagnosis and what kind of treatment the patient needs.
What is a patient report form?
The Patient Report Form provides a medico legal record of assessments, observations, treatment and actions undertaken by LAS clinicians. This information is essential to provide evidence that the clinician's duty of care has been fully met.
How do you write a good patient assessment?
Assessment & PlanWrite an effective problem statement.Write out a detailed list of problems. From history, physical exam, vitals, labs, radiology, any studies or procedures done, microbiology write out a list of problems or impressions.Combine problems.
What are the five steps of patient assessment?
emergency call; determining scene safety, taking BSI precautions, noting the mechanism of injury or patient's nature of illness, determining the number of patients, and deciding what, if any additional resources are needed including Advanced Life Support.
What are the components of a patient assessment?
WHEN YOU PERFORM a physical assessment, you'll use four techniques: inspection, palpation, percussion, and auscultation. Use them in sequence—unless you're performing an abdominal assessment. Palpation and percussion can alter bowel sounds, so you'd inspect, auscultate, percuss, then palpate an abdomen.
What is a PRF form?
The Personality Research Form (PRF) is an extensively researched and validated measure of normal personality. The PRF is designed to yield scores for personality traits relevant to the functioning of individuals in a wide variety of situations.
What is included in the review of systems?
The Review of Systems (ROS) is an inventory of the body systems that is obtained through a series of questions in order to identify signs and/or symptoms which the patient may be experiencing.
What is a PRF ambulance?
Ambulance trusts across the country are saving significant time by using Formic to scan and process millions of patient clinical records (PCR)/patient report forms (PRF).
How do you document an assessment?
An assessment report should accomplish the following:Outline the student learning or program outcomes or goals assessed during the assessment cycle timeframe.Identify and describe the specific assessment method(s) and tools used to gather evidence for the outcomes or goals.Identify the specific source(s) of the data.More items...
How do you write an assessment statement?
Five tips for writing a good assessmentMake it applicable. Think of the most realistic way of assessing the learner's ability. ... There shouldn't be any surprises. ... Test knowledge of the subject matter, not reading comprehension. ... Don't go above and beyond. ... Give learners the best chance of succeeding.
How do you document patient understanding?
Five Steps for Effective Documentation1) Use a standardized form. ... 2) Document formal and informal teaching. ... 3) Describe the response of the learners. ... 4) When possible, put copies of educational materials in the chart. ... 5) Update the teaching plan.
What is a new patient assessment form?
A new patient assessment form is a type of assessment form that is used as a means of assessing and grading a person development before and after they have entered the medical institution. This is typically done as a means of determining the state of health a patient was in prior to their admission to the hospital.
What is a health assessment?
This is done like clockwork to monitor a patient’s recovery, as well as the development of whatever ailment they may have at the time.
Why do hospitals do self assessment?
This is often done to ensure that the hospital’s patients are recovering at a steady pace. However, patients are often encouraged to undergo a self-assessment using a self-assessment form to help the patient develop their psychological recovery as well.
What is a patient assessment form?
A Patient Assessment Form is a form used by healthcare professionals which usually contains questions related to a patient’s health, medical condition, ailments, pain level, religious beliefs, among other things, that might impact a medical treatment, as well as a patient’s medical history. Related:
Why is physical assessment important?
The Advantages of Conducting Physical Assessments: Allows your doctor to detect any possible conditions that could possibly affect your physical performance. This then gives you the opportunity to get rid of or periodically maintain these ailments.
What are the head, eyes, and ears checked for?
Head, Eyes, Ears. The head, eyes, and ears are then checked for any abnormality in their size, shape, symmetry, or acuity , as well as surprising observations to the eyelids, lacrimal glands, conjunctiva, visual fields, peripheral vision, sclera, etc. or hearing problems.
What is a medical history template?
The template is used by patients to register medical history through providing their personal information, weight, allergies, illnesses, operations, healthy habits, unhealthy habits. You can integrate the data to your own systems.
What information can be collected through a hospital registration form?
Through the Hospital Patient Registration Form, you can collect all necessary data of your patients' health related information as their name, birthday, health history, family doctor, emergency contact information and more.
What is patient registration?
Patient registration forms are used to register patients for procedures offered at medical facilities. Whether you need to register new patients for your hospital, clinic, health center, or private practice, our free Patient Registration Forms will streamline the registration and onboarding process by seamlessly gathering patient information online. Simply customize any of the free templates below to match your medical facility, and you’ll be registering new patients in no time! Patients will be able to provide their personal information, provide emergency contact numbers, write down their medical histories, attach files, and submit payments all at once. Submissions will be stored safely in your secure JotForm account, easy for you and your staff to access from any device.
