10+ SAMPLE Nursing Incident Report in PDF
33 hours ago A Nursing Incident Report is a document may it be a paper or a typewritten one that provides detailed information and account of the chain of events leading up to and following an unforeseen circumstance in a healthcare setting or facility especially in the nursing side. ... like for example a patient, a significant other, or even a nurse ... >> Go To The Portal
Consider the following examples as situations in which an incident report should be filed:
- You’re working as a nurse on an acute inpatient psych unit when one of the patients begins to act violently and attacks...
- You’re ambulating a patient in the hallway and securely holding onto their gait belt when the patient abruptly falls to...
Full Answer
What is an example of an incident report?
If there is an injury, illness or damage as a result of the hazard, that is an incident and should be reported as such. For example… If no one changes a burned out lightbulb leading to dimly lit conditions in an area, that is a hazard.
What is a fall incident report?
The report states a landing zone was established along Charleston Highway and Murdaugh was airlifted to what SLED later revealed was Memorial Health University Medical Center in Savannah, Georgia. There, he was treated for a superficial gunshot wound to the head, according to SLED.
What is a patient incident report?
The incident involves only patients of Planned Parenthood Los Angeles, which operates 21 health centers in the Southern California city, the agency said in a statement on its site.
What is a nurse incident report?
An incident report is a document that describes an accident or incident that deviates from safe nursing standards. Nurses want to exercise utmost care with their work, but accidents do happen and when they do, an incident report needs to be filed.
How do you write a nursing fall incident report?
What Information Do You Put in an Incident Report?Detailed description of the event with events listed chronologically.Witnesses or injured party statements.Injuries sustained by the person(s) as a result of the incident or the outcome.Actions taken immediately after the incident occurred.Treatments administered.More items...•
How do you write a patient incident report?
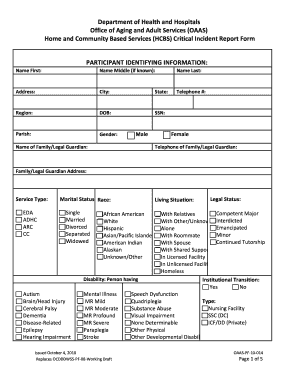
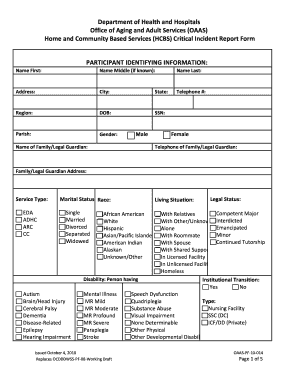
What to Include In a Patient Incident ReportDate, time and location of the incident.Name and address of the facility where the incident occurred.Names of the patient and any other affected individuals.Names and roles of witnesses.Incident type and details, written in a chronological format.More items...•
How do I document a fall incident report?
What Does an Incident Report Need to Include?Type of incident (injury, near miss, property damage, or theft)Address.Date of incident.Time of incident.Name of affected individual.A narrative description of the incident, including the sequence of events and results of the incident.Injuries, if any.More items...•
How do you write a nursing patient report?
How to write a nursing progress noteGather subjective evidence. After you record the date, time and both you and your patient's name, begin your nursing progress note by requesting information from the patient. ... Record objective information. ... Record your assessment. ... Detail a care plan. ... Include your interventions.
What are the examples of incident?
The definition of an incident is something that happens, possibly as a result of something else. An example of incident is seeing a butterfly while taking a walk. An example of incident is someone going to jail after being arrested for shoplifting.
What are the 4 types of incident reports?
Common Types of Incident ReportsWorkplace. Workplace incident reports detail physical events that happen at work and affect an employee's productivity. ... Accident or First Aid. ... Safety and Security. ... Exposure Incident Report.
What should an incident report include?
8 Items to Include in Incident ReportsThe time and date the incident occurred. ... Where the incident occurred. ... A concise but complete description of the incident. ... A description of the damages that resulted. ... The names and contact information of all involved parties and witnesses. ... Pictures of the area and any property damage.More items...•
What makes a good incident report?
Effective Incident Reports identify the facts and observations. They avoid inclusion of personal biases; they do not draw conclusions/predictions, or place blame. Effective Incident Reports use specific, descriptive language and identified the action(s) taken by staff as a result of the unusual incident.
How do I create an incident report template?
Incident Report TemplateIdentify the type of incident and provide details of person of injury, job and hazard/incident.Take or attach photo evidence of incident, environment, person(s) involved.Gather witness statements and capture digital signature.Sign off with digital signature of person reporting.
What should a nursing report include?
What to cover in your nurse-to-nurse handoff reportThe patient's name and age.The patient's code status.Any isolation precautions.The patient's admitting diagnosis, including the most relevant parts of their history and other diagnoses.Important or abnormal findings for all body systems:More items...•
What is an incident report in nursing?
An incident report in nursing is a report which details an event where a person is injured, or property is damaged. If these conditions occur on medical facility property, completion of an incident report is necessary.
How do you give a good report?
