Understanding Your Pathology Report: Colon Cancer
27 hours ago · The report is broken down into a few sections and may include: Demographic information about the patient: name, birthdate, medical record number, presumed diagnosis (if known), name... Description of the procedure and how/from where the specimen was obtained. Gross description: what the specimen ... >> Go To The Portal
Medication
Key Points 1 Colon cancer is a disease in which malignant (cancer) cells form in the tissues of the colon. 2 Health history affects the risk of developing colon cancer. 3 Signs of colon cancer include blood in the stool or a change in bowel habits. 4 Tests that examine the colon and rectum are used to detect (find) and diagnose colon cancer.
Procedures
You will probably never meet the pathologist, but samples of your colon tissue, removed during surgery or biopsy, will be sent to them for review. The pathologist prepares a report of their findings. This is called the pathology report.
Therapy
Meanwhile, there have been many changes in the pathologic diagnosis of colorectal cancer (CRC), pathologic findings included in the pathology report, and immunohistochemical and molecular pathology required for the diagnosis and treatment of colorectal cancer.
Nutrition
Signs of colon cancer include blood in the stool or a change in bowel habits. These and other signs and symptoms may be caused by colon cancer or by other conditions. Check with your doctor if you have any of the following: A change in bowel habits.
See more
How is colon cancer diagnosed?
What is a colon pathology report?
What are the recent changes in the pathologic diagnosis of colorectal cancer?
What are the signs and symptoms of colon cancer?
How do I read my cancer test results?
There are three possible results:Positive: Cancer cells are found at the edge of the margin. This may mean that more surgery is needed.Negative: The margins don't contain cancerous cells.Close: There are cancerous cells in the margin, but they don't extend all the way to the edge. You may need more surgery.
What is clinical presentation of colon cancer?
Because of increased emphasis on screening practices, colon cancer is now often detected before it starts to cause symptoms. In more advanced cases, common clinical presentations include iron-deficiency anemia, rectal bleeding, abdominal pain, change in bowel habits, and intestinal obstruction or perforation.
How do doctors know if someone has colon cancer?
Colon cancer can occur in any part of the colon. An examination of your entire colon using a long, flexible tube equipped with a camera (colonoscopy) is one way to detect colon cancer and polyps.
Where is colon cancer pain felt?
Many cases of colon cancer have no symptoms. If there are symptoms, the following may indicate colon cancer: Abdominal pain and tenderness in the lower abdomen.
What are usually the first symptoms of colon?
Diarrhea, constipation, or feeling that the bowel does not empty completely. General abdominal discomfort, such as frequent gas pains, bloating, fullness and/or cramps. Constant feeling of fatigue or tiredness.
What are the top 10 signs of colon cancer?
Signs of colon cancerBlood in stool. When blood is in your stool, it might look like bright red streaks or dark purplish clots. ... Change in stool frequency. ... Change in stool appearance. ... Rectal pain. ... Abdominal pain. ... Unintentional weight loss. ... Anemia. ... Fatigue or weakness.More items...
How does colon cancer start?
Most colorectal cancers start as a growth on the inner lining of the colon or rectum. These growths are called polyps. Some types of polyps can change into cancer over time (usually many years), but not all polyps become cancer. The chance of a polyp turning into cancer depends on the type of polyp it is.
Does colon cancer have pain?
“Colon cancer typically presents as a dull belly ache, if anything at all,” Dr. Ali says. In the more advanced stages of colon cancer, the pain may feel cramp-like or similar to bloat. Pain that is persistent and severe can be a sign of colon cancer and should never be overlooked.
What is meant by clinical presentation?
The constellation of physical signs or symptoms associated with a particular morbid process, the interpretation of which leads to a specific diagnosis.
What is the first stage of colon cancer?
Also known as carcinoma in situ, in this stage abnormal cells are only in the inner lining of the colon or rectum. Stage 1. The cancer has penetrated the lining, or mucosa, of the colon or rectum and may have grown into the muscle layer. It hasn't spread to nearby lymph nodes or to other parts of the body.
What are the symptoms of left sided colon cancer?
Abdominal symptoms such as pain, bloating or rectal bleeding are often signs of an abnormal process in the left side of your colon.
Which characteristic is a risk factor for colorectal cancer?
Lack of regular physical activity. A diet low in fruit and vegetables. A low-fiber and high-fat diet, or a diet high in processed meats. Overweight and obesity.
How many people died from colorectal cancer in 2017?
In 2014, there were an estimated 1.3 million people with colorectal cancer in the United States. It is estimated that in 2017, there will be 135,430 new cases diagnosed in the United States and an estimated 50,260 people will die of the disease. According to the NIH SEER program, rates of colorectal cancer have been declining approximately 2.7% each year over the past 10 years, with death rates declining by 2.5% each year (2005 - 2014)[3].
