Patient Portals and the HIPAA Security Rule - Compliancy …
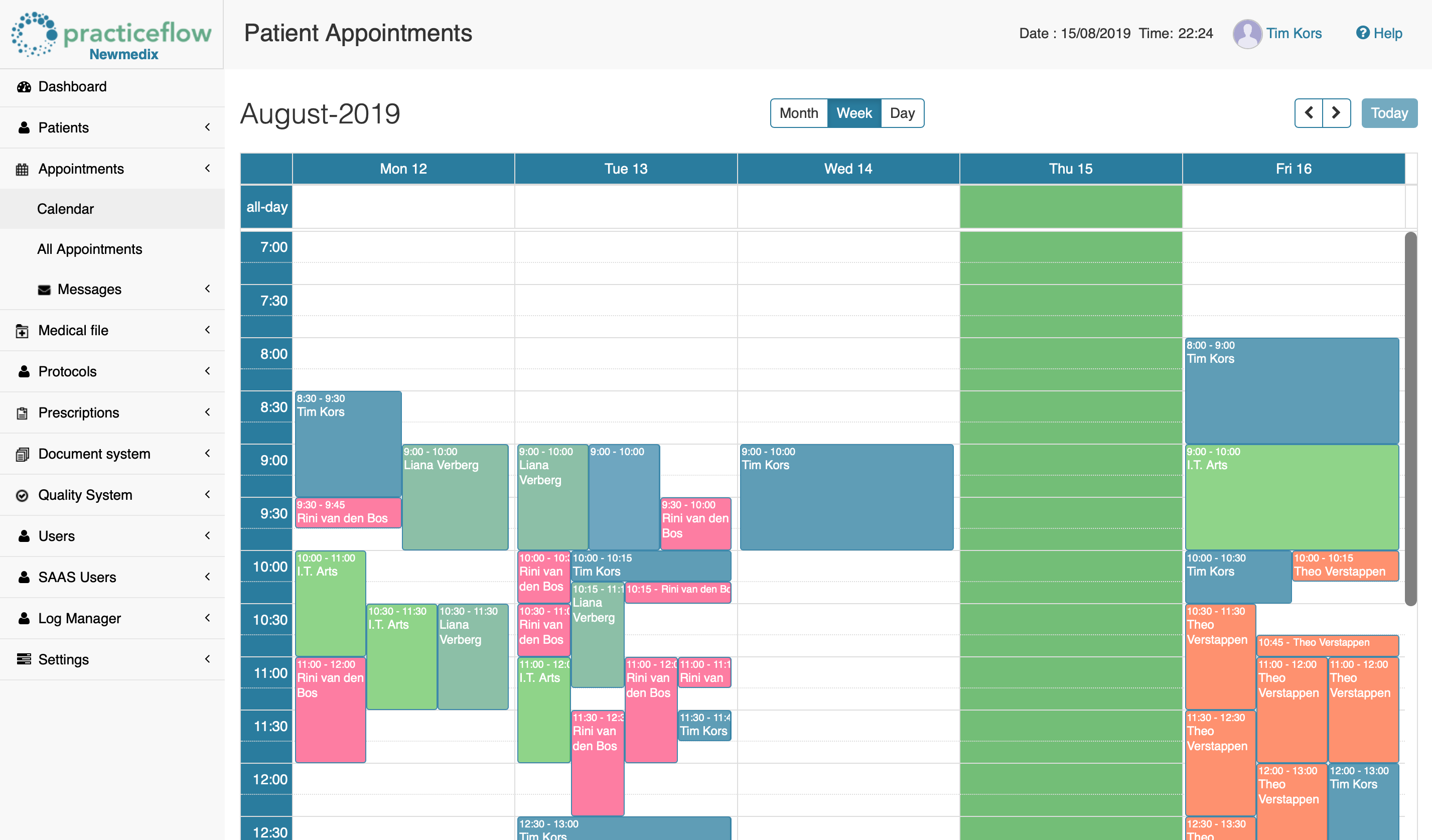
17 hours ago Sep 09, 2019 · Patient Portals and the HIPAA Security Rule. Healthcare providers frequently allow patients to access their electronic health records (EHRs) through a patient portal. Online patient portals allow patients to view their medical records, schedule appointments, and even request refills of prescriptions, anywhere the patient has access to the Internet. Patient portals contain … >> Go To The Portal
Health Insurance Portability and Accountability Act
The Health Insurance Portability and Accountability Act of 1996 was enacted by the 104th United States Congress and signed by President Bill Clinton in 1996. It was created primarily to modernize the flow of healthcare information, stipulate how Personally Identifiable Information maintained by the healthcare and healthcare insurance industries should be protected from fraud and theft, and address lim…
What are the patients rights under HIPAA?