What is a HIPAA medical history form?
HIPAA Medical History Form allows gathering patient's contact details with their current symptoms, medications, allergies, drug use, and family medical history that allows for a better healthcare service and management process. Healthcare Forms.
What is counseling intake form?
The Counseling Intake Form allows for an easier client registration process as it automates gathering information from your clients, reduces paperwork and helps to keep patient records in a systematic way.
Subjective
The subjective section of your documentation should include how the patient is currently feeling and how they’ve been since the last review in their own words.
Objective
The objective section needs to include your objective observations, which are things you can measure, see, hear, feel or smell.
Assessment
The assessment section is where you document your thoughts on the salient issues and the diagnosis (or differential diagnosis), which will be based on the information collected in the previous two sections.
Plan
The final section is the plan, which is where you document how you are going to address or further investigate any issues raised during the review.
Why do we need a medical assessment form?
Medical Assessment Form template provides information by medical establishments to record the results of the assessment. The meant organization will then draw knowledge from the details and collate that knowledge for analysis.
What is a health assessment?
Health assessment is the analysis of the health standing by activity a physical test when taking health history into consideration.
What is a housing medical assessment?
A person who is applying for housing would additionally bear a housing medical assessment. This helps to seek out a house compatible with him. Any unhealthiness or incapacity would get to be thought about discarding that idea and getting a new one. Use this template to assess all these kinds of loopholes and developing a concrete housing medical assessment.
What is standardized medical council assessment form?
The use of standardized medical council assessment forms is for establishments and organizations that give health services. If you’re a hospital manager or the administrator of any health services supplier, you ought to create it your goal to make a decent health assessment model form.
What information should be included in a health assessment template?
Lastly, another piece of information that should be included in a health assessment template is the attending physician’s (or any healthcare personnel’s) name, designation, signature. Doing this legitimizes the entire assessment process. It also helps ensure that a qualified personnel made the health assessment and came up with a medical diagnosis which the patient will be treated for. You may also see sample assessment templates.
Why use a health assessment template?
Another reason why it makes sense to create and use a standard health assessment template for your hospital or clinic is that it is required by most governments and organizations that overlook the health services sector. If you are already looking to create the most comprehensive and useful health assessment tool for your organization, it makes sense to ensure that this new health assessment template is also compliant to different standards set by the government. You may also see risk assessment form templates.
What are some examples of health assessment forms?
Examples include hospitals, clinics, health spas, mental health institutions, traditional and alternative medicine clinics, rehabilitation centers, emergency rooms. And when health assessment forms are used by these health institutions or organizations, they will often follow a standard template format.
What is the process of evaluating an individual's current health status through detailed health history taking?
A health assessment is a process of evaluating an individual’s current health status through detailed health history taking and the use of physical inspection, palpation, percussion and auscultation (hearing breath and heart sounds).
Why use a standard health assessment tool?
5. To protect self and institution against medical malpractice lawsuits. Another often-overlooked benefit of using a standard health assessment tool for any health service provider is that they may be used to protect the hospital and its employees from an medical malpractice or negligence lawsuits.
Is patient information confidential?
One key rule to remember when designing a health assessment form is that any information provided or shared by the patient is confidential according to the law. The specific implementing rules for your county or state’s privacy laws may differ but, for the most part, patient information is always confidential.
Who does a health assessment?
Health assessments are usually done by a licensed physician or anyone who is part of the healthcare team like nurses, surgeons, consultants, etc). The findings of a health needs assessment are usually written in a health assessment form or template. As its name implies, health assessment templates are typically used in the healthcare setting.
What should be indicated in the assessment report?
The patient’s blood pressure, temperature, and pulse rate should also be indicated in the assessment report. Know the patient’s mental state. Patients with different illnesses are most likely to have different moods. State the mood swings of the patient, hygiene, posture and how he remembers things.
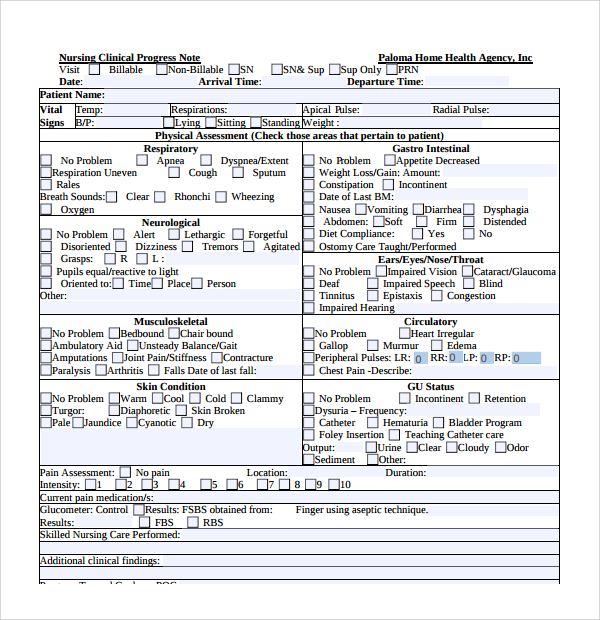
What is a nursing assessment form?