3:2220:45How to Give a Nursing Shift Report - YouTubeYouTubeStart of suggested clipEnd of suggested clipFirst I have right here is attending doctor as the nurse you need to know who is the attendee overMoreFirst I have right here is attending doctor as the nurse you need to know who is the attendee over that patients care of the doctor.
What to Expect After Writing an Incident Report?
Information in the nursing incident report will be analyzed and comprehended to identify the root cause of the incident. This is subject to changes...
What Do I Need to Tell the Patient and the Patient’s Family?
Educate the patient or the significant other on what to expect regarding the incident report. Impart an explanation when results of some procedures...
Do you dread writing a nurse incident report?
Now, that depends on the person writing it. Stressing over getting the report done or about what to include are common concerns for nurses. Always...
What is a nursing incident report?
A nursing incident report is a kind of report that a nurse or any health care worker writes to report an incident. This report gives a good bird's...
Why is it so important to write about the incident in detail?
The reason it is necessary to write the incident in detail is to make sure that you have written out what really happened. Not fabricating anything...
What is something that should be avoided when writing a nursing incident report?
Forgetting to place the evidence or the proof of what happened. As well as not rearranging in chronological order as to how it happened. Details ar...
What Is a Nursing Incident Report?
We know what an incident report is and what it looks like. But do we have any idea as to what a nursing incident report is and what it looks like? Is there even any difference between these two kinds of reports? A nursing incident report is a kind of report that is filled out by nurses or anyone in the health care or medical field.
How to Write a Nursing Incident Report?
Being able to know what can and cannot be written in a nursing incident report is important. Take note that this document is a formal written report, and must be treated as such all the time. So to not make any mistakes when writing your incident report, here are five simple tips to guide you when you are writing your nursing incident report.
What is a nursing incident report?
A nursing incident report is a kind of report that a nurse or any health care worker writes to report an incident. This report gives a good bird’s eye view of how the incident happened and what can be done to resolve it.
Why is it so important to write about the incident in detail?
The reason it is necessary to write the incident in detail is to make sure that you have written out what really happened. Not fabricating anything in the report and to make sure that anyone who was there is also aware of what happened. That they can assure the one reading your report that it really happened.
What is something that should be avoided when writing a nursing incident report?
Forgetting to place the evidence or the proof of what happened. As well as not rearranging in chronological order as to how it happened. Details are an important part of the incident report.
What is incident report?
An incident report is an electronic or paper document that provides a detailed, written account of the chain of events leading up to and following an unforeseen circumstance in a healthcare setting.
Why are incident reports important?
Incident reports are used to communicate important safety information to hospital administrators and keep them updated on aspects of patient care for the following purposes: Risk management. Incident report data is used to identify and eliminate potential risks necessary to prevent future mistakes.
How long does it take to complete an incident report?
To ensure the details are as accurate as possible, incident reports should be completed within 24 hours by whomever witnessed the incident. If the incident wasn’t observed (e.g., a patient slipped, fell, and got up on his own), then the first person who was notified should submit it.
What are some examples of reportable events in New York?
Examples: adverse reactions, equipment failure or misuse, medication errors.
What are the concerns of nurses?
Stressing over getting the report done or about what to include are common concerns for nurses — not to mention worrying about whether filing the report reflects badly on your performance. Mistakes happen all the time, and healthcare facilities are not immune.
What is the third leading cause of death in the U.S.?
According to a 2016 study conducted by Johns Hopkins, medical errors have become the third-leading cause of death in the U.S. and threaten the safety and well-being of patients. As time-consuming as incident reports may be, their role in patient care cannot be ignored.
What Is Patient Incident Report?
Incidents are potentially dangerous incidents that have the potential to put patients or staff members at risk. Medical events are anything that can happen in the healthcare industry and can be caused by anything from equipment failure to injuries to poor patient care. Medical events can occur for a variety of reasons.
What Is the Purpose of the Patient Incident Report?
Patient incident reports provide information to facility officials about what happened to the patient. The information provided in the reports provides light on the steps that must be performed in order to deliver excellent patient care while also maintaining the smooth operation of your facility.
What to Include in a Patient Incident Report?
A patient incident report should include the bare minimum of information regarding the occurrence, such as who was involved, what happened, where it happened, when it happened, and how it happened. You should also include ideas on how to deal with the problem in order to lessen the likelihood of further instances occurring.
What Are the Benefits of Patient Safety Reporting?
Setting the relevant key performance indicators in your organization gets easier as a result of healthcare data analysis and analysis. You can receive the following significant advantages from filing a complaint:
Types of Incident Report
Even if an occurrence appears to be insignificant or has not resulted in any harm, it is still crucial to record it. Whether a patient has an allergic response to a drug or a visitor slips over an electrical cord, these occurrences provide valuable insight into how your facility can create a better, more secure environment for its visitors.
How to Create an Efficient Patient Incident Report
One thorough incident report should address all of the fundamental questions — who, what, where, when, and how — and provide full answers. The majority of hospitals adhere to a predetermined reporting format that is tailored to their own organizational requirements. An incident report, on the other hand, must include the following information:
FAQs
It is possible to acquire information on patient safety occurrences through the use of incident-reporting systems (IRSs). Even if they come with a significant financial cost, however, little is known regarding their usefulness.
