Publication of case reports: Is consent required? - PMC
16 hours ago Following legal advice, the British Journal of Psychiatry has adopted a guideline saying that consent must be obtained if an individual patient is described; if consent cannot be obtained, “the report can be published only if all details that would enable any reader (including the individual or anyone else) to identify the person are omitted”. It is important to note that, particularly for … >> Go To The Portal
Do patients read consent forms?
They often do not read consent forms carefully because they assume that someone else has scrutinised the risks and benefits on their behalf. Interviews with 103 patients showed that many factors influence a decision to take part in medical research (Hastings Center Report 1996;26 (5):25-9).
Is your medical consent properly informed?
Informed consent to medical treatment is fundamental in both ethics and law. Patients have the right to receive information and ask questions about recommended treatments so that they can make well-considered decisions about care. Successful communication in the patient-physician relationship fosters trust and supports shared decision making.
What is a patient consent?
The physician provided his patient with a dense seven-page consent form, in which specific surgical risks, like tissue necrosis, were mentioned; she signed the consent form. However, the physician did not engage in any detailed discussions with his patient ...
Is informed consent possible?
Informed consent is not only required for clinical trials but is an essential prerequisite before enrolling each and every participant in any type of research involving human subjects including; diagnostic, therapeutic, interventional, bioequivalence, social and behavioral studies and for all research conducted domestically or abroad.
Do case reports require ethical approval?
Case reports and studies intended for quality improvement are often considered not research and do not need IRB approval. Nevertheless, there should be some processes of clearing those studies with respect to ethical handling of patients and related data.
When or in what case it is not necessary for informed consent?
Exceptions to Informed Consent Several exceptions to the requirement for informed consent include (1) the patient is incapacitated, (2) life-threatening emergencies with inadequate time to obtain consent, and (3) voluntary waived consent.
What do you need to write a case report?
Case reports should encompass the following five sections: an abstract, an introduction with a literature review, a description of the case report, a discussion that includes a detailed explanation of the literature review, and a brief summary of the case and a conclusion.
How do you consent a patient to a case report?
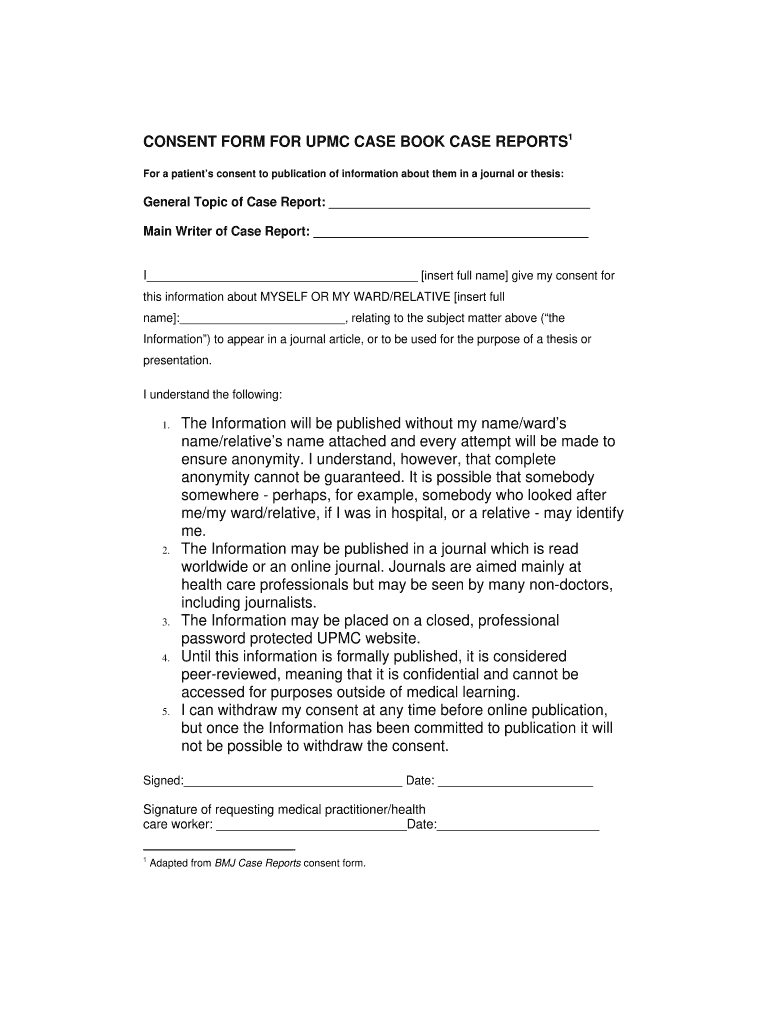
For a patient's consent to publication of information about them in a journal or thesisThe Information will be published without my name/child's name/relatives name attached and every attempt will be made to ensure anonymity. ... The Information may be published in a journal which is read worldwide or an online journal.More items...
