10+ SAMPLE Nursing Incident Report in PDF
8 hours ago How to Write a Nursing Incident Report 1. Use Clinical Reasoning and Judgment. This is to confirm that an accident or incident has occurred that requires an... 2. Meet and Document the Statements. Documenting the statements of the principal parties involved as well as the... 3. Input the Necessary ... >> Go To The Portal
An incident report is a document that describes an accident or incident that deviates from safe nursing standards. Nurses want to exercise utmost care with their work, but accidents do happen and when they do, an incident report needs to be filed.
Full Answer
What is a nurse incident report?
An incident report is a document that describes an accident or incident that deviates from safe nursing standards. Nurses want to exercise utmost care with their work, but accidents do happen and when they do, an incident report needs to be filed.
What is incident reporting in nursing?
The short-term rehabilitation rating is based on care provided to residents who spent 100 days or fewer at a skilled nursing facility for care needed as a result of a stroke or accident, joint replacement or other rehabilitation-focused recovery.
How to submit an incident report?
You must file an Oregon Traffic Accident and Insurance Report with DMV within 72 hours when:
- Damage to any vehicle is over $2,500 (even if your vehicle was the only one in the crash);
- Any vehicle is towed from the scene;
- Injury or death resulted from this accident; or
- Damages to anyone’s property other than a vehicle involved in this accident is more than $2,500.
Should I file an incident report?
Generally, though, you should outline:
- What happened (detailed description of the incident, incident category/type)
- When it happened (date and time)
- Where it happened (be as specific as possible)
- How it happened (Are there any obvious root causes, like a puddle on the floor where an employee slipped)
- Who it happened to (employee name and title)
- Who reported it (Who is writing this document?)
How do you write an incident report in nursing?
What Information Do You Put in an Incident Report?Detailed description of the event with events listed chronologically.Witnesses or injured party statements.Injuries sustained by the person(s) as a result of the incident or the outcome.Actions taken immediately after the incident occurred.Treatments administered.More items...•
What goes in an incident report nursing?
Filling Out an Effective Incident Report Include the full names of those involved and any witnesses, as well as any information you have about how, or if, they were affected. Add other relevant details, such as your immediate response—calling for help, for example, and notifying the patient's physician.
What should be included in a patient incident report?
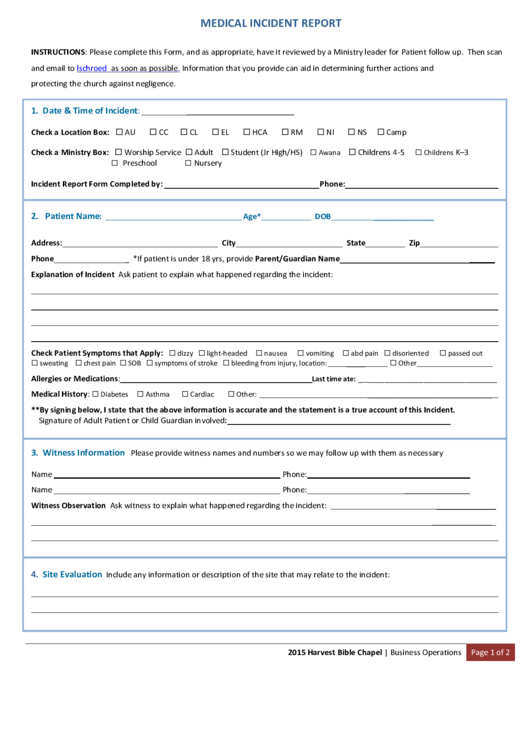
What to Include In a Patient Incident ReportDate, time and location of the incident.Name and address of the facility where the incident occurred.Names of the patient and any other affected individuals.Names and roles of witnesses.Incident type and details, written in a chronological format.More items...•
What are the 4 types of incident reports?
Common Types of Incident ReportsWorkplace. Workplace incident reports detail physical events that happen at work and affect an employee's productivity. ... Accident or First Aid. ... Safety and Security. ... Exposure Incident Report.