Sep 09, 2019 · Patient Portals and the HIPAA Security Rule. Healthcare providers frequently allow patients to access their electronic health records (EHRs) through a patient portal. Online patient portals allow patients to view their medical records, schedule appointments, and even request refills of prescriptions, anywhere the patient has access to the Internet. Patient portals contain …
What are the rules of HIPAA?
Mar 23, 2020 · If you have a patient portal developed, provided by, or on behalf of a covered entity (health plan, healthcare clearinghouses, or healthcare providers), it must be HIPAA compliant. If you are a business associate that stores, collects, processes, or transmits PHI on behalf of covered entities, your patient portal must be HIPAA compliant.
What is a patient portal?
HIPAA eCommerce compliance requires patient portals to have strong security and privacy protections to prevent unauthorized access of these confidential PHI records. HIPAA Compliance is Key Failing to adhere to HIPAA standards can result in serious fines. Investing in a HIPAA compliant website can keep your medical business out of trouble.
Are patient portals required?
Not only does a patient portal raise privacy issues, but also it most certainly will have HIPAA security issues. You must include a patient portal in your risk assessment. I strongly suggest that you do so before permitting patient use. But if you haven’t previously done so, get on it!
What does HIPAA have to say about patient portals?
Patient portals contain information that constitutes electronic protected health information (ePHI) under the HIPAA Security Rule. ePHI is defined as any protected health information (PHI) that is created, stored, transmitted, or received in any electronic format or media.Sep 9, 2019
Are patient portals HIPAA compliant?
Patient healthcare portals help medical practices adhere to HIPAA regulations both by providing patients with easy access to their medical records and by using security measures to protect those records.
What are the 3 HIPAA implementation requirements?
Broadly speaking, the HIPAA Security Rule requires implementation of three types of safeguards: 1) administrative, 2) physical, and 3) technical.
What are the HIPAA requirements for EHR use?
Access control: A HIPAA-compliant EHR should use access control measures, such as passwords, so that only authorized persons can access protected health information. Encryption: The EHR should provide encryption for the data it contains.Jul 2, 2018
Are patient portals confidential?
Yes, many patient portals are secure as they have security and privacy safeguards to keep your information protected. To ensure your data remains protected from any unauthorized access, these healthcare portals are hosted on a secure connection and can be accessed via a password-protected login.Nov 11, 2021
What safeguards are in place for patient portals?
Patient portals have privacy and security safeguards in place to protect your health information. To make sure that your private health information is safe from unauthorized access, patient portals are hosted on a secure connection and accessed via an encrypted, password-protected logon.
What are the 4 rules of HIPAA?
The HIPAA Security Rule Standards and Implementation Specifications has four major sections, created to identify relevant security safeguards that help achieve compliance: 1) Physical; 2) Administrative; 3) Technical, and 4) Policies, Procedures, and Documentation Requirements.
What are the 5 main components of HIPAA?
What are the 5 main components of HIPAA?Title I: HIPAA Health Insurance Reform. ... Title II: HIPAA Administrative Simplification. ... Title III: HIPAA Tax-Related Health Provisions. ... Title IV: Application and Enforcement of Group Health Plan Requirements. ... Title V: Revenue Offsets.
What are the 5 HIPAA standards?
HHS initiated 5 rules to enforce Administrative Simplification: (1) Privacy Rule, (2) Transactions and Code Sets Rule, (3) Security Rule, (4) Unique Identifiers Rule, and (5) Enforcement Rule.Feb 3, 2022
What is the difference between EMR and EHR?
It's easy to remember the distinction between EMRs and EHRs, if you think about the term “medical” versus the term “health.” An EMR is a narrower view of a patient's medical history, while an EHR is a more comprehensive report of the patient's overall health.Feb 15, 2017
What are the privacy and security issues involved with EHR?
As with any online digital format, concerns of breach exist. Internet hackers possess a digital power that frightens individuals looking to conceal sensitive data. There have been cases in which medical information has been accessed by unauthorized users.
What is an EMR HIPAA?
EMR is a system that a particular healthcare provider uses to collect and track all patient data in his or her facility. Thus, patient data in EMRs is limited to a single provider. EHRs, on the other hand, accumulate data across different healthcare providers and specialists involved in taking care of the patient.Jul 30, 2019
What is HIPAA Privacy?
What Is HIPAA? The Health Insurance Portability and Accountability Act (HIPAA) protects patients’ privacy by limiting access to PHI (Protected Health Information) and governing acceptable use of their health data. The HIPAA Privacy Rule is composed of national regulations for the use and disclosure of PHI in healthcare treatment, payment, ...
What is protected health information?
Protected Health Information (PHI) is any information that is held by a covered entity regarding a patient’s health status, provision of health care, or health care payment.
