Patient Portals: Considerations for Minors
34 hours ago Information about services provided to a minor for which the minor has the right to consent to treatment cannot be placed in a portal that can be accessed by a parent or guardian. A portal for a minor may include these services. Other circumstances? Deven McGraw 202-637-9800 x115 deven@cdt.org www.cdt.org/healthprivacy >> Go To The Portal
When to grant patient portal access solely to minors?
Information about services provided to a minor for which the minor has the right to consent to treatment cannot be placed in a portal that can be accessed by a parent or guardian. A portal for a minor may include these services. Other circumstances? Deven McGraw 202-637-9800 x115 deven@cdt.org www.cdt.org/healthprivacy
Can a patient portal be used for a parent?
The Medicaid program provides coverage to 27 million children under age 18 in the United States. According to the U.S. Surgeon General, while 11 percent of youth have been diagnosed with a mental illness, two-thirds of youth who have a condition are not identified and do not receive mental health service. Research by the National Institute on Mental Health found that half of all …
How can health care providers give parents access to minor medical records?
Medicaid Third Party Liability & Coordination of Benefits. Medicaid Eligibility Quality Control Program. Financial Management. Payment Limit Demonstrations. Disproportionate Share Hospitals. Medicaid Administrative Claiming. State Budget & Expenditure Reporting for Medicaid and CHIP. Provider Preventable Conditions.
Does Medicaid cover mental health services for children?
NC Medicaid is committed to ensuring providers have the resources to continue to serving Medicaid beneficiaries without interruption or delays due to the COVID-19 outbreak. NC Medicaid Ombudsman The NC Medicaid Ombudsman is a resource to help Medicaid beneficiaries learn more about NC Medicaid Managed Care, understand their rights and ...

How do I check my Medicaid status in Illinois?
If you aren't sure if your Medicaid coverage has been approved yet or if it is still active, you can check Manage My Case or call the state's Automated Voice Recognition System (AVRS) at 1-855-828-4995 with your Recipient Identification Number (RIN).
Is Texas children Health Plan Medicaid?
What is STAR? STAR is a Medicaid-managed care plan. This plan helps family members of any age. Texas Children's Health Plan offers STAR in more than 20 counties in the Jefferson and Harris Service Areas.
How do I change my child's Medicaid plan in Texas?
CHIP members: The Texas Medicaid program allows you to change your or your child's health plan. You can learn more by calling CHIP toll-free at 1-800-647-6558. During the first 90 days after you or your child are enrolled in a health plan, you can change to another plan once for any reason.
Is Medi-Cal and Medicaid the same?
Medi-Cal is California's part of a national health coverage program called Medicaid. Each state runs its own Medicaid program. The states have to follow certain national Medicaid rules, but they have flexibility in how they run their programs.
Can an 18 year old get Medicaid in Texas?
Age 18 or younger (Children up to age 20 may be able to get Medicaid in some cases). A pregnant woman of any age can apply for CHIP perinatal services or Medicaid for her unborn child. A Texas resident.
How long can a child stay on Medicaid in Texas?
Your child can stay on your family plan until they turn 26, or much longer if they still depend on you financially and have a disability that meets the qualifications for receiving SSI.
How can I change my Medicaid plan?
OnlineLog in to your Marketplace account.Choose your active application under "Your Existing Applications."Select "Report a Life Change" from the left-hand menu.Read through the list of changes, and click "Report a Life Change" to get started.Select the kind of change you want to report.More items...
What are the different Medicaid plans in Texas?
Medicaid Buy-In for Adults.Medicaid Buy-In for Children.Medicaid for Children & Adults with Disabilities.Medicaid for the Elderly & People with Disabilities.
How do I cancel my Texas Medicaid?
Contact the Texas Medicaid program at 800-252-8263. If you wish to cancel a child's Medicaid, call this program at 800-647-6558.
What is Medicaid called in California?
Medi-CalMedi-Cal is California's Medicaid health care program. This program pays for a variety of medical services for children and adults with limited income and resources. Medi-Cal is supported by Federal and state taxes.
What is the monthly income limit for Medi-Cal?
Medi-Cal does have the option to review an applicant's income on an annual basis. For a single adult, the monthly Medi-Cal income was $1,482. In 2022, the monthly income will increase to $1,564. In other words, an adult can earn up to $1,564 per month and still qualify for no cost Medi-Cal.Feb 16, 2022
How much is Medi-Cal per month?
