Genitourinary Tract Injuries | Conditions | UCSF Health
31 hours ago Purpose: To assess the spectrum of computed tomography (CT) findings in patients with genitourinary cancers visiting the emergency room (ER) and evaluate the relationship between CT findings and overall survival (OS). Methods: Retrospective analysis of consecutive patients with genitourinary cancers undergoing CT during an ER visit at a tertiary cancer center during a 20 … >> Go To The Portal
What is genital reconstruction?
What is UCSF urethra?
About this website
What does the emergency room do for UTI?
Going for urgent care for UTI When a patient visits an emergency room for urgent care for a UTI, the doctors may analyze the patient's urine sample to look for bacteria. The doctors will also look for red blood cells or white blood cells. Doctors may also use a urine culture.
What should you monitor when someone has a UTI?
Step 1: Assessing for UTI Patients should be asked about symptoms such as dysuria, frequency, urgency, suprapubic pain, flank pain or tenderness, fever, or hematuria in noncatheterized patients.
How do you check genitourinary?
Genitourinary Tract Injuries DiagnosisCatheterization Urinary catheters are tubes placed into the bladder to drain the urine. ... Abdominal Computed Tomography (CT) A computed tomography (CT) scan uses X-rays to produce detailed pictures of the body's internal structures, such as the abdomen.More items...
What are the priority nursing interventions for a patient experiencing a UTI?
Nursing ManagementAssess the symptoms of UTI.Encourage patient to drink fluids.Administer antibiotic as ordered.Encourage patient to void frequently.Educate patient on proper wiping (from front to the back)Educate patient on drinking acidic juices which help deter growth of bacteria.Take antibiotics as prescribed.More items...
How do you document a UTI?
Document urinary frequency or urgency, nocturia, bloody urine, incontinence, hesitancy or dysuria, and any associated pain or tenderness in the suprapubic, flank, or costovertebral angle (CVA) regions. Use a pain rating scale to assess pain.
What is the management of UTI?
Low-dose antibiotics, initially for six months but sometimes longer. Self-diagnosis and treatment, if you stay in touch with your doctor. A single dose of antibiotic after sexual intercourse if your infections are related to sexual activity. Vaginal estrogen therapy if you're postmenopausal.
What is the main role of the nurse during the genitourinary exam?
The nursing assessment of the genitourinary system generally focuses on bladder function. Ask about urinary symptoms, including dysuria , urinary frequency , or urinary urgency . Dysuria is any discomfort associated with urination and often signifies a urinary tract infection.
What is included in genitourinary?
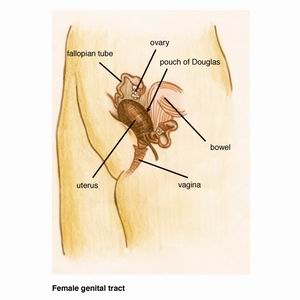
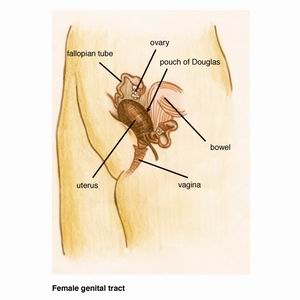
All organs involved in the production and excretion of urine plus all organs involved with reproduction. Organs of the genitourinary tract include the kidneys, bladder, fallopian tubes, and penis.
What does a genitourinary exam consist of?
Examination should involve inspection and palpation of: Prepuce, glans and foreskin - for example, to exclude a phimosis and signs of hypospadias. The skin should be examined for ulcers and rashes. The shaft of the penis is examined for plaques of Peyronie's disease.
What are the priority nursing diagnosis related to urinary elimination?
A lit- erature search combined with clinical observation and review of anatomy and physiology helped to identify five specific nursing diagnoses. They are: urinary retention, stress incontinence, urge incontinence, reflex incontinence, and uncontrolled incontinence.
How nurses can prevent urinary tract infections?
Several practices, often implemented in bundles, appear to reduce UTI or CAUTI in nursing home residents such as improving hand hygiene, reducing and improving catheter use, managing incontinence without catheters, and enhanced barrier precautions.
Ep 151 AKI Part 2 – ED Management
In this Part 2 of our AKI series we discuss the timing, volume and IV crystalloid of choice in AKI patients as well as dialysis indications and timing in light of the recent STARRT-AKI trial.
Ep 150 Acute Kidney Injury – A Simple Emergency Approach to AKI
In this first part of our 2 part podcast series on AKI we answer questions such as: Is there any value in the BUN:Cr ratio in distinguishing prerenal from intrarenal disease? Why is nephritic syndrome one of the most important intrarenal causes to pick up in the ED? Is there any value in urine electrolytes for the ED workup of AKI? Is there a role for bicarb in patients with severe AKI? How can we choose wisely when it comes to imaging for patients with AKI? How can we utilize POCUS best in working up the patient with AKI? What are the indications for ordering a CK to look for rhabdomyolysis? At what CK level do patients typically develop AKI? How can the McMahon score help us manage rhabdomyolysis? What is the value of urine myoglobin in the workup of rhabdomyolysis? What are indications for dialysis in patients with rhabdomyolysis? What are safe discharge criteria for patients with rhabdomyolysis? and many more....