Is informed consent required?
Informed consent is required for any investigation or treatment proposed to a patient. Understanding of the nature of procedure, benefits and risks are the cornerstones of informed consent. While autonomy is one of the four main ethical principles, I argue that there is no absolute right to autonomy or consent.
Is informed consent always required?
Informed consent always must be voluntary (45 CFR 46.116). IRBs should ensure that non-financial incentives are not so great as to diminish the voluntariness of consent or cloud someone's appreciation of risks or potential benefits that might be gained from participating in a study (45 CFR 46.116).
Can medical students write case reports?
By writing case reports, medical students can contribute to the first line of evidence for developing new therapies [6–8].
What is clinical case report?
WHAT IS A CLINICAL CASE REPORT? A case report is a detailed report of the symptoms, signs, diagnosis, treatment, and follow-up of an individual patient. Case reports usually describe an unusual or novel occurrence and as such, remain one of the cornerstones of medical progress and provide many new ideas in medicine.
What is the purpose of the case report form?
A Case Report Form (CRF) is a printed or electronic document that is created and used in clinical trial research to capture standardised clinical data from each patient separately and to transfer it to Data Management.
Can I publish a case study?
Submit your case study through your chosen channel's online submission site, find author support and understand your next steps to publish your case study.
What is required to submit a case report?
Journals often have specific requirements for publishing case reports, which could include a requirement for informed consent, a letter or statement from the IRB and other things.
Why is it important to write a case report?
the reason you would go to the trouble of writing one, is that the case is sufficiently unique, rare or interesting such that other medical professionals will learn something from it.
What is a case report?
What is a case report? A medical case report, also known as a case study, is a detailed description of a clinical encounter with a patient. The most important aspect of a case report, i.e. the reason you would go to the trouble of writing one, is that the case is sufficiently unique, rare or interesting such that other medical professionals will learn something from it.
Does CHM have funding for publication?
It is best practice to check the journal's Info for Authors section or Author Center to determine what the cost is to publish. CHM does NOT have funds to support publication costs, so this is an important step if you do not want to pay out of pocket for publishing.
Do you need informed consent for a case report?
Although not technically required, especially if the case report does not include any identifying information, some journals require informed consent for all case reports. The CARE guidelines recommend obtaining informed consent AND the patient's perspective on the treatment/outcome (if possible).
Do journals have informed consent?
Journals may have their own informed consent form that they would like you to use, so please look for this when selecting a journal. Once you've identified the case, selected an appropriate journal (s), and considered informed consent, you can collect the required information to write the case report.
Does HIPAA apply to case reports?
First, you will be collecting protected health information, thus HIPAA applies to case reports. Spectrum Health has created a very helpful guidance document for case reports, which you can see here: Case Report Guidance - Spectrum Health. While this guidance document was created by Spectrum Health, the rules and regulations outlined could apply ...
How to write a case report?
This can be accomplished by arranging the events in chronological order, being specific about your differential diagnostic considerations, elucidating the arguments for your clinical decision-making process, and following up to round off the story neatly. This will create an imaginary journey where your readers can follow every development of the case and understand why you have performed specific tests or made certain decisions during a particular treatment.
Why are case reports important?
As a method of documenting a single clinical observation, case reports offer timely and valuable information , especially with regards to rare diseases. They show medical professionals how fellow practitioners have acted in similar situations and thus aid in the decision-making process by sharing best practices.
What happens if a case is unique but not well documented?
This is not only a waste of your precious time but also a discouragement which might prevent you from producing more case reports in the future.
What to include in a case report for differential diagnosis?