How old is the average person diagnosed with colorectal cancer?
Colorectal carcinoma is common; accounting for 15% of all newly diagnosed cancers, and tends to be a disease of the elderly, with the median age of diagnosis between 60 and 80 years of age, slightly younger for rectal carcinoma.
What is the second most common cancer in adults?
Colorectal Carcinoma (CRC) is commonest malignancy of the gastrointestinal tract and is the second most usually diagnosed cancer in adults, mainly at 6th to 7th decades of life[2]. CT and MRI are the modalities of choice used for staging.
What happens when a tumor is invasive?
Once a tumor is invasive, it can extend through the layers of the colonic wall and invade adjacent structures. Lymphatic, hematogenous, and peritoneal spread may also occur. The overall prognosis and outcome depend on the stage of the tumor at diagnosis.
What is clinical presentation?
Clinical presentation is typically sneaking, with altered bowel habit or iron deficiency anemia from chronic occult blood loss. Patient can present with symptoms of bowel obstruction, intussusception, heavy bleeding and metastatic disease. Sometime it is detected incidentally by CT done for other reason[1].
What is the survival rate of a patient with stage III chemo?
Adjuvant chemotherapy is reserved for stage III disease. Overall 5 year survival rate is 40 - 50%, with stage at operation the single most important factor affecting prognosis. In case of late presentation with acute obstruction or obstruction with perforation immediate surgery or intervention performed to relieve symptoms. For this patient treatment plan was resection and patient travel to home country for surgery.
Can a CT show a dilated colon?
Teaching point: Whenever patient present with pain and constipation or other relevant GI symptoms and X-ray shows dilated segment of colon with distal non-dilated colon an in adult patient colonic malignancy should be suspected and CT is recommended for better evaluation. Sometimes patient present late with obstructive colonic symptoms when Ileocecal junction is incompetent and we see dilated small bowel as well as colon.
What tests are needed for colon cancer?
Staging helps determine what treatments are most appropriate for you. Staging tests may include imaging procedures such as abdominal, pelvic and chest CT scans.
What is the procedure to check for colon cancer?
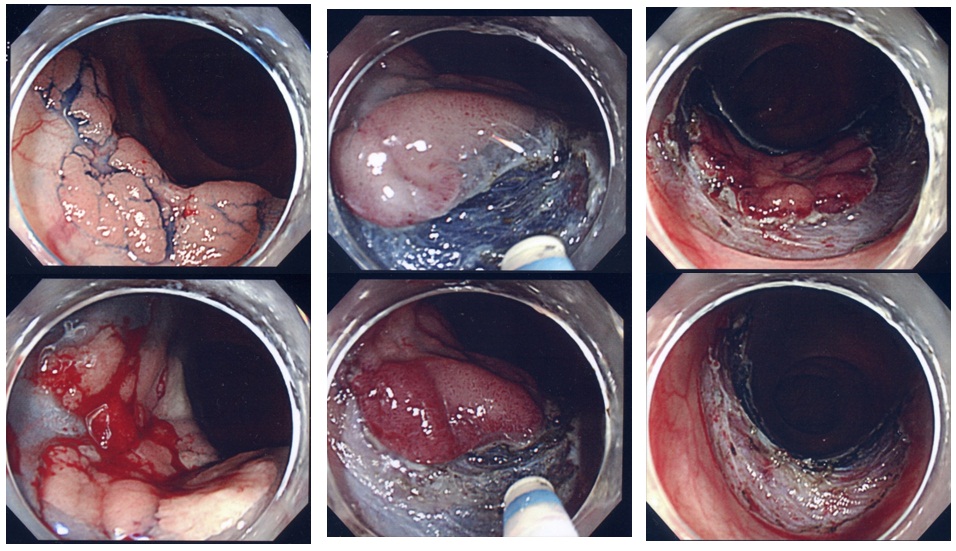
Colonoscopy. During a colonoscopy , the doctor inserts a colonoscope into your rectum to check for abnormalities in your entire colon. If your signs and symptoms indicate that you could have colon cancer, your doctor may recommend one or more tests and procedures, including:
How does chemotherapy help with colon cancer?
Chemotherapy uses drugs to destroy cancer cells. Chemotherapy for colon cancer is usually given after surgery if the cancer is larger or has spread to the lymph nodes. In this way, chemotherapy may kill any cancer cells that remain in the body and help reduce the risk of cancer recurrence.
What is the earliest stage of colon cancer?
At its earliest stage (stage 0), colon cancer is limited to the inner lining of your colon. As colon cancer progresses, it can grow through your colon and extend to nearby structures. The most advanced stage of colon cancer (stage IV) indicates cancer has spread to other areas of the body, such as the liver or lungs.
