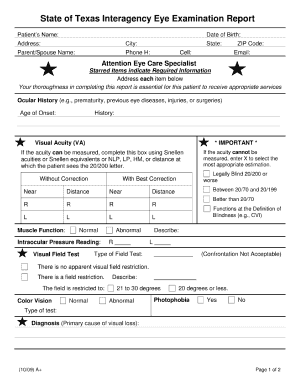
Patient Acuity Form - Fill and Sign Printable Template …
8 hours ago Get the Patient Acuity Form you need. Open it using the cloud-based editor and begin altering. Fill the empty areas; engaged parties names, places of residence and numbers etc. Customize the template with unique fillable fields. Add the day/time and place your e-signature. >> Go To The Portal
What do research reports tell us about patient acuity?
First, most of the research reports are about developing or comparing instruments to measure patient acuity.
How do you score a patient based on acuity?
The tool uses both clinical patient characteristics and workload indicators to score patients from 1 to 4 based on acuity level. This approach gives nurses the power to score their patient, then report to the charge nurse so that RN assignments for the oncoming shift are quantifiable and equitable.
What is the patient acuity tool?
The patient acuity tool addresses the important issue of unbalanced nurse-patient assignments and helps nurses influence decision-making in their organizations. Patient assignments can lead to dissatisfaction among nursing staff, especially when they’re not consistent, objective, and quantifiable.
What is acuity assessment in nursing?
Definition. The levels of patient acuity equate to the number of hours needed for nursing staff to care for the offender's physical and mental health needs, therefore acuity assessment is a nursing function.
How would you describe patient acuity?
Patient acuity is generally defined as a measurement of intensity of nursing care needed by a patient. For the proper development of a staffing plan for people receiving hospital care, patient acuity is a particularly critical benchmark.
What does acuity mean in nursing?
Definition. The levels of patient acuity equate to the number of hours needed for nursing staff to care for the offender's physical and mental health needs, therefore acuity assessment is a nursing function.
How is Acuity calculated?
Acuity Targets and Average Acuity Calculations in Reports The sum of each completed assessment's acuity level is divided by the total number of completed assessments. The average acuity level for the report time interval is calculated using the level of completed assessments and the location's default acuity level.
What makes a patient high acuity?
In general, patients requiring a greater degree of observation and intervention from nurses receive a higher acuity rating. While high-acuity patients are typically sicker, other factors can change a patient's acuity ranking.
What is low patient acuity?
The outcomes of interest were low acuity presentation, defined as those who self-presented (were not transported by ambulance), were assigned a triage category of 4 or 5 (semiurgent or non-urgent) and discharged back to usual residence from ED.
What is another word for acuity?
In this page you can discover 18 synonyms, antonyms, idiomatic expressions, and related words for acuity, like: sharpness, acuteness, keenness, visual acuity, sharp-sightedness, giftedness, longheadedness, longsightedness, perspicaciousness, quick-wittedness and sharp-wittedness.
What health condition is Acuity 1?
1. Acuteness (see acute [def. 2]); the level of severity of an illness.
What is acuity level 3?
Level 3: Urgent – Serious conditions that require emergency intervention. Level 4: Less urgent – Conditions that relate to patient distress or potential complications that would benefit from intervention.
How do you categorize a patient?
Categorization of patients contains overall data on the patient condition reviewed through 16 risk factors: assessment of patient autonomy (hygiene, dressing, feeding and elimination), assessment of patient physi- cal activity (walking, standing, sitting, moving and turning), assessing patient risk of falling, ...
What is a medium acuity patient?
A medium-acuity patient is defined as a patient who requires active monitoring or management and in whom all the following apply: 1. The patient does not meet the criteria of an emergency patient.
How you can fill out the Nursing 100 fill in worksheet form online
To begin the document, utilize the Fill & Sign Online button or tick the preview image of the blank.
How to calculate patient acuity
Find a suitable template on the Internet. Read all the field labels carefully. Start filling out the blanks according to the instructions:
Instructions and help about Patient Acuity Worksheet
hello I'm a nursing people it slays welcome back to my channel today we're gonna talk all about the nursing brain and the report sheet something that I have had so many student nurses and people have precepted and just new nurses asked how on earth do I keep track of this chaos when you have five or so patients it gets to be a lot but having an organized report sheet is going to save your life so if you're like me you have to write absolutely everything down otherwise it's not going to get done and I finally come up with a way that kind of condenses all that information into an organized pallet that I can then work off of and cross things off when I'm done because I'm also super type-a and I love crossing things out so if you're looking for something that can kind of give you a overview in your entire day you can hold up to four patients on one piece of paper if you have five you kind of have to staple two together and you get to cross a lot of things off and this is for you okay so he.
FAQs
Here is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
What is the right way to fill out Two-Earners Worksheet tax form?
Wages, in this context, are what you expect to appear in box 1 of your W-2.The IRS recommends that the additional withholding be applied to the higher-paid spouse and that the lesser-paid spouse should simply claim zero withholding allowances, as this is usually more accurate (due to the way that withholding is actually calculated by payroll programs, you may wind up with less withheld than you want if you split it)..
For the new 2018 W-4 form, do I also print out the separate A-H worksheet and fill that out for my employer?
No, an employee is not required to give the separate worksheet to the employer. Keep it for your own records.
Which one is correct, "fill in a form" or "fill out a form"?