Nursing Assessment Forms are used to state the observations and the suggestions from a nurse to a patient’s health status. The nurse is expected to use accurate medical terms and detailed explanations for their measured examination.
What is a nursing need assessment decision record?
Nursing Needs Assessment Decision Record Form – this serves as a document wherein the nurse will state what form of procedure that the doctor decided in line with the assessment records.
What is a nurse assistant?
The nurse serves as an assistant to everything that the doctor will do, from assisting a patient to sit up to assisting the doctor during surgery procedures. Throughout time, the professional field has required all employed individuals to be assessed for ranking, and this includes a nursing assessment or evaluation.
Why is it important to complete a nursing assessment form?
It is important to complete a nursing assessment form to have a full understanding of what the patient is facing and what he will be needing in the future. The form will vary depending on the state of the patient regarding his illness, medical record and the facilities that he may be using.
What happens if there is no improvement in the patient's condition?
If there are no improvement in the patient’s condition, the nurse will be requested to repeat the process from the assessment phase again. Nurses must achieve familiarity with the five common steps since one skipped phase may result in an unexpected patient condition.
How to assess a patient with a nursing monitoring form?
Medical centers may differ in their patient protocols but there are common steps in assessing a patient with the help of a Nursing Monitoring Form: Have the patient’s medical records. This includes the patient’s medical history and the details of his previous admission. Do an initial interview.
What is a physical therapy assessment form?
A physical therapy assessment form is a document which is used by physical therapists for their patients and clients. The form can be used for initial assessments and final assessments in determining a patient’s medical history as well as the patient’s therapy progress. On the other hand, physical therapy assessment forms can also be used by physical therapy students and teachers for them to identify areas to be corrected in lieu of the course or program that they plan to accomplish as part of their education.
What is the first section of a medical assessment form?
The first section or part of the form is for indicating the date when the assessment was taken by the patient, the patient’s number and name, the diagnosis of the patient and the name of the referring person, the billable units of the patient, and the patient’s time in an out in the medical center or clinic.
What is a musculoskeletal assessment form?
A physical therapy musculoskeletal assessment form is the document to be used by a therapist or a physician who is observing and assessing the athlete. Basically, in the form, the patient’s posture and reliability will be the areas to be assessed by the therapist by using a rating scale or scoring method.
What is the first section of a therapist assessment?
The first section or part of the form is for indicating the date when the assessment was taken by the patient, the patient’s number and name, the diagnosis of the patient and the name of the referring person, the billable units of the patient, and the patient’s time in an out in the medical center or clinic. Then, a patient information section will be the next portion to be completed which is basically for the patient’s profile, complaints, medication and allergies, activities and occupation, and the goals of the patient during his therapy. After which, the systems review of the therapist for the patient will be the focus of the third section of the form while the fourth section enlists the tests and measures of the patient, the fifth section is allotted for the therapist’s evaluation, the sixth section explains the intended plans for caring for the patient, and the seventh section of the form is where an informed consent statement is incorporated for documenting that the patient and his legal guardian were informed of all the treatments and tests conducted by the therapist for the purpose of the assessment.
What is the table in a physical therapy lymphedema assessment form?
The table is for the reviews of the patient’s system, and the diagrams are for labeling purposes for the patient’s pain assessment and swelling location.
Why do physical therapists measure their patients?
Patient physical dimensions –Physical therapists need to measure their patients in order to further obtain information about the patient’s physique. Some of the parts to be measured includes the patient’s head and whether it is flexed or extended, as well as the patient’s shoulders and knees.

Popular Posts:
- 1. pmc patient portal not working
- 2. cigna carecentrix patient portal
- 3. how to create a hipaa secure patient portal
- 4. japanese brain patient spect report
- 5. united surgical associates patient portal
- 6. www valleymedicalgroup patient portal ridgewood nn
- 7. www.lawrenceville-doctors.com/patient portal
- 8. patient ability to report complaints
- 9. patient portal children's clinic
- 10. sanvello patient portal