How to tell what stage of colon cancer you have?
The stages of colon cancer are indicated by Roman numerals that range from 0 to IV, with the lowest stages indicating cancer that is limited to the lining of the inside of the colon.
Why is chemotherapy used before surgery?
Chemotherapy might also be used before an operation to shrink a large cancer so that it's easier to remove with surgery.
How to make decisions about cancer?
Learn enough about your cancer to feel comfortable making treatment decisions. Ask your doctor to tell you the type and stage of your cancer, as well as your treatment options and their side effects. The more you know, the more confident you'll be when it comes to making decisions about your own care. Look for information in your local library and on reliable websites.
How do you know if you have colon cancer?
Signs and symptoms of colon cancer include: A persistent change in your bowel habits, including diarrhea or constipation or a change in the consistency of your stool. Rectal bleeding or blood in your stool. Persistent abdominal discomfort, such as cramps, gas or pain. A feeling that your bowel doesn't empty completely.
What are the treatments for colon cancer?
If colon cancer develops, many treatments are available to help control it, including surgery, radiation therapy and drug treatments, such as chemotherapy, targeted therapy and immunotherapy .
How does colon cancer start?
In general, colon cancer begins when healthy cells in the colon develop changes (mutations) in their DNA. A cell's DNA contains a set of instructions that tell a cell what to do.
What are the most common inherited diseases that cause colon cancer?
Only a small percentage of colon cancers are linked to inherited genes. The most common inherited syndromes that increase colon cancer risk are familial adenomatous polyposis (FAP) and Lynch syndrome, which is also known as hereditary nonpolyposis colorectal cancer (HNPCC).
How to reduce the risk of colon cancer?
Take steps to: Eat a variety of fruits, vegetables and whole grains. Fruits, vegetables and whole grains contain vitamins, minerals, fiber and antioxidants, which may play a role in cancer prevention.
What are the risk factors for colon cancer?
Risk factors. Factors that may increase your risk of colon cancer include: Older age. Colon cancer can be diagnosed at any age, but a majority of people with colon cancer are older than 50. The rates of colon cancer in people younger than 50 have been increasing, but doctors aren't sure why. African-American race.
Which race has the highest risk of colon cancer?
African-American race. African-Americans have a greater risk of colon cancer than do people of other races.
What is colon cancer?
Key Points. Colon cancer is a disease in which malignant (cancer) cells form in the tissues of the colon. Health history affects the risk of developing colon cancer. Signs of colon cancer include blood in the stool or a change in bowel habits. Tests that examine the colon and rectum are used to diagnose colon cancer.
How do you know if you have colon cancer?
Signs of colon cancer include blood in the stool or a change in bowel habits. These and other signs and symptoms may be caused by colon cancer or by other conditions. Check with your doctor if you have any of the following: A change in bowel habits. Blood (either bright red or very dark) in the stool.
How many lymph nodes does cancer spread to?
Cancer has spread to one to three nearby lymph nodes or cancer cells have formed in tissue near the lymph nodes; or. through the mucosa (innermost layer) of the colon wall to the submucosa (layer of tissue next to the mucosa). Cancer has spread to four to six nearby lymph nodes. Enlarge.
What are the risk factors for colon cancer?
Risk factors for colorectal cancer include the following: Having a family history of colon or rectal cancer in a first-degree relative (parent, sibling, or child). Having a personal history of cancer of the colon, rectum, or ovary.
Where does colon cancer spread?
Cancer has spread from the mucosa of the colon wall to the submucosa or to the muscle layer. In stage I colon cancer, cancer has formed in the mucosa (innermost layer) of the colon wall and has spread to the submucosa (layer of tissue next to the mucosa) or to the muscle layer of the colon wall.
How does cancer spread?
Cancer can spread through tissue, the lymph system, and the blood:
Where are abnormal cells found in the colon?
Abnormal cells are shown in the mucosa of the colon wall. In stage 0, abnormal cells are found in the mucosa (innermost layer) of the colon wall. These abnormal cells may become cancer and spread into nearby normal tissue. Stage 0 is also called carcinoma in situ.
Overview
Colorectal cancer often begins as a growth called a polyp inside the colon or rectum. Finding and removing polyps can prevent colorectal cancer. Explore the links on this page to learn more about colorectal cancer prevention, screening, treatment, statistics, research, clinical trials, and more.
Research
Clinical advances, research findings, and NCI programs that are leading to progress in finding and treating colorectal cancer.
Coping with Cancer
The information in this section is meant to help you cope with the many issues and concerns that occur when you have cancer.
What are lesions other than colorectal cancer?
When there are lesions other than colorectal cancer, such as separate adenomas, polyps, gastrointestinal stromal tumors, or inflammatory bowel disease, they can be denoted in this section.