How much is an EPHI violation fine?
A covered entity that did not know and could not have reasonably known of an ePHI breach could be fined $100-$50,000 per incident and up to $1.5 Million.
Who is Kirsty from Bridge Patient Portal?
Community Manager at Bridge Patient Portal. Kirsty is an experienced marketer with a demonstrated history of working in the medical and software industry. She is skilled in digital marketing, including SEO copywriting. Kirsty marries her passion for healthcare with her experience in digital marketing.
Is PHI included in HIPAA notifications?
HIPAA compliant messaging requires you to exclude PHI in an SMS, email, push, or IVR notification. If you do include PHI in a notification, have your patients accept terms and conditions which permit you to use limited PHI in your notifications, clearly defining what PHI is included. Always use a HIPAA-Compliant Hosting Service.
What is the HIPAA Privacy Rule?
With limited exceptions, the HIPAA Privacy Rule (the Privacy Rule) provides individuals with a legal, enforceable right to see and receive copies upon request of the information in their medical and other health records maintained by their health care providers and health plans.
Who has the right to access health records?
The Privacy Rule generally also gives the right to access the individual’s health records to a personal representative of the individual. Under the Rule, an individual’s personal representative is someone authorized under State or other applicable law to act on behalf of the individual in making health care related decisions. With respect to deceased individuals, the individual’s personal representative is an executor, administrator, or other person who has authority under State or other law to act on behalf of the deceased individual or the individual’s estate. Thus, whether a family member or other person is a personal representative of the individual, and therefore has a right to access the individual’s PHI under the Privacy Rule, generally depends on whether that person has authority under State law to act on behalf of the individual. See 45 CFR 164.502 (g) and 45 CFR 164.524.
What does it mean when a lab report is complete?
For purposes of the HIPAA Privacy Rule, clinical laboratory test reports become part of the laboratory’s designated record set when they are “complete,” which means that all results associated with an ordered test are finalized and ready for release.
Can a covered entity send a copy of a PHI?
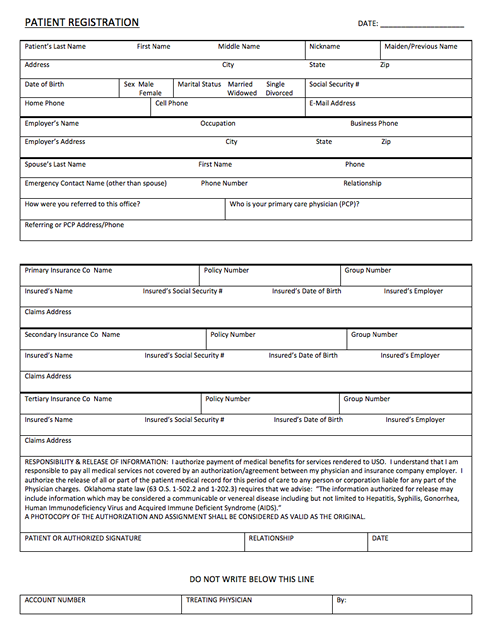
The individual’s request to direct the PHI to another person must be in writing, signed by the individual, and clearly identify the designated person and where to send the PHI. A covered entity may accept an electronic copy of a signed request (e.g., PDF), as well as an electronically executed request (e.g., via a secure web portal) that includes an electronic signature. The same requirements for providing the PHI to the individual, such as the fee limitations and requirements for providing the PHI in the form and format and manner requested by the individual, apply when an individual directs that the PHI be sent to another person. See 45 CFR 164.524 (c) (3).
What is access requested?
The access requested is reasonably likely to cause substantial harm to a person (other than a health care provider) referenced in the PHI. The provision of access to a personal representative of the individual that requests such access is reasonably likely to cause substantial harm to the individual or another person.
What are the two categories of information that are expressly excluded from the right of access?
In addition, two categories of information are expressly excluded from the right of access: Psychotherapy notes , which are the personal notes of a mental health care provider documenting or analyzing the contents of a counseling session, that are maintained separate from the rest of the patient’s medical record.
Why is it important to have access to health information?
Providing individuals with easy access to their health information empowers them to be more in control of decisions regarding their health and well-being. For example, individuals with access to their health information are better able to monitor chronic conditions, adhere to treatment plans, find and fix errors in their health records, ...
What are the challenges of implementing HIPAA compliant patient portals?
The challenges of implementing HIPAA compliant patient portals depend on a provider's IT infrastructure and its operating system's complexity and interoperability. There are also the legal and regulatory requirements that include meeting mandatory HIPAA guidelines and voluntary best practices. The challenges of HIPAA compliant portal development include:
What is the HIPAA Privacy Rule?