Californians who qualify may be able to receive Medi-Cal by paying a small monthly premium based on their income. Premiums range from $20 to $250 per month for an individual or from $30 to $375 for a couple. To qualify, you must: Meet the medical requirements of Social Security's definition of disability.
What is meaningful use stage 2?
In particular, meaningful use Stage 2 is pushing for healthcare providers to provide more immediate access, particularly the ability to view, download, and transmit information through what is normally expected to be some sort of patient portal.
Can a parent access a minor's medical records?
Healthcare providers can choose to give parents access to the minor's records via a patient portal, but the providers should consider segregating certain information to make those confidential services inaccessible by the parent, Greene says.
NC Medicaid Managed Care Launches
Starting July 1, nearly 1.6 million Medicaid beneficiaries in North Carolina began receiving the same Medicaid services in a new way through NC Medicaid Managed Care health plans. Most beneficiaries will continue to get care from the same doctors they saw previously, but they will now be a member of a health plan.
NC Medicaid Managed Care: Info for Beneficiaries
NC Medicaid Managed Care means most Medicaid beneficiaries will receive the same Medicaid benefits in a new way – through a health plan’s provider network.
What is the CMS dental program?
The Centers for Medicare & Medicaid Services (CMS) is committed to improving access to dental and oral health services for children enrolled in Medicaid and CHIP. We have been making considerable progress (PDF, 303.79 KB) in our efforts to ensure that low-income children have access to oral health care. From 2007 to 2011, almost half of all states (24) achieved at least a ten percentage point increase in the proportion of children enrolled in Medicaid and CHIP that received a preventive dental service during the reporting year. Yet, tooth decay remains one of the most common chronic childhood diseases.
What is benchmark dental?
The benchmark dental package must be substantially equal to the (1) the most popular federal employee dental plan for dependents, (2) the most popular plan selected for dependents in the state's employee dental plan, or (3) dental coverage offered through the most popular commercial insurer in the state. States are also required to post ...
Does Medicaid cover dental care?
Medicaid covers dental services for all child enrollees as part of a comprehensive set of benefits, referred to as the Early and Periodic Screening, Diagnostic and Treatment (EPSDT) benefit. Though oral screening may be part of a physical exam, it does not substitute for a dental examination performed by a dentist.
Is dental insurance required for children?
Dental health is an important part of people's overall health. States are required to provide dental benefits to children covered by Medicaid and the Children's Health Insurance Program (CHIP), but states choose whether to provide dental benefits for adults.
How to apply for medicaid in New Jersey?
To be eligible for New Jersey Medicaid, a person must: 1 be a resident of New Jersey 2 be a U.S. Citizen or qualified alien (most immigrants who arrive after August 22, 1996 are barred from Medicaid for five years, but could be eligible for NJ FamilyCare and certain programs for pregnant women) 3 meet specific standards for financial income and resources
What is NJ Medicaid?