What makes a good incident report?
Effective Incident Reports identify the facts and observations. They avoid inclusion of personal biases; they do not draw conclusions/predictions, or place blame. Effective Incident Reports use specific, descriptive language and identified the action(s) taken by staff as a result of the unusual incident.
Why do nurses report incidents?
Nurses must comply with any formal internal reporting procedure, typically a written incident report. The next step is internal investigation or tracking, depending on the nature and seriousness of the event. It is helpful for an organization to know what worked well during the incident as well as what did not.
What are examples of incidents?
The definition of an incident is something that happens, possibly as a result of something else. An example of incident is seeing a butterfly while taking a walk. An example of incident is someone going to jail after being arrested for shoplifting.
How do you prepare an incident report?
Incident Report Sample Walkthrough: A Step-by-Step GuideStep 1: Provide Fundamental Information. ... Step 2: Take Note of Any Damages and Injuries. ... Step 3: Identify Affected Individual(s) ... Step 4: Identify Witnesses and Take Their Statements. ... Step 5: Take Action. ... Step 6: Close Your Report.
What are some examples of healthcare incidents?
A healthcare incident refers to an unintended or unexpected event that harms a patient or caregiver—or has the potential to harm them....2. Incidents related to the dispense of medication include:Wrong dose of prescription indicated.Wrong medication supplied.Incomplete or incorrect medication handoffs.
What are the 3 types of incidents?
3 Types of Incidents You Must Be Prepared to Deal WithMajor Incidents. Large-scale incidents may not come up too often, but when they do hit, organizations need to be prepared to deal with them quickly and efficiently. ... Repetitive Incidents. ... Complex Incidents.
What is a Type 5 incident?
TYPE 5 INCIDENT: One or two single response resources with up to 6 response personnel, the incident is expected to last only a few hours, no ICS Command and General Staff positions activated.
What types of incidents should be reported?
When do I need to report an incident?accidents resulting in the death of any person.accidents resulting in specified injuries to workers.non-fatal accidents requiring hospital treatment to non-workers.dangerous occurrences.
What is an incident report in healthcare?
Incident reporting in healthcare refers to collecting healthcare incident data with the goal to improve patient safety and care quality. Done well, it identifies safety hazards and guides the development of interventions to mitigate risks, thereby reducing harm.
How do I fill out an incident report?
Incident Report Sample Walkthrough: A Step-by-Step GuideStep 1: Provide Fundamental Information. ... Step 2: Take Note of Any Damages and Injuries. ... Step 3: Identify Affected Individual(s) ... Step 4: Identify Witnesses and Take Their Statements. ... Step 5: Take Action. ... Step 6: Close Your Report.
When should a nurse write an incident report?
Personal Liability No one wants to think that they will be named in a lawsuit, but it happens every day. So, merely for personal liability, nurses ought to complete incident reports with every event that includes property damage (or loss) or injury to anyone.
What to Expect After Writing an Incident Report?
Information in the nursing incident report will be analyzed and comprehended to identify the root cause of the incident. This is subject to changes...
What Do I Need to Tell the Patient and the Patient’s Family?
Educate the patient or the significant other on what to expect regarding the incident report. Impart an explanation when results of some procedures...
Do you dread writing a nurse incident report?
Now, that depends on the person writing it. Stressing over getting the report done or about what to include are common concerns for nurses. Always...
What is a nursing incident report?
A nursing incident report is a kind of report that a nurse or any health care worker writes to report an incident. This report gives a good bird's...
Why is it so important to write about the incident in detail?
The reason it is necessary to write the incident in detail is to make sure that you have written out what really happened. Not fabricating anything...
What is something that should be avoided when writing a nursing incident report?
Forgetting to place the evidence or the proof of what happened. As well as not rearranging in chronological order as to how it happened. Details ar...
How to write an incident report?