The HIPAA Privacy Rule gives patients the right to obtain copies of their medical records, treatments and protected health information or PHI. These requirements go further if medical providers want to receive reimbursement from Medicare and Medicaid -- patients must be able to access their records online, download copies and transmit the information to third-party providers. Most medical practices are finding it necessary to develop patient portals where patients and physicians can interact, share information and perform important functions such as practices billing patients and accepting payments online. HIPAA standards rule requires that these patient portals have strong security and privacy protections to prevent unauthorized access of these confidential PHI records.
What are patient portals?
Patient portals generate many associated mandatory and medical compliance issues. Practices must consider their business associates and chain-of-trust issues that arise when sending information by electronic transmission. Medical companies deal with insurance companies, Internet service providers, labs, pharmacies, billing and coding services, hospitals and other practices across different medical-related specialties.
What stakeholders are involved in developing a patient portal?
These include the practice's senior leadership, patient advocates in the community, risk management stakeholders like insurers and legal counsel, physicians and clinicians and marketing staffs and health information management professionals who need to sell the benefits of using the patient portal to patients, caregivers and even some staff members who might hesitate to interact with patients electronically. Patient portals enhance communications, and sounding out these stakeholders is essential for developing an effective portal because each will be using the technology at ever-increasing rates.
Fees That Can Be Charged to Individuals For Copies of Their Phi
Right to Have Phi Sent Directly to A Designated Third Party
- Can an individual, through the HIPAA right of access, have his or her health care provider or heal…
Yes. If requested by an individual, a covered entity must transmit an individual’s PHI directly to another person or entity designated by the individual. The individual’s request must be in writing, signed by the individual, and clearly identify the designated person or entity and where to send t… - Are there any limits or exceptions to the individual’s right to have the individual’s PHI sent directl…
The right of an individual to have PHI sent directly to a third party is an extension of the individual’s right of access; consequently, all of the provisions that apply when an individual obtains access to her PHI apply when she directs a covered entity to send the PHI to a third part…
Scope of Information Covered by Access Right
- What personal health information do individuals have a right under HIPAA to access from their h…
With limited exceptions, the HIPAA Privacy Rule gives individuals the right to access, upon request, the medical and health information (protected health information or PHI) about them in one or more designated record sets maintained by or for the individuals’ health care providers a… - Does an individual’s right under HIPAA to access their health information apply only to the infor…
No. An individual has a broad right under the HIPAA Privacy Rule to access the PHI about the individual in all designated record sets maintained by or for a covered entity, whether in electronic or paper form, not just the designated record set that comprises the “medical record.” See 45 CF…
timelines For Providing Access
- How timely must a covered entity be in responding to individuals’ requests for access to their PHI?
Under the HIPAA Privacy Rule, a covered entity must act on an individual’s request for access no later than 30 calendar days after receipt of the request. If the covered entity is not able to act within this timeframe, the entity may have up to an additional 30 calendar days, as long as it pro… - Under the EHR Incentive Program, participating providers are required to provide individuals wit…
Health care providers participating in the EHR Incentive Program may use the patient engagement tools of their Certified EHR Technology to make certain information available to patients quickly and satisfy their EHR Incentive Program objectives. Doing so also has the added benefit of satis…
Other Questions on Access Right
- Is a health care provider permitted to deny an individual’s request for access because the individ…
No. A covered entity may charge an individual that has requested a copy of her PHI a reasonable, cost-based fee for the copy. See 45 CFR 164.524(c)(4). However, a covered entity may not withhold or deny an individual access to her PHI on the grounds that the individual has not paid t… - If an individual’s physician orders a test from a clinical laboratory that may take multiple steps o…
For purposes of the HIPAA Privacy Rule, clinical laboratory test reports become part of the laboratory’s designated record set when they are “complete,” which means that all results associated with an ordered test are finalized and ready for release.
Other Access Topics
- Under HIPAA, when can a family member of an individual access the individual’s PHI from a heal…
The HIPAA Privacy Rule provides individuals with the right to access their medical and other health records from their health care providers and health plans, upon request. The Privacy Rule generally also gives the right to access the individual’s health records to a personal representati… - May a covered entity accept standing requests from individuals to access their PHI or to have th…
Yes, and covered entities should have processes in place that enable individuals to receive access to their PHI, including to direct a copy of their PHI to a third party of their choice, on a standing, regular basis, without requiring individuals to repeat their requests for access every time a copy …
Popular Posts:
- 1. norwood urgent care patient portal
- 2. patient portal site:nih.gov
- 3. christus patient portal sign in
- 4. albany ob gyn patient portal
- 5. central mo cardiology patient portal
- 6. patient portal for rj langerman patient
- 7. abington women's primary patient portal
- 8. uofm patient portal
- 9. chambersburg patient portal
- 10. mt baker patient portal