What does it mean to form a general impression of a …
29 hours ago · General Impression. Impression of the patient's condition that is formed on first approach, based on patient's environment, chief complaint, … >> Go To The Portal
Samples of clinical impression statements: “The individual appears to be a reliable informant with sincere commitment to achieving goals by adherence to the developed treatment plan.” “The individual exhibits moderate difficulty in social and occupational functioning that is compounded by significant medical, financial and legal problems.”
What is a clinical impression in an assessment?
There comes a time in any assessment when the practitioner must formulate an opinion of the individual’s status. The quality of this opinion is directly related to the practitioner’s formal education and professional clinical experience. The clinical impression is both an ongoing process and declaration of the “state of the individual”.
What makes a good general impression of a patient?
The entire mythical gestalt of your general impression actually involves only three things: the patient’s behavior, their breathing, and the appearance of their skin. The first thing you notice when you meet a person is their behavior.
What is the difference between impression and findings in a radiologist?
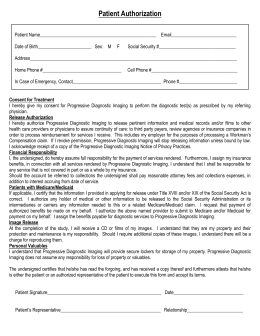
Findings – what was “found” out from the exam, listing each area of the body that was examined in the diagnostic imaging study. Oftentimes, the radiologist will use the word “unremarkable” if an area is normal. Impression – this is the radiologist’s “impression” or diagnosis of the diagnostic imaging exam.
What is general impression in EMS training?
In EMS training this is often described as the “general impression,” the “view from the door,” “big sick vs. little sick,” or other euphemisms. It’s your basic opinion of whether a patient is doing okay or not, and it’s formed within the first moments of contact.
What does impression mean on medical report?
An impression is a clinical summation of information and/or an opinion formed, which is the outcome of the clinical assessment process. The Clinical Impression may lead to a statement of a Condition about a patient.
What does impression mean in diagnosis?
Effective July 1, 2007, “diagnostic impression” is defined as equivalent to a provisional diagnosis, wherein there is “enough information to make a working diagnosis but the clinician wishes to indicate a significant degree of diagnostic uncertainty” (DSM-IV-TR, American Psychiatric Association, 2000).
What is an impression on test results?
Impression – this is the radiologist's “impression” or diagnosis of the diagnostic imaging exam. This section includes a summary of the results and any follow up testing (like a biopsy or additional diagnostic imaging) that the radiologist recommends.
What do you write in a clinical impression?
The clinical impression needs to take into account the individual's goals for the assessment and the resulting intervention. It should also identify the antecedent factors and environmental influences that affect the person's situation as well as the individual's positive strengths, attributes and competencies.
What does impression mean on CT scan results?
Impression. In this section, the radiologist summarizes the findings and reports the most important findings that they see and possible causes (this is called a differential diagnosis) for those findings. This section offers the most important information for decision-making.
What do you mean by impression?
Definition of impression 1 : the effect produced by impressing: such as. a : an especially marked and often favorable influence or effect on feeling, sense, or mind. b : a stamp, form, or figure resulting from physical contact.
What is the impression on an MRI report?
Section 6: The Radiologist's Diagnosis The “impression” section of a medical report is where patients will find the radiologist's diagnosis, along with recommendations for future testing for confirmation.
What is a primary working impression?
The primary impression is a concise statement describing the symptom, problem, or condition that is the reason for a medical encounter. A secondary impression is a second, less severe problem with the patient, which may or may not be directly related to the primary impression.
What is radiologist impression?
In a radiology report, the summary has been referred to as the "Impression," "Conclusion," or "Diagnosis" section. Sometimes this summary is an impression, sometimes it is a conclusion or diagnosis, and sometimes it is a concise statement of the findings.
What are impressions nursing?
Clinical impression was defined as nurses' impression that the child appeared 'ill' or 'not ill'.
What is initial impression in medicine?
The same is true for patients having their initial encounter with healthcare providers, be they physicians, nurses or other personnel. The first impression is established from the first moments of contact and will dictate the perceived quality of the overall experience.
How do you write clinically?
