How to Write a Discharge Summary - Geeky Medics
1 hours ago Discharge summary reports play a vital role in informing the immediate family about the patient’s condition during the duration of his or her stay in the hospital. It has to provide true details about the patient in observance of the hospital’s protocols. Following the right contents would make it concise and accurate. >> Go To The Portal
What is a discharge summary from a hospital? A discharge summary is a clinical report created by health professionals that contains the specifics of a patient’s hospitalization and is given to the patient after the patient has been discharged.
How to write a discharge summary?
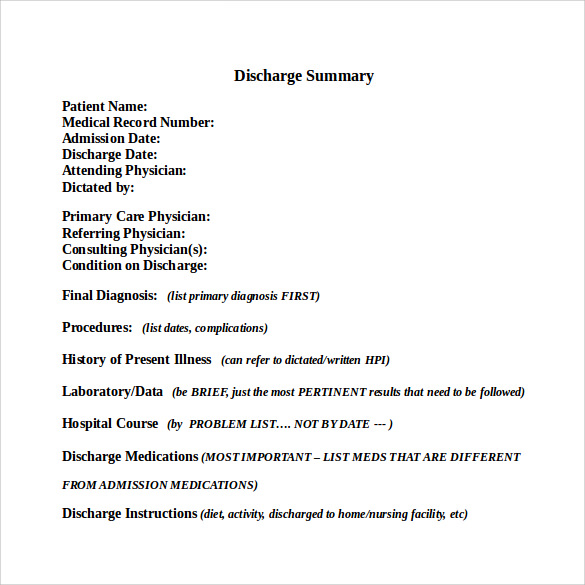
Discharge Summary Template Date of Admission: Date of Discharge: Attending Physician: (should be the attending on the day of discharge) PCP: (must include the name of the PCP or clinic, “out of town” not acceptable) Admission Diagnosis: This should be the reason for admission (e.g. dehydration, respiratory distress, hypoxia, abdominal pain), not the discharge diagnosis.
What should be included in a hospital discharge summary?
Your discharge plan should include information about where you will be discharged to, the types of care you need, and who will provide that care. It should be written in simple language and include a complete list of your medications with dosages and usage information. How do you write a discharge summary? Demographics. Clinical details.
What is the definition of discharge summary?
discharge condition information is a concern and may affect patient safety. Introduction . Hospital discharge summaries serve as the primary documents communicating a patient’s care plan to the post-hospital care team. 1, 2. Often, the discharge summary is the only form of communication that accompanies the patient to the next setting of care. 1
What is a hospital discharge summary?
A discharge summary is a physician -authored synopsis of a patient’s hospital stay, from admission to release. It’s a communication tool that helps clinicians outside the hospital understand what happened to the patient during hospitalization.

What is included in patient discharge summary?
A discharge summary is a physician-authored