Head-to-Toe Assessment: Complete 12-Step Checklist
14 hours ago View Guidelines for Report of Patient Assessment (1).docx from NURSING MISC at Nassau Community College. Guidelines for Report of Patient Assessment: Head to Toe Patient (initials) _ is a _ year old Study Resources >> Go To The Portal
4 General Principles for Head-to-Toe Nursing Assessments
- 1: Documentation Is Important. Remember that head-to-toe assessment documentation is a critical part of the process. If...
- 2: Communicate Throughout. Be sure to communicate clearly with your patient throughout the assessment. Always ask...
- 3: Keep an Eye on Bilateral Symmetry. The human body is, in general,...
- Collect their vital signs. (It's encouraged to ask permission before touching a patient. ...
- Check heart rate.
- Measure blood pressure.
- Take body temperature.
- Pulse oxymetry.
- Respiratory rate.
- Check pain levels.
- Check hight and weight and calculate their BMI.
What is a head to toe assessment in nursing?
Chapter 2. Patient Assessment A comprehensive head-to-toe assessment is done on patient admission, at the beginning of each shift, and when it is determined to be necessary by the patient’s hemodynamic status and the context.
How do you conduct a head-to-toe assessment?
In-Depth Guide to Conducting a Head-to-Toe Assessment. 1 Step 1: Check Vital Signs and Neurological Indicators. The first things you'll want to check are patient vital signs and overall neurological status. 2 Step 2: Examine Head and Face. 3 Step 3: Inspect Eyes. 4 Step 4: Evaluate Ears. 5 Step 5: Check Nose. More items
What is a head to toe physical exam/survey?
• Systematic head to toe physical exam that is complaint focused & conducted simultaneously with reassessment of the ABCDEs. • This exam / survey is done after stabilization of life threatening airway, breathing and circulation problems www.depts.washington.edu
What is a comprehensive head-to-toe assessment?
A comprehensive head-to-toe assessment is done on patient admission, at the beginning of each shift, and when it is determined to be necessary by the patient’s hemodynamic status and the context. The head-to-toe assessment includes all the body systems, and the findings will inform the health care professional on the patient’s overall condition.
See more
How do you record head to toe assessment?
Head-to-Toe Assessment Sequence “During an assessment, the first thing that should be noted is the patient's overall appearance or general status,” Zucchero says. “This includes level of alertness, state of health/comfort/distress, and respiratory rate. This is done even prior to taking vital signs.”
How do I document normal head assessment?
Documenting a normal exam of the head, eyes, ears, nose and throat should look something along the lines of the following:Head – The head is normocephalic and atraumatic without tenderness, visible or palpable masses, depressions, or scarring. ... Eyes – Visual acuity is intact.More items...•
How do you write a nursing assessment summary?
The following are comprehensive steps to write a nursing assessment report.Collect Information. ... Focused assessment. ... Analyze the patient's information. ... Comment on your sources of information. ... Decide on the patient issues.
Why is there a need to assess patient thoroughly from head to toe while doing physical assessment?
Electronic head to toe assessment forms makes sure that nurses and other professional examiners don't miss a single test item during the patient's physical exam. They also provide a full and timely insight into the health condition of a patient and can point to some early symptoms that may require early attention.
How do you document an assessment?
An assessment report should accomplish the following:Outline the student learning or program outcomes or goals assessed during the assessment cycle timeframe.Identify and describe the specific assessment method(s) and tools used to gather evidence for the outcomes or goals.Identify the specific source(s) of the data.More items...
How do you document patient general appearance?
AppearanceAge: Does the patient appear to be his stated age, or does he look older or younger?Physical condition: Does he look healthy? ... Dress: Is he dressed appropriately for the season? ... Personal hygiene: Is he clean and well groomed, or unshaven and unkempt, with dirty skin, hair or nails?More items...•
How do you write a patient report?
Summary: The format of a patient case report encompasses the following five sections: an abstract, an introduction and objective that contain a literature review, a description of the case report, a discussion that includes a detailed explanation of the literature review, a summary of the case, and a conclusion.
How do you write a nursing patient report?
How to write a nursing progress noteGather subjective evidence. After you record the date, time and both you and your patient's name, begin your nursing progress note by requesting information from the patient. ... Record objective information. ... Record your assessment. ... Detail a care plan. ... Include your interventions.
How do you write a patient assessment?