NJ Medicaid. Medicaid provides health insurance to parents/caretakers and dependent children, pregnant women, and people who are aged, blind or disabled. These programs pay for hospital services, doctor visits, prescriptions, nursing home care and other healthcare needs, depending on what program a person is eligible for.
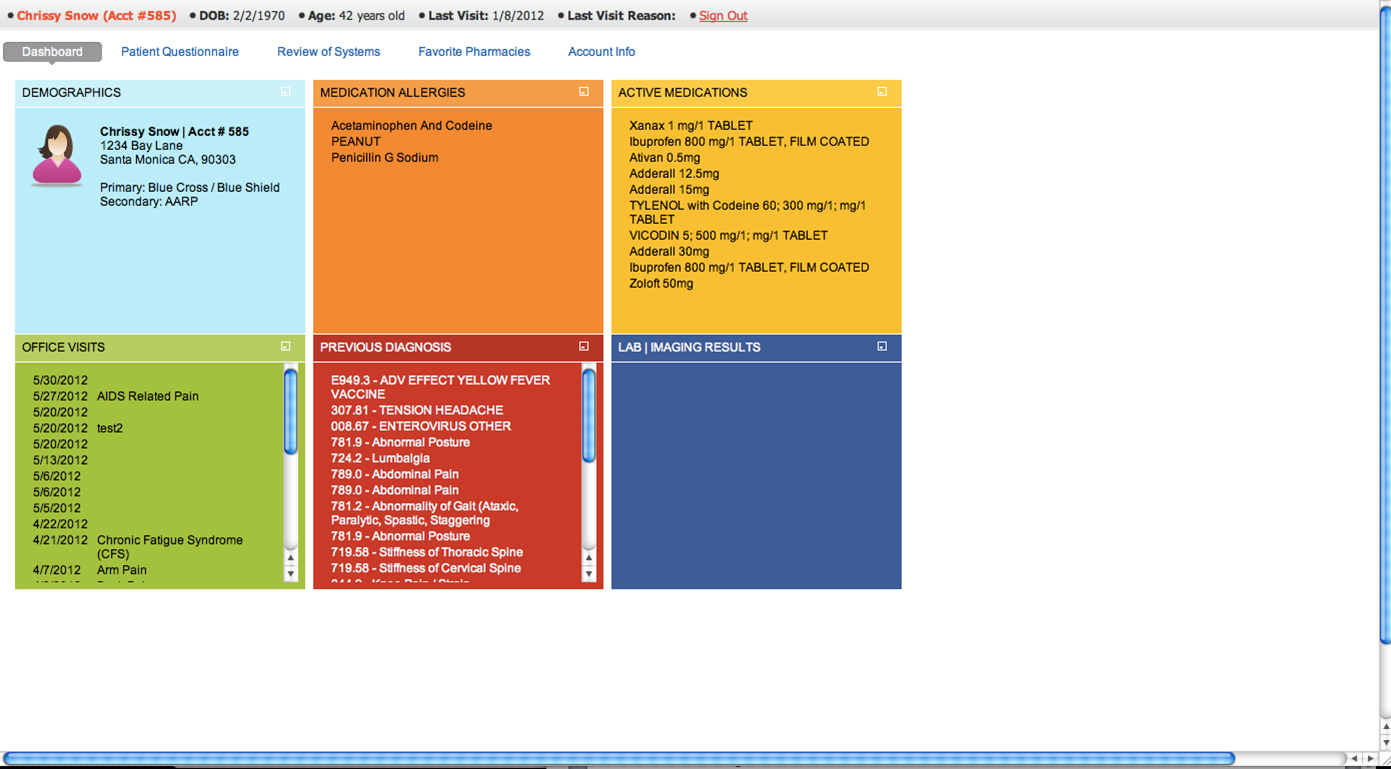
The Role of Patient Portals
Privacy Challenges with Patient Portals
- MCGEE: What do you think are the biggest privacyand security challenges related to patient portals? GREENE: I think one of them is authentication. How do you know that the patient is who the patient really says he or she is? There are a number of different strategies for trying to tackle that. Another privacy and security challenge here is that you have an Internet-facing website, ess…
Authentication For Portal Use
- MCGEE:What are the various ways that individuals can be credentialed and authenticated for accessing patient portals? GREENE:There are two stages here; the initial identity-proofing and the subsequent authentication every time someone logs into the patient portal. The identity-proofing normally happens either in-person or online. The in-person part...
Why only Passwords?
- MCGEE:Why do you think most organizations that have a patient portals will go with the username and password only? GREENE:Difficulty and lack of demand. I think there is going to be a minority of patients who may want the more robust features of multi-factor authentication, and may want to feel confident that their information is not going to be accessible to others based on just the …
Minors' EHRs
- MCGEE:What are the privacy and security challenges involved with providing access to health records of minors via the patient portals? GREENE:This is a very tough situation. You're going to have, under the law, some minors who have their parent or guardian as their personal representative under HIPAA who has the right to access their information. But, minors may be a…
Adult Caregivers
- MCGEE:What are the privacy and security challenges involved with giving access to elderly patients' information to say, an adult children? GREENE: I think it's a great idea. I think you definitely want to give the tools so that the patient does not have to share their username and password, but instead could have a greater level of control by creating a delegate account wher…
Other Methods of Access
- MCGEE:How do patient portals compare with other methods of providing patients with access to their health information, such as secure e-mail? GREENE:I think it is much easier to use. It will also link in sometimes with these other practices. So for example, the patient portal may also be a messaging portal where a secure e-mail is received by an individual. They receive an unsecure e …
Biggest Emerging Threats
- MCGEE:What do you think the biggest emerging privacy and security threats for portals? GREENE:I think as you get more of these, there will be more stories of vulnerabilities that have been identified. If the individual changes the URL by one number, and they are able to see someone else's information, I think we'll see security challenges on that front. I think we're going to see a c…
Popular Posts:
- 1. patient portal lake cumberland medical associates
- 2. marion women's health center patient portal
- 3. oda tool for patient portal questionnaire
- 4. patient portal hudson heights
- 5. how to enroll in nextmd patient portal
- 6. oschnew patient portal
- 7. patient portal dr gupta
- 8. patient portal arc
- 9. womens care florida patient portal
- 10. enroll patient portal ammc