Ep 144 Testicular Torsion: A Diagnostic Pathway
In this Part 2 of Urologic Emergencies EM Cases main episode podcasts Dr. Natalie Wolpert and Dr.
Ep 143 Priapism and Urinary Retention: Nuances in Management
This month's main episode podcast on Urologic Emergencies - Priapism and Urinary Retention asks: for priapism how much time to do we have to fix it before there’s irreversible tissue damage? How is priapism managed differently depending on the cause? What is the value of a corporal blood gas for managing priapism? What are the indications for cavernosal phenylephrine injections? What are the common medications that cause urinary retention that we often miss leading to needless recurrent urinary retention? Why is a suprapubic catheter in many respects safer than a urethral catheter for managing urinary retention? Which patients are at high risk for complications of post-obstructive diuresis? and many more....
Journal Jam 11 Post Contrast Acute Kidney Injury – PCAKI
Lauren Westafer joins Justin Morgenstern, Rory Spiegel and Anton Helman in a deep dive discussion on the world's literature on Post Contrast Acute Kidney Injury (PCAKI) in this Journal Jam podcast.
How many traumatic renal injuries are there in the world?
Worldwide, approximately 250,000 traumatic renal injuries occur annually. 1 The urological organ most commonly injured is the kidney, followed by the testicles and the bladder. 2 Depending on the data set used, renal and genitourinary (GU) trauma is present in 5% to 10% of all abdominal trauma patients. 3-5 Over the last 20 to 30 years, the care of renal and GU injuries has evolved, becoming more conservative and expectant. Advances in military medicine, where 5% of all combat injuries are GU-related, have accelerated the pace of this change and advances in care. 6
Is gross hematuria a good indicator of injury?
Gross hematuria is the best indicator of injury, but its absence does not rule out injury; in penetrating trauma, there is no correlation between the amount or even presence of hematuria and the degree of injury.
Is GU trauma a primary event?
Renal and GU trauma is rarely the “main event” in the sick polytrauma patient. ATLS guidelines, with good reason, mandate dealing with the life-threatening injuries first. However, genital trauma with marked physical examination abnormalities can and should be addressed on secondary or tertiary examination, with a plan in place for additional imaging, such as ultrasound, and appropriate subspecialty consultation. The time-sensitive nature of some genital trauma makes this especially important.
Do you need a RUG before a Foley catheter?
In any patient for whom you have a concern for possible urethral injury, based on history, physical examination, presence of significant pelvic fractures on x-ray, or suspicious findings on initial CT scan, you should perform a RUG prior to attempting placement of a Foley catheter. Without this test, you risk turning a minor urethral injury into a major one.
Is urinalysis necessary for trauma?
While a urinalysis can help risk stratify and identify the severity of some types of renal trauma, a normal urinalysis is not sufficient to rule out the diagnosis. There are many case reports of patients with severe injuries and normal urinalyses, especially in vascular injury and penetrating trauma. 2.
Can polytrauma be missed?
In polytrauma patients with other potentially life-threatening injuries, renal and genitourinary trauma may be overlooked initially, but a delayed or missed diagnosis of these injuries may result in preventable complications.
Can you see a ureteral injury with IV contrast?
A regular CT of the abdomen with IV contrast is not timed to catch most ureteral injuries. When the path of the projectile or stabbing implement, based on history or physical examination, is near a ureter or the kidney, delayed excretory images performed roughly 10 minutes after contrast administration are required.
Citation
Disclaimer: These citations have been automatically generated based on the information we have and it may not be 100% accurate. Please consult the latest official manual style if you have any questions regarding the format accuracy.
Clinical Findings
The clinician should attempt to identify the cause of the AKI, and uncover and treat life-threatening complications. A meticulous history of chronic medical conditions, recent illnesses, medications, intravenous (IV) contrast exposure should be obtained to elicit specific etiologies of AKI.
What causes oliguria and anuria?
Prerenal and postrenal causes are often elicited by the history and physical examination. It is helpful to determine the presence and severity of acute kidney injury (AKI) that frequently accompanies oliguria and anuria. Prerenal causes include hypovolemia, sepsis, and heart failure.
Is oliguria a prerenal or postrenal?
It is helpful to categorize the mechanism of oliguria or anuria as prerenal (eg, resulting from decreased or abnormal renal perfusion), renal (eg, resulting from intrinsic renal disease), or postrenal (eg, disease of the urinary collecting system distal to the renal parenchyma). Prerenal and postrenal causes are often elicited by ...
Popular Posts:
- 1. patient portal st barnanbas
- 2. rapid city medical center healow patient portal
- 3. gordon medical patient portal
- 4. silver summit patient login
- 5. after change of shift report which patient should the nurse assess first
- 6. carolina digestive patient login
- 7. harmony ob gyn patient portal
- 8. patient portal columbus regional hospital
- 9. unified women's healthcare of texas patient portal
- 10. southampton family pratice patient portal