What is the histologic classification of tumors?
Histologic classification of tumors is based on WHO classification (5th edition) [ 5 ]. Although most CRCs are “adenocarcinoma, not otherwise specified (NOS),” if there are other histologic variants, it is recommended to mention them separately. This is because some histologic variants may be associated with specific molecular alteration or patient prognosis [ 5, 7 ]. Representative histologic types of CRC described in WHO classification and AJCC 8th edition are shown in Table 1 [ 4, 5 ].
How is differentiation determined in a tumor?
Differentiation of tumors is determined by the area ratio of gland or tubule formation by tumor cells [ 7 ]. The degree of differentiation of the tumor is applicable to adenocarcinoma, NOS. This is because other histologic types show their own prognosis [ 7 ]. Recently, tumor differentiation has been shown to affect the prognosis of patients with mucinous adenocarcinoma [ 5, 18 ]. However, standardized tumor grading of mucinous adenocarcinoma has not been presented yet. Tumor grading is preferably performed using a two-tiered system with low-grade and high-grade [ 5 ]. In the 3-tiered grading system, tumor differentiation is graded as well differentiated (> 95% gland formation), moderately differentiated (50%–95% gland formation), or poorly differentiated (< 50% gland formation). The “well- and moderately differentiated” grades correspond to low-grade, while “poorly differentiated” corresponds to high-grade of the two-tiered grading system [ 5, 19 ].
Is CRC a cancer in Korea?
Colorectal cancer (CRC), which was the fourth most common cancer in Korea at the time, is now the second most common cancer in Korea. Meanwhile, there have been many changes in the pathologic diagnosis of CRC, such as the diagnostic criteria for carcinoma, and pathologic findings included in the pathology report [1,2].
Is CRC a molecular or immunohistochemical diagnosis?
Meanwhile, there have been many changes in the pathologic diagnosis of colorectal cancer (CRC), pathologic findings included in the pathology report, and immunohistochemical and molecular pathology required for the diagnosis and treatment of colorectal cancer.
Can superficial type be used to describe tumor morphology?
Superficial type is not recommended for describing tumor gross morphology, because superficial type could be defined by microscopic examination. Fungating/polypoid type can substitute most gross morphology of the previously established superficial type. Nevertheless, if superficial type is used, it should be applied to tumors that are confined to mucosa or submucosa and with tumor thickness of no more than two-fold thickness of adjacent mucosa. Other criteria for tumor gross types are the same as in the previous version. Fungating/polypoid, ulcerofungating, ulceroinfiltrative, and infiltrative gross types correspond to the Borrmann classification of gastric cancer.
Does the standardization report reflect colon cancer?
The existing standardization report does not reflect the recent changes in colon cancer diagnosis. There has been considerable demand for the revision of the standardized pathology report, which is used by many Korean pathologists.
What is Kelsey Hill's cancer?
Kelsey Hill. Adrenal Cancer with Metastasis to the Lungs and Liver . Kelsey was diagnosed with cancer of the adrenal gland, with multiple tumors that had metastasized to her lungs and liver—at 6 months old. Her parents declined all chemotherapy treatment and chose antineoplaston treatment instead.
What type of cancer did Mary Jo Siegel have?
Mary Jo Siegel was diagnosed with Stage IV Non-Hodgkin's Lymphoma in 1991. She refused to undergo chemotherapy, radiation, and a bone marrow transplant and chose Antineoplaston therapy instead. She has been healthy and cancer-free since 1996.
What kind of cancer did Susan Hale have?
Susan Hale was diagnosed with Glioblastoma Multiforme Grade IV brain cancer in May of 1997. After two surgeries, 6 weeks of radiation, and gamma knife radiation failed affect her cancer, she chose Antineoplaston treatment. After 4 months of treatment she has been healthy and cancer-free ever since. Medical Records.
Is Sophia a cancer patient?
Sophia was diagnosed with a deadly Pinealoblastoma brain cancer—at 10 months old. After surgeons were unable to remove the entire tumor, her parents declined all chemotherapy treatment and chose antineoplaston treatment instead. After six years of treatment, Sophia remains healthy and cancer-free. Medical Records.

Diagnosis
Treatment
Clinical Trials
Coping and Support
Preparing For Your Appointment
- Screening for colon cancer
Doctors recommend certain screening tests for healthy people with no signs or symptoms in order to look for signs of colon cancer or noncancerous colon polyps. Finding colon cancer at its earliest stage provides the greatest chance for a cure. Screening has been shown to reduce you… - Diagnosing colon cancer
If your signs and symptoms indicate that you could have colon cancer, your doctor may recommend one or more tests and procedures, including: 1. Using a scope to examine the inside of your colon (colonoscopy).Colonoscopy uses a long, flexible and slender tube attached to a vi…