In determining what to include in an incident report and which details can be omitted, concentrate on the facts.#N#Describe what you saw when you arrived on the scene or what you heard that led you to believe an incident had taken place. Put secondhand information in quotation marks, whether it comes from a colleague, visitor, or patient, and clearly identify the source.# N#Include the full names of those involved and any witnesses, as well as any information you have about how, or if, they were affected .#N#Add other relevant details, such as your immediate response—calling for help, for example, and notifying the patient’s physician. Include any statement a patient makes that may help to clarify his state of mind, as well as his own contributory negligence.#N#It’s equally important to know what does not belong in an incident report.#N#Opinions, finger-pointing, and conjecture are not helpful additions to an incident report.#N#Do not:
When is an incident report required?
When a situation is significant—resulting in an injury to a person or damage to property —it’s obvious that an incident report is required. But many times, seemingly minor incidents go undocumented, exposing facilities and staff to risk. Let’s discuss three hypothetical situations.
Why is incident reporting important?
An incident report invariably makes its way to risk managers and other administrators, who review it rapidly and act quickly to change any policy or procedure that appears to be a key contributing factor to the incident. The report may also alert administration that a hospital representative should talk to a patient or family to offer assistance, an explanation, or other appropriate support. That’s an important function because such communication can be the balm that soothes the initial anger—and prevents a lawsuit.
Why is it important to file incident reports?
Filing incident reports that are factually accurate is the only way to help mitigate potentially disastrous situations arising from malpractice and other lawsuits. It’s your responsibility to record unexpected events that affect patients, colleagues, or your facility, regardless of your opinion of their importance.
What is the duty of a nurse?
As a nurse, you have a duty to report any incident about which you have firsthand knowledge. Failure to do so could lead to termination. It could also expose you to liability, especially in cases of patient injury. Protect yourself and your patients by filing incident reports anytime unexpected events occur.
What happens when incident reports are filled out properly?
If the incident report has been filled out properly with just the facts, there should be no reason to be concerned about how it’s used. The danger comes only when incident reports contain secondhand information, conjecture, accusations, or proposed preventive measures that do not belong in these reports.
Why is it important to talk to a hospital representative?
That’s an important function because such communication can be the balm that soothes the initial anger —and prevents a lawsuit.
What is incident report?
An incident report is an electronic or paper document that provides a detailed, written account of the chain of events leading up to and following an unforeseen circumstance in a healthcare setting.
Why are incident reports important?
Incident reports are used to communicate important safety information to hospital administrators and keep them updated on aspects of patient care for the following purposes: Risk management. Incident report data is used to identify and eliminate potential risks necessary to prevent future mistakes.
How long does it take to complete an incident report?
To ensure the details are as accurate as possible, incident reports should be completed within 24 hours by whomever witnessed the incident. If the incident wasn’t observed (e.g., a patient slipped, fell, and got up on his own), then the first person who was notified should submit it.
What are the concerns of nurses?
Stressing over getting the report done or about what to include are common concerns for nurses — not to mention worrying about whether filing the report reflects badly on your performance. Mistakes happen all the time, and healthcare facilities are not immune.
What are some examples of reportable events in New York?
Examples: adverse reactions, equipment failure or misuse, medication errors.
What Is a Nursing Incident Report?
We know what an incident report is and what it looks like. But do we have any idea as to what a nursing incident report is and what it looks like? Is there even any difference between these two kinds of reports? A nursing incident report is a kind of report that is filled out by nurses or anyone in the health care or medical field.
How to Write a Nursing Incident Report?
Being able to know what can and cannot be written in a nursing incident report is important. Take note that this document is a formal written report, and must be treated as such all the time. So to not make any mistakes when writing your incident report, here are five simple tips to guide you when you are writing your nursing incident report.
What is a nursing incident report?
A nursing incident report is a kind of report that a nurse or any health care worker writes to report an incident. This report gives a good bird’s eye view of how the incident happened and what can be done to resolve it.
Why is it so important to write about the incident in detail?
The reason it is necessary to write the incident in detail is to make sure that you have written out what really happened. Not fabricating anything in the report and to make sure that anyone who was there is also aware of what happened. That they can assure the one reading your report that it really happened.