9:1710:21How to Write Clinical Patient Notes: The Basics - YouTubeYouTubeStart of suggested clipEnd of suggested clipMake sure you've got some sort of heading if you're in a multidisciplinary or a hospital basedMoreMake sure you've got some sort of heading if you're in a multidisciplinary or a hospital based environment. So that people know who is writing this note and what it's for make. Sure you have the date.
What are the three things that are included in the mythical gestalt of your general impression?
The entire mythical gestalt of your general impression actually involves only three things: the patient’s behavior, their breathing, and the appearance of their skin.
What is the gut sense of a patient?
Here’s my beef. Every medical provider, particularly those who work in the acute setting (such as prehospital medicine, critical care, or the emergency department), talks about a concept familiar to us all: the overall, gut sense of how ill a patient appears. In EMS training this is often described as the “general impression,” the “view from the door,” “big sick vs. little sick,” or other euphemisms. It’s your basic opinion of whether a patient is doing okay or not, and it’s formed within the first moments of contact.
What does it mean when a sick person can't complain?
And if sick people aren’t so sick they can’t complain at all, then their complaints reflect their acuity. They scream, they moan, they are visibly distressed by pain or fear. They say things like they’re dying or can’t breathe or can’t see or can’t move.
Why are people awake and alert?
A sick patient may be unconscious, or visibly lethargic; healthy people are awake and alert, because the brain is one of the last things the body allows to shut down. They’re also not obviously loopy, such as profoundly confused or combative, unless they have a chronic condition such as dementia.
What does it mean when a patient has a big problem after a full work up?
A gut belief that a patient has a big problem after a full work-up (including an H&P and diagnostics) is a different phenomenon, and suggests that your intuitive side is recognizing a larger pattern that your conscious self hasn’t yet been able to label. But that’s a distinct process from the instantaneous triage you perform when you first walk into a room.
What does it mean when you talk about a patient who looks sick?
When you talk about a patient who looks sick, or “doesn’t feel right,” or has some other nebulous problem like being “toxic,” you’re not tapping into some vast, indescribable vault of clinical judgment. All you’re doing is using shorthand that refers to the patient’s behavior, breathing, and skin. (Notice how these factors are emphasized in our initial assessment .)
Can you describe the quality of a patient that looks sick?
If you tell me the patient “looked sick” and I ask what you mean, you’ll probably wave your hands and reply that it’s ineffable; that you “had to be there”; that you know it when you see it, but that it can’t be quantified and can’t be analyzed.
Why is clinical impression important?
The clinical impression can assist the practitioner in deciding how to focus the psychosocial assessment process. Problem focused assessments are helpful for individuals who need “fixes” like linkage to specific services, medical interventions or pharmacological management.
Why is it important to write out the diagnosis in full?
Even if the client does not present with complicated conditions with several specifiers, it is important to write out the diagnosis in full in addition to the correct diagnostic code. Omitting this information can create difficulties if other medical personnel – who are not mental health specialists - are involved in the treatment of the patient. For this reason clarity is primary.
How to write out a diagnosis?
For every diagnosis you include, write out the diagnosis beside the numeric code. Write the correct name of the diagnosis in full, along with any specifiers related to the diagnosis.
How is a diagnosis determined in a mental health clinic?
Obviously, the diagnosis for any primary medical condition would be determined not by the mental health clinician, but by the physician assessing and treating the medical condition. The mental health clinician would only have that information because it would be forwarded to her/him through case coordination. However, in order to accurately record the diagnosis, your records must indicate the presence of the medical condition that most accurately explains the client’s full diagnostic picture. Treatment of an underlying medical condition will typically resolve the associated mental health problems, whereas the inverse is not true.
What is the practitioner's responsibility to communicate to the individual?
It is the practitioner’s responsibility to communicate to the individual that the relevance and effectiveness of the assessment and resulting intervention is directly related to the accuracy and completeness of the information provided. The individual or family being assessed must be empowered to participate, to identify priorities, ...
When to use provisional diagnosis?
The provisional diagnosis enters into the record an appropriate note of caution in choosing a diagnosis before all the facts are in.
When did ICD-10 become the standard for recording diagnoses?
ICD-10 became the standard for recording diagnoses on October 1, 2015. Knowledge and awareness of the changes to medical diagnoses must be recorded – when relevant – as part of the client’s record. To help prepare the clinician for this change, some of the more common medical diagnoses that mental health clinicians might encounter in their work are listed.