Assessment & PlanWrite an effective problem statement.Write out a detailed list of problems. From history, physical exam, vitals, labs, radiology, any studies or procedures done, microbiology write out a list of problems or impressions.Combine problems.
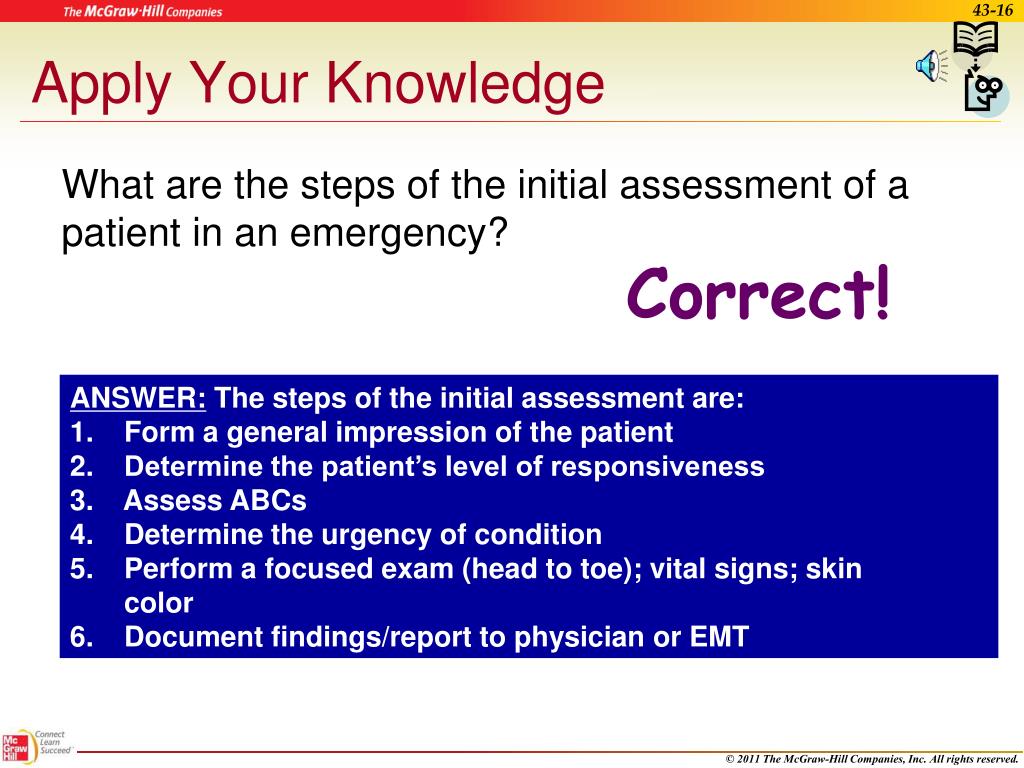
What are the five steps of patient assessment?
emergency call; determining scene safety, taking BSI precautions, noting the mechanism of injury or patient's nature of illness, determining the number of patients, and deciding what, if any additional resources are needed including Advanced Life Support.
What is the usual sequence of doing examination from head to toe?
In-Depth Guide to Conducting a Head-to-Toe Assessment4 General Principles for Head-to-Toe Nursing Assessments. ... Step 1: Check Vital Signs and Neurological Indicators. ... Step 2: Examine Head and Face. ... Step 3: Inspect Eyes. ... Step 4: Evaluate Ears. ... Step 5: Check Nose. ... Step 6: Probe Mouth and Throat.More items...•
How long should a head to toe assessment take?
The assessment takes about 5-10 minutes.
What is the importance of establishing a personal relationship with the patient and the nurse?
When beginning an assessment, Zucchero says, “establishing a personal relationship of trust and respect between the patient and the nurse is vital.” She adds that is it important throughout an assessment to assess how the patient is doing, and make sure they are properly draped and comfortable.
What is problem focused assessment?
A problem-focused assessment is an assessment based on certain care goals. For example, a nurse working in the ICU and a nurse that does maternal-child home visits have different patient populations and nursing care goals, she says. These assessments are generally focused on a specific body system such as respiratory or cardiac. While the entire body is important there is usually not enough time for a detailed full-body assessment.
What does Ferere say about nursing?
Ferere adds that new nurses should trust the foundational knowledge obtained in nursing school and seek strong, supporting nursing mentors as resources in health care delivery settings.
What does it mean to be a nurse?