You can also include in your case reports descriptions of actual values for blood test results, detailed dosages for medications prescribed or other variables that should be taken into account with respect to the outcome of the situation.
Who are the editors of Medical Mycology Case Reports?
To assist researchers with this task, Professors Oliver Kurzai and Adilia Warris, editors of the journal Medical Mycology Case Reports shared tips on writing high impact case reports in the latest Researcher Academy webinar. We are pleased to share here some quick do’s and don’ts from the webinar.
Can you publish a case report without consent?
Don’t publish a case report without the patient’s consent. As explained above, informed patient consent is mandatory for the publication of your case reports. Ignoring this requirement can result in a rejection for your work and worse, ruin your relationship and reputation with patients.
Do clinical practitioners have to disclose patient information?
Don’t forget, moreover that clinical practitioners are not required to, and should not reveal personal patient information to a journal that is not relevant to the case.
When publishing personal information about identifiable living patients, do we require a signed copy of our patient consent permission form?
This form is available as a pdf and in multiple languages.
What happens if a patient has not seen the final version of the manuscript?
If the patient has not seen a final version of the manuscript to be submitted to BMJ, the form must be amended to make clear what the patient has seen and that they have agreed to publication without having seen the final version of the manuscript.
What is a case report?
A case report is a medical/educational activity that does not meet the DHHS definition of “research”, which is: "a systematic investigation, including research development, testing and evaluation, designed to develop or contribute to generalizable knowledge.".
What happens if the author strips off all HIPAA identifiers?
If the author strips off all HIPAA identifiers, but the information associated with the subject of the article includes a “unique characteristic” which would make it identifiable to the subject, or the author has actual knowledge that the information about the subject could be used alone or in combination with other information to identify the subject, the author must contact the HIPAA Privacy Officer to discuss the required steps to take prior to publication.
Do you need a privacy authorization for an article?
Authors who remove HIPAA identifiers (including unique patient characteristics) from the data prior to submission and publication of the article do not need to obtain a signed privacy authorization.
Does a case report have to be approved by the IRB?
Yes. Under HIPAA, a case report is an activity to develop information to be shared for medical/educational purposes. Although the use of protected health information to prepare the paper does not require IRB review, the author of a case report must comply with HIPAA.
Do journals require an IRB letter?
Background: Many journals now require a letter, or other acknowledgement, from an IRB prior to publication of a case report. Specifically, they wish to know whether IRB approval was obtained or was not required for the described case. The JHM IRBs have adopted a policy to address the following question and answers.
How to make an eSignature for a PDF document online
Are you looking for a one-size-fits-all solution to eSign do you need consent to write a case report? signNow combines ease of use, affordability and security in one online tool, all without forcing extra ddd on you. All you need is smooth internet connection and a device to work on.
Find out other Do You Need Consent To Write A Case Report
If you believe that this page should be taken down, please follow our DMCA take down process here.
How to select a case for the case report?
Every case is unique in a way, but every case cannot be reported. I am giving you some pointers on how to select a good case and ensure it gets published after all those writing efforts – the next time you go to your clinic, document the case if you observe any of the following:
Structure of a case report
Case reports are shorter than most other types of articles. They consist of the following six sections:
Abstract
An abstract is not compulsory, but it is always better if you give one. The abstract should summarize the case, the problem it addresses, and the message it conveys. Abstracts of case studies are usually short (preferably not more than 200 words) and unstructured (not subdivided into different headings but a single paragraph).
Introduction
The introduction gives a brief overview of the problem that the case addresses, citing relevant literature where necessary. It should provide background information on why the case is worth reading and publishing. The introduction generally ends with a single sentence describing the diagnosis and treatment plan executed.
Case description
The case description or summary is the focus of the case report. The case should be best presented in enough detail for the reader to establish his or her own conclusions about the case's validity.
Discussion
The discussion is the most important section of the case report. It interprets the key findings of the case report, contrasts the case report with what is already known in the literature to justify its uniqueness and draws clinically useful conclusions.
Conclusion
The author should provide the main conclusion of the case report based on the evidence reviewed in the discussion section. A concise statement of the lesson to be learnt from the case could be stated. Here, the author can give suggestions and recommendations to clinicians, teachers, or researchers.