Abstract
In a society that values appearance, those who exhibit malformed parts of the face, neck and oral cavity may become less socially acceptable. Rehabilitation of the maxillofacial patient into society requires a broad knowledge of prosthodontics, plus the capacity for compassionate patient management.
Introduction
The cleft palate is an opening in the hard and/or soft palate. It may be genetic due to improper union of the maxillary process and the median nasal process during the second month of intrauterine development.
Primary Objectives
In the total rehabilitation of the maxillectomy patient, there are two primary objectives:
Impression Technique
The small defects should be blocked out with moist cotton or gauze (gauze or cotton should be lubricated with vaseline or petrolatum).
Discussion
Prosthodontic management of palatal defects has been employed for many years. Ambroise Pare probably was the first to use artificial means to close a palatal defect – as early as the 1500's. The early obturators were used to close congenital rather than acquired defects.
Summary
A thorough knowledge of what is normal is a must for the dentist to understand the acquired defects with which he interacts. It is important that the clinician become familiar with a technique and master it.
What is the difference between diagnosis and impression?
Impression is the initial opinion of a doctor by examining the patient. Diagnosis is the final opinion of a doctor about the disease. Impression is the initial opinion of a doctor by examining the patient. Diagnosis is the final opinion of a doctor about the disease.
What is the initial opinion of a doctor by examining the patient?
Impression is the initial opinion of a doctor by examining the patient.
What happens if a prescription doesn't arrive?
If a prescription doesn't arrive, the pharmacy will be calling the doctor to remind her about it. If a doctor is a "fake," the police/DEA investigation will be s
What is the diagnosis of a disease?
Diagnosis is the final opinion of a doctor about the disease. For example if a patient comes with fever,after examining the patient doctor will get an impression it MAY be malaria.But after further blood tests (of course,malaria test is positive),he will diagnose it finally as malaria.
Do we write down a diagnosis in the Netherlands?
In The Netherlands at present we don’t write down a diagnosis nor impression on our prescriptions, having to do with very sensitive privacy issues.
How long should an internal medicine presentation be?
The length of your presentation will depend on various factors, including the complexity of your patient, your audience, and your specialty. I have found that new internal medicine inpatients generally take 5-10 minutes to present. Internal medicine clerkship directors seem to agree. In a 2009 survey, they reported a range of 2-20 minutes for the ideal length of student inpatient presentations, with a median of 7 minutes.
How to protect patient privacy?
Be confident: Speak clearly at the loudest volume appropriate to protect patient privacy, vary your tone to emphasize the most important details, and maintain eye contact with members of your team.
Why is oral presentation important?
Effective oral case presentations help facilitate information transfer among physicians and are essential to delivering quality patient care. Oral case presentations are also a key component of how medical students and residents are assessed during their training. At its core, an oral case presentation functions as an argument.
How long should a surgical presentation be?
Every specialty presents patients differently. In general, surgical and OB/GYN presentations tend to be much quicker (2-3 minutes), while pediatric and family medicine presentations tend to be similar in length to internal medicine presentations. Tailor your presentations accordingly.
What is oral case presentation?
Oral case presentations are generally made to a medical care team, which can be composed of medical and pharmacy students, residents, pharmacists, medical attendings, and others. As the presenter, you should strive to deliver an interesting presentation that keeps your team members engaged.
Is an outpatient presentation the same as an inpatient presentation?
Outpatients may be presented similarly to inpatients. Your presentation’s focus, however, should align with your outpatient clinic’s specialty. For example, if you are working at a cardiology clinic, your presentation should be focused on your patient’s cardiac complaints.
Do you have to report lab results?
This section includes the results of any relevant laboratory testing, imaging, or other diagnostics that were obtained. You do not have to report the results of every test that was ordered. Before presenting, consider which results will further support your proposed diagnosis and exclude alternatives.
Why is it important to have access to your health records?
Online access to your health records may help you make more informed decisions about your healthcare. In addition, online access lets you share your radiology reports with other doctors electronically. This may increase the safety, quality, and efficiency of your care. top of page.
What is the most important part of a radiology report?