Being a nurse means being a lot of things to a lot of people. But one of the basics of nursing is performing a head-to-toe assessment. We've put together a step-by-step guide to what happens in a nursing assessment and how nurses should understand the physical, emotional and mental aspects of someone’s body systems.
Why is it important to engage a patient early in the visit?
Engaging the patient early in the visit increases the likelihood that the patient will take more ownership of health status and ongoing health needs.
What is a complete health assessment?
A complete health assessment is a detailed examination that typically includes a thorough health history and comprehensive head-to-toe physical exam. This type of assessment may be performed by registered nurses for patients admitted to the hospital or in community-based ...
What is head to toe assessment?
A head-to-toe assessment refers to a physical examination or health assessment, and it becomes one of the many important components of understanding a patient’s needs and problems.
Why does my bowel make a noise after surgery?
Hypoactive or absent bowel sounds may be present after abdominal surgery, or with peritonitis or paralytic ileus. Pain and tenderness may indicate underlying inflammatory conditions such as peritonitis. Unusual findings in urine output may indicate compromised urinary function.
How to check capillary refill?
To check capillary refill, depress the nail edge to cause blanching and then release. Colour should return to the nail instantly or in less than 3 seconds. If it takes longer, this suggests decreased peripheral perfusion and may indicate cardiovascular or respiratory dysfunction. Unusual findings should be followed up with a focused cardiovascular assessment.
How many patient identifiers are needed to confirm patient ID?
Confirm patient ID using two patient identifiers (e.g., name and date of birth).
What does a limitation in range of movement mean?
Limitation in range of movement may indicate articular disease or injury. Palpate pulses for symmetry in rate and rhythm. Asymmetry may indicate cardiovascular conditions or post-surgical complications. Unequal handgrip and/or foot strength may indicate underlying conditions, injury, or post-surgical complications.
What are the steps to assess skin, hair, and nails?
Evaluating the skin, hair, and nails is an ongoing element of a full body assessment as you work through steps 3-9. 2. Skin, hair, and nails: Inspect for lesions, bruising, and rashes. Palpate skin for temperature, moisture, and texture. Inspect for pressure areas. Inspect skin for edema.
What is the egg in hair?
Check hair for the presence of lice and/or nits (eggs), which are oval in shape and adhere to the hair shaft.
How to check for lice and nits?
Inspect scalp for lesions and hair and scalp for presence of lice and/or nits. Inspect nails for consistency, colour, and capillary refill. Check for and follow up on the presence of lesions, bruising, and rashes.Variations in skin temperature, texture, and perspiration or dehydration may indicate underlying conditions.
How to test hearing?
Test the hearing by occluding one ear and whispering two words and have the patient repeat them back. Repeat this for the other ear.
Where is the ortic located?
A ortic: found right of the sternal border in the 2nd intercostal space REPRESENTS S2 “dub” which is the loudest.
How many sounds per minute should you hear when you auscultate?
Auscultate with the diaphragm for bowel sounds: start in the RIGHT LOWER QUADRANT and go clockwise in all the 4 quadrants. should hear 5 to 30 sounds per minute…if no, bowel sounds are noted listen for 5 full minutes. Documents as: normal, hyperactive, or hypoactive.
How to strengthen a patient's arm?
Have the patient extend their arms and move the arms against resistance and flex against resistance (grade strengthen 0-5) along with having the patient squeeze your fingers (note the grip).
How long does it take for a fingernail to refill?
Hand and fingernails for color: they should be pink and capillary refill should be less than 2 seconds
What color should your lips be?
Inspect lips (lip should be pink NOT dusky or blue/cyanotic or cracked, and free from lesions)
What is the order of auscultation?
Auscultation. However, with the abdomen it is changed where auscultation is performed second instead of last. The order for the abdomen would be: Inspection. Auscultation. Percussion. Palpation (palpation and percussion are done last to prevent from altering bowel sounds) Provide privacy, perform hand hygiene, introduce yourself to the patient, ...
How are the bulbar and palpebral conjunctiva examined?
The bulbar and palpebral conjunctivae are examined by separating the eyelids widely and having the client look up, down and to each side. When separating the lids, the examiner should exert NO PRESSURE against the eyeball; rather, the examiner should hold the lids against the ridges of the bony orbit surrounding the eye.
How to stop lid eversion?
Ask the client to look down but keep his eyes slightly open. This relaxes the levator muscles, whereas closing the eyes contracts the orbicularis muscle, preventing lid eversion. Gently grasp the upper eyelashes and pull gently downward. Do not pull the lashes outward or upward; this, too, causes muscles contraction.