In terms of outcome, they mean the same thing. Usage, at least in my Canadian neighbourhood, varies depending on how specific the circumstance is. [Clerk hands you a blank form.]Here, fill in this form.Here, fill this out.
What are the benefits of acuity tool?
Benefits. Given the original concern by staff that assignments were unequal, one of the strengths of this acuity tool is that it allows nurses to become stakeholders in making patient assignments. In addition, it also gives the charge nurse an objective way to justify assignment rationale.
What scale is a patient on?
Each patient is scored on a 1-to-4 scale (1, stable patient; 2, moderate-risk patient; 3, complex patient; 4, high-risk patient) based on the clinical patient characteristics and the care involved (workload.) Each nurse scores his or her patients, based on acuity, for the upcoming shift and relays this information to the charge nurse, who then assigns patients before the shift change. The handoff report between RNs allows each to validate patients’ current acuity and care needs. (See Patient acuity tool .)
What is the goal of the patient safety tool?
The goals of the tool are to: increase nurse satisfaction with their patient assignment. increase nurse perception of patient safety by assigning patients with high acuity scores equitably.
Why do nurse assignments change every 4 hours?
Sometimes patient assignments changed every 4 hours because of differences in nurse shift length, which left the staff with no consistent communication between shifts. The charge nurse would also occasionally take a patient assignment when patient acuity was high and RN census was low, resulting in outliers in data.
Why is patient acuity important?
The patient acuity tool addresses the important issue of unbalanced nurse-patient assignments and helps nurses influence decision-making in their organizations. Patient assignments can lead to dissatisfaction among nursing staff, especially when they’re not consistent, objective, and quantifiable.
How to determine the equality of nurses' assignments within a shift?
To determine the equality of nurses’ assignments within a shift, the difference in total acuity between the highest and lowest scoring assignments was obtained . (See RN assignments using acuity tool .)
Who is Jennifer Powell?
Jennifer Powell is a neonatal intensive care unit nurse at Novant Health Hemby Children’s Hospital in Charlotte, North Carolina. Editor’s note: The authors grant permission for using the tool in the article provided they are credited as the source.
Use A Tool For Consistent, Objective, and Quantifiable Patient Assignments.
Purpose and Goals
- We used evidence-based information to create an objective acuity tool to establish patient assignments. The tool uses both clinical patient characteristics and workload indicators to score patients from 1 to 4 based on acuity level. This approach gives nurses the power to score their patient, then report to the charge nurse so that RN assignments for the oncoming shift are quant…
The Patient Acuity Tool
- Each patient is scored on a 1-to-4 scale (1, stable patient; 2, moderate-risk patient; 3, complex patient; 4, high-risk patient) based on the clinical patient characteristics and the care involved (workload.) Each nurse scores his or her patients, based on acuity, for the upcoming shift and relays this information to the charge nurse, who then assi...
Methodology
- Anecdotal reports by the RN staff and our observations prompted the collection of data from staff. Some of the staff comments about the current system included: 1. “Why are my patient assignments so unfair?” 2. “How will I care for all of my patients effectively?” 3. “Involved care is a subjective term.” We conducted a literature review and eventually combined two existing tools a…
Data
- At the end of the pilot study, we reviewed patient assignments before and after implementing the acuity tool to assess their equality, and we surveyed RNs about the two goals we set for the project: improve nurse satisfaction and increase nurse perception of patient safety.
Equality of Patient Assignments
- To determine the equality of nurses’ assignments within a shift, the difference in total acuity between the highest and lowest scoring assignments was obtained. (See RN assignments using acuity tool.) Before implementing the acuity tool, the average distribution of total acuity between highest and lowest nurse assignments for each shift was 4.83 (using a scale of 1 = lowest acuit…
Challenges
- We attributed many of the challenges faced during the implementation of this project to staff assignment changes during some 24-hour periods. Sometimes patient assignments changed every 4 hours because of differences in nurse shift length, which left the staff with no consistent communication between shifts. The charge nurse would also occasionally take a patient assign…
Benefits
- Given the original concern by staff that assignments were unequal, one of the strengths of this acuity tool is that it allows nurses to become stakeholders in making patient assignments. In addition, it also gives the charge nurse an objective way to justify assignment rationale. The tool costs no money to implement and requires no special technology. In addition, it’s noninvasive t…
Striking A Balance
- The patient acuity tool addresses the important issue of unbalanced nurse-patient assignments and helps nurses influence decision-making in their organizations. Our research found that an objective patient acuity tool on a medical-surgical floor could increase assignment equality, improve nurse satisfaction, and improve nurse perception of patient safety. The tool is now bein…
Selected References
- Chiulli KA, Thompson J, Reguin-Hartman KL. Development and implementation of a patient acuity tool for a medical-surgical unit. Academy of Medical-Surgical Nurses. 2014;23(2):1, 9-12. Kidd M, Grove K, Kaiser M, Swoboda B, Taylor A. A new patient-acuity tool promotes equitable nurse-patient assignments. American Nurse Today. 2014;9(3):1-4.
Popular Posts:
- 1. dr. robert louis patient portal
- 2. stockton cardiology patient portal
- 3. natesan medical group patient portal
- 4. derry medical patient portal login
- 5. ortho montana billings mt patient portal
- 6. healthpartners login patient
- 7. ecri report and policy on use of patient owned equipment
- 8. dr lipinski patient portal
- 9. brandon hospital/patient portal
- 10. health assessment report of sickle cell crsisi patient