What is something that should be avoided when writing a nursing incident report?
Forgetting to place the evidence or the proof of what happened. As well as not rearranging in chronological order as to how it happened. Details are an important part of the incident report.
What should a nurse report about an incident?
The nurse must be careful not to put blame or draw any conclusions about the incident. Incident reports should be devoid of opinion and bias. The nurse should just describe the incident as it happened. All witnesses and all those involved in the incident must be identified.
What is an incident report?
An incident report is a document that describes an accident or incident that deviates from safe nursing standards. Nurses want to exercise utmost care with their work, but accidents do happen and when they do, an incident report needs to be filed. Some incidents requiring incident reports are medication errors, falls, needle stick injuries, ...
How long does it take to fill out an incident report?
The nurse involved in the situation must fill out an incident form as soon as possible, preferably within 24 hours of the event. The form must be complete, accurate and factual. All pertinent information must be included in the report. The patient’s full name, initials, and hospital identification number must be written.
What are some incidents that require an incident report?
Some incidents requiring incident reports are medication errors, falls, needle stick injuries, damage to equipment, property losses, or any incident which causes harm to the patient because the nurse did not exercise reasonable care.
What should a nurse do if an accident occurs?
In this case, the nurse should seek assistance from the facility or legal counsel. If an accident occurs, the nurse should assess the client for any injury. Completing the incident report is the next thing to do.
Who reviews incident reports?
Incident reports are reviewed by nurse supervisors or managers, or sometimes by a panel who will decide on whether to investigate further . The nurse may be required to explain how the incident happened, how it could have been avoided, and what recommendations can be considered.
Should a nurse make a copy of an incident report?
The nurse should not place or make a copy of the incident report, nor make any reference about the form in the patient’s medical record. Instead, the nurse should make a complete and separate entry regarding the incident in the patient’s chart.
What Is Patient Incident Report?
Incidents are potentially dangerous incidents that have the potential to put patients or staff members at risk. Medical events are anything that can happen in the healthcare industry and can be caused by anything from equipment failure to injuries to poor patient care. Medical events can occur for a variety of reasons.
What Is the Purpose of the Patient Incident Report?
Patient incident reports provide information to facility officials about what happened to the patient. The information provided in the reports provides light on the steps that must be performed in order to deliver excellent patient care while also maintaining the smooth operation of your facility.
What to Include in a Patient Incident Report?
A patient incident report should include the bare minimum of information regarding the occurrence, such as who was involved, what happened, where it happened, when it happened, and how it happened. You should also include ideas on how to deal with the problem in order to lessen the likelihood of further instances occurring.
What Are the Benefits of Patient Safety Reporting?
Setting the relevant key performance indicators in your organization gets easier as a result of healthcare data analysis and analysis. You can receive the following significant advantages from filing a complaint:
Types of Incident Report
Even if an occurrence appears to be insignificant or has not resulted in any harm, it is still crucial to record it. Whether a patient has an allergic response to a drug or a visitor slips over an electrical cord, these occurrences provide valuable insight into how your facility can create a better, more secure environment for its visitors.
How to Create an Efficient Patient Incident Report
One thorough incident report should address all of the fundamental questions — who, what, where, when, and how — and provide full answers. The majority of hospitals adhere to a predetermined reporting format that is tailored to their own organizational requirements. An incident report, on the other hand, must include the following information:
FAQs
It is possible to acquire information on patient safety occurrences through the use of incident-reporting systems (IRSs). Even if they come with a significant financial cost, however, little is known regarding their usefulness.
What is an incident in healthcare?
An incident is an unfavourable event that affects patient or staff safety. The typical healthcare incidents are related to physical injuries, medical errors, equipment failure, administration, patient care, or others. In short, anything that endangers a patient’s or staff’s safety is called an incident in the medical system.
What is clinical incident?
A clinical incident is an unpleasant and unplanned event that causes or can cause physical harm to a patient. These incidents are harmful in nature; they can severely harm a person or damage the property. For example—
Why is incident reporting important?