What color is the iris?
Color of the iris depends on the person’s race (black, blue, brown or green).
What part of the eye covers the iris?
Upper eyelids cover the small portion of the iris, cornea, and sclera when eyes are open.
How to tell if a client has a taste?
1. Sensory function (This nerve innervate the anterior 2/3 of the tongue). Place a sweet, sour, salty, or bitter substance near the tip of the tongue. Normally, the client can identify the taste. 2. Motor function. Ask the client to smile, frown, raise eyebrow, close eyelids, whistle, or puff the cheeks.
What is the purpose of inspecting the eyelids?
Inspect the eyelids for position and symmetry.
Why is it important to have a good physical assessment?
Establishing a good assessment would later-on provide a more accurate diagnosis, planning, and better interventions and evaluation, that’s why it’s important to have a good and strong assessment.
What is the name of the pupil that responds to light accommodation?
The iris is flat and round. PERRLA (pupils equally round respond to light accommodation), illuminated and non-illuminated pupils constricts. Pupils constrict when looking at near object and dilate at far object. Pupils converge when object is moved towards the nose.
How long does it take for nails to return to normal color?
It is smooth and is intact with the epidermis. When nails pressed between the fingers (Blanch Test), the nails return to usual color in less than 4 seconds.
How far can a client read newsprint?
The client was able to read the newsprint held at a distance of 14 inches.
How many times does the eyelid close symmetrically?
Eyelids: There were no presence of discharges, no discoloration and lids close symmetrically with involuntary blinks approximately 15-20 times per minute.
What is intact chest wall?
Lungs / Chest: The chest wall is intact with no tenderness and masses. There’s a full and symmetric expansion and the thumbs separate 2-3 cm during deep inspiration when assessing for the respiratory excursion. The client manifested quiet, rhythmic and effortless respirations.
What is the color of the client's tongue?
The tongue of the client is centrally positioned. It is pink in color, moist and slightly rough. There is a presence of thin whitish coating.
What color are the lips of a client?
Mouth: The lips of the client are uniformly pink; moist, symmetric and have a smooth texture. The client was able to purse his lips when asked to whistle. Teeth and Gums: There are no discoloration of the enamels, no retraction of gums, pinkish in color of gums.
Head-To-Toe Assessment Nursing Experts
What Is A Head-To-Toe Assessment?
- A head-to-toe assessment refers to a physical examination or health assessment, and it becomes one of the many important components of understanding a patient’s needs and problems.
Head-To-Toe Assessment Basics
- Types of Assessments
There are several types of assessments that can be performed, says Zucchero. 1. A complete health assessmentis a detailed examination that typically includes a thorough health history and a comprehensive head-to-toe physical exam. This type of assessment may be performed by regist… - Length of Assessment
Ferere explains that the duration of the exam is directly in correlation to the patient’s overall health status. “Health patients with limited health histories may be completed in less than 30 minutes,” she says. “Many health practices have patients complete health history and pre-visit forms prior …
How to Prepare For The Assessment
- “Like all clinical settings, standard precautions (formerly universal precautions) should always be practiced with each and every patient to protect both the nurse and patient,” states Zucchero. “The primary goal of standard precautions is to prevent the exchange of blood and body fluids and includes hand hygiene, use of personal protective equipment, and safe handling and cleaning of …
Beginning An Assessment
- When beginning an assessment, Zucchero says, “establishing a personal relationship of trust and respect between the patient and the nurse is vital.” She adds that is it important throughout an assessment to assess how the patient is doing, and make sure they are properly draped and comfortable. She continued, “in addition, it’s important that an assessment is conducted system…
Seek Out Help from Mentors and Colleagues
- Ferere adds that new nurses should trust the foundational knowledge obtained in nursing school and seek strong, supporting nursing mentors as resources in health care delivery settings. “Confidence in assessment continues to grow with every completed assessment. Nurses should not be afraid to ask for help when something does not seem right and rely on your instincts and …
Popular Posts:
- 1. emory acwprth patient portal
- 2. chi memorial hospital chattanooga patient portal
- 3. myhealth24-7 patient portal
- 4. psychosocial report for a dimentia patient
- 5. patient portal poa
- 6. dental care of lake wylie patient portal
- 7. edmond dental patient portal
- 8. patient portal university of utah
- 9. osler medical patient web portal
- 10. shriners patient portal sign in