In this section, the radiologist summarizes the findings. The section lists your clinical history, symptoms, and reason for the exam. It will also give a diagnosis to explain what may be causing your problem. This section offers the most important information for decision-making. Therefore, it is the most important part of the radiology report for you and your doctor.
What is a comparison in radiology?
Comparison. Sometimes, the radiologist will compare the new imaging exam with any available previous exams. If so, the doctor will list them here. Comparisons usually involve exams of the same body area and exam type. Example: Comparison is made to a CT scan of the abdomen and pelvis performed August 24, 2013.
What does it mean when a radiologist looks at an area of the body?
Sometimes an exam covers an area of the body but does not discuss any findings. This usually means that the radiologist looked but did not find any problems to tell your doctor.
What is a biopsy?
biopsy. combining the finding with clinical symptoms or laboratory test results. comparing the finding with prior imaging studies not available when your radiologist looked at your images. For a potentially abnormal finding, the radiologist may make any of the above recommendations.
How many mm are axial images of pubic symphysis?
5 mm axial images from the lung bases through the pubic symphysis were acquired following the administration of intravenous and oral contrast. Coronal and Sagittal reformatted images were constructed from the source data.
Can a radiology doctor answer questions?
Sometimes, you may have questions about your report that your physician cannot answer. If so, talk to your facility's imaging staff. Many radiologists are happy to answer your questions.
What does "impression" mean in a radiologist?
Impression – this is the radiologist’s “impression” or diagnosis of the diagnostic imaging exam. This section includes a summary of the results and any follow up testing (like a biopsy or additional diagnostic imaging) that the radiologist recommends. ...
How long does it take to get a report from suburban imaging?
Reports are sent to your healthcare provider within 24 hours of your exam.
What is included in a radiology report?
A typical radiology reports includes these sections: Name or Type of Exam. Date of Exam. Interpreting Radiologist – the name of the radiologist who read the diagnostic imaging exam and wrote the report. Clinical History – describes the patient’s symptoms or existing diagnosis.
What is clinical history?
Clinical History – describes the patient’s symptoms or existing diagnosis.
Abstract
Introduction
- The cleft palate is an opening in the hard and/or soft palate. It may be genetic due to improper union of the maxillary process and the median nasal process during the second month of intrauterine development. It may also be acquired and the most common causes for maxillary defects are trauma, disease, pathological changes, genetics, surgical intervention, syndrome ass…
Primary Objectives
- In the total rehabilitation of the maxillectomy patient, there are two primary objectives: 1. To restore the functions of mastication, deglutition and speech. 2. To achieve normal oro – facialappearance.
Impression Technique
- The small defects should be blocked out with moist cotton or gauze (gauze or cotton should be lubricated with vaseline or petrolatum).
- Larger defects with gross undercuts should be packed with 4 x 4 inch gauze squares, it should be readily retrieved and they should be shoved into the defect.
- With time, the dentist will acquire clinical judgment with regard to which areas need blocking …
- The small defects should be blocked out with moist cotton or gauze (gauze or cotton should be lubricated with vaseline or petrolatum).
- Larger defects with gross undercuts should be packed with 4 x 4 inch gauze squares, it should be readily retrieved and they should be shoved into the defect.
- With time, the dentist will acquire clinical judgment with regard to which areas need blocking out prior to impressions.
Step by Step Procedure
- Preliminary impressions
- Primary cast
- Fabrication of special tray
- Final impression
Discussion
- Prosthodontic management of palatal defects has been employed for many years. Ambroise Pare probably was the first to use artificial means to close a palatal defect – as early as the 1500's. The early obturators were used to close congenital rather than acquired defects. The early objectives of treatment were artificial closure of the defect and adequate retention of the artifici…
Summary
- A thorough knowledge of what is normal is a must for the dentist to understand the acquired defects with which he interacts. It is important that the clinician become familiar with a technique and master it. It must always be remembered, and patient must be so counselled before treatment, that the clinician can only try to provide alternative means of what the patient has lost…
Popular Posts:
- 1. rvmc patient portal
- 2. psychbc patient portal
- 3. abq davita patient login
- 4. uphs patient portal
- 5. charles river medical patient portal
- 6. florida waterman hospital patient portal
- 7. southern vermont medical center patient portal
- 8. chr milestone patient portal
- 9. mindful therapy group patient portal
- 10. dasco patient portal