Improving patient safety is the ultimate goal of incident reporting. From enhancing safety standards to reducing medical errors, incident reporting helps create a sustainable environment for your patients. Eventually, when your hospital offers high-quality patient care, it will build a brand of goodwill.
Why is reporting important in healthcare?
Reporting can also make healthcare operations more economically effective. By gathering and analyzing incident data daily, hospitals’ can keep themselves out of legal troubles. A comprehensive medical error study compared 17 Southeastern Asian countries’ medical and examined how poor reporting increases the financial burden on healthcare facilities.
What is clinical risk management?
Clinical risk management, a subset of healthcare risk management, uses incident reports as essential data points. Risk management aims to ensure the hospital administrators know their institution performance and identify addressable issues that increase their exposure.
What are near miss incidents?
#2 Near Miss Incidents 1 A nurse notices the bedrail is not up when the patient is asleep and fixes it 2 A checklist call caught an incorrect medicine dispensation before administration. 3 A patient attempts to leave the facility before discharge, but the security guard stopped him and brought him back to the ward.
How much of healthcare is wasted?
Even the World Health Organisation (WHO) has estimated that 20-40% of global healthcare spending goes waste due to poor quality of care. This poor healthcare quality leads to the death of more than 138 million patients every year. Patient safety in hospitals is in danger due to human errors and unsafe procedures.
Why is incident reporting important in nursing?
Nurses and other healthcare workers may feel that reporting the incident would not actually lead to change in their practice, or that there would be little follow up. It is important for organizations to allow employees to describe their involvement in an incident and discuss what could have been done to prevent the error and how they can resolve any longstanding effects and make resolution with coworkers.
Why is reporting events important in healthcare?
Safety is of the utmost importance in healthcare. Reporting events that may have negatively impact ed the safety of a patient or worker is not only beneficial for future safety, but also serves as a teaching tool.
What are healthcare incidents, and what causes them?
A healthcare incident refers to an unintended or unexpected event that harms a patient or caregiver—or has the potential to harm them. Incidents or errors occur for various reasons or root causes, such as system design flaws, lack of administrative oversight, poor training, digression from protocols, miscommunication, and more.
What are examples of incidents in healthcare?
Unfortunately, one doesn’t need to look far to find examples of incidents in healthcare. That’s because the industry is incredibly complex and fast-paced. It’s easy to make honest mistakes. For example:
What are the most commonly-reported hospital incidents?
Medication-related incidents are the most commonly reported incidents in healthcare. This includes administering the wrong dose, giving medication to the wrong patient, or omitting the dose.
Incidents: Insight to patient safety risks
Learning why incidents occur can help organizations make improvements to prevent them from happening again. But first, the healthcare system must prioritize incident reporting by providers, staff, and patients. In fact, risk management and patient safety rely on healthcare’s collective:
Are there incident severity levels?
The World Health Organization (WHO) classifies healthcare incidents according to the levels of severity (i.e., mild, moderate, severe, or death) based on the severity of the symptoms or loss of function, the duration of the symptoms, and/or the interventions required as a result of the incident.
What is incident management?
Incident management refers to the process of analyzing incidents and identifying the causes. Incident management entails more than simply filling out an incident report to track events and prevent them from occurring again. Incident management is also increasingly about handling data for quality improvement that affects reimbursement.
The symplr approach
Preventable harm will continue to occur unless organizations take a proactive approach to mitigate risk. That’s where symplr can help. symplr’s patient safety and risk management software is a structured digital event management system that captures (near) incidents, provides analytics, manages workflows, and monitors improvements.
Popular Posts:
- 1. patient web portal - quadramed
- 2. remove emory healthcare patient portal
- 3. sierra madre medical group patient portal
- 4. charlotte radiology patient portal login
- 5. baptist east patient portal
- 6. shreveport internal medicine patient portal
- 7. cerner patient portal support
- 8. moncure medical center patient portal
- 9. tria patient portal
- 10. sample patient case report with vaginal discharge due tosti