What to include in an incident report?
Every facility has different needs, but your incident report form could include: 1 Date, time and location of the incident 2 Name and address of the facility where the incident occurred 3 Names of the patient and any other affected individuals 4 Names and roles of witnesses 5 Incident type and details, written in a chronological format 6 Details and total cost of injury and/or damage 7 Name of doctor who was notified 8 Suggestions for corrective action
Why do we use resolved patient incident reports?
Using resolved patient incident reports to train new staff helps prepare them for real situations that could occur in the facility. Similarly, current staff can review old reports to learn from their own or others’ mistakes and keep more incidents from occurring. Legal evidence.
Why is it important to review patient incidents?
Reviewing incidents helps administrators know what risk factors need to be corrected within their facilities , reducing the chance of similar incidents in the future.
Why is it important to know that an incident has occurred?
Knowing that an incident has occurred can push administrators to correct factors that contributed to the incident. This reduces the risk of similar incidents in the future. Quality control. Medical facilities want to provide the best care and customer service possible.
How long does it take to file a patient incident report?
Patient incident reports should be completed no more than 24 to 48 hours after the incident occurred.
Why is it important to document an incident?
Even if an incident seems minor or didn’t result in any harm, it is still important to document it. Whether a patient has an allergic reaction to a medication or a visitor trips over an electrical cord, these incidents provide insight into how your facility can provide a better, safer environment.
How many hospital incidents go unreported?
According to a study by the US Department of Health and Human Services, 86 per cent of hospital incidents go unreported. Even more staggering, though, is the reason behind this. Staff did not consider 62 per cent of incidents as reportable, due to unclear incident reporting requirements.
What is critical incident?
A case study of a critical incident based on a hospital fall of an elderly patient with memory problems who has had several falls at home and has been admitted to a community hospital for assessment.
What is a fall in a Commodore?
A fall is defined as an unexpected, involuntary loss of balance by which a person comes to rest at a lower or ground level (Commodore 1995). The older population is growing in number, and falling is common in this group.
How old is Patient A?
Patient A is a 77 year old female who is in frail health. She has experienced numerous falls at home and is showing symptoms of dementia. Patient A was admitted to a general hospital because her diabetes was extremely unstable.
Why is the term "fall" considered contentious?
It is debated that the term “fall” is now considered contentious because those who fall are perceived quite negatively as old, frail and dependent (DoH 2001).
Can a fall cause physical injury?
Even if falls do not cause physical injury, the psychological effect can be long-lasting. “Post-fall syndrome” results in hesitancy and a loss of confidence leading to loss of mobility and independence (Cannard 1996). Arguably, this can cause shame and unwillingness to admit to falls.
Can dementia cause increased risk of falling?
However, for older people with cognitive impairment or dementia, changes in mood, memory and thought processes in addition to changed physical health can result in increased risk and vulnerability that includes an increase in the potential for falling, as in the case of patient A (Oliver et al 2007).
What are healthcare incidents, and what causes them?
A healthcare incident refers to an unintended or unexpected event that harms a patient or caregiver—or has the potential to harm them. Incidents or errors occur for various reasons or root causes, such as system design flaws, lack of administrative oversight, poor training, digression from protocols, miscommunication, and more.
What are examples of incidents in healthcare?
Unfortunately, one doesn’t need to look far to find examples of incidents in healthcare. That’s because the industry is incredibly complex and fast-paced. It’s easy to make honest mistakes. For example:
What are the most commonly-reported hospital incidents?
Medication-related incidents are the most commonly reported incidents in healthcare. This includes administering the wrong dose, giving medication to the wrong patient, or omitting the dose.
Incidents: Insight to patient safety risks
Learning why incidents occur can help organizations make improvements to prevent them from happening again. But first, the healthcare system must prioritize incident reporting by providers, staff, and patients. In fact, risk management and patient safety rely on healthcare’s collective:
Are there incident severity levels?
The World Health Organization (WHO) classifies healthcare incidents according to the levels of severity (i.e., mild, moderate, severe, or death) based on the severity of the symptoms or loss of function, the duration of the symptoms, and/or the interventions required as a result of the incident.
What is incident management?
Incident management refers to the process of analyzing incidents and identifying the causes. Incident management entails more than simply filling out an incident report to track events and prevent them from occurring again. Incident management is also increasingly about handling data for quality improvement that affects reimbursement.
The symplr approach
Preventable harm will continue to occur unless organizations take a proactive approach to mitigate risk. That’s where symplr can help. symplr’s patient safety and risk management software is a structured digital event management system that captures (near) incidents, provides analytics, manages workflows, and monitors improvements.
Popular Posts:
- 1. lehigh medical group patient portal
- 2. middlesex family practice patient portal
- 3. patient portal ogden regional
- 4. revolution patient portal
- 5. ahc patient portal
- 6. south point family practice belmont nc patient portal
- 7. north georgia diabetes patient portal
- 8. tenet tennessee st francis partners patient portal
- 9. community radiologists patient portal
- 10. st peters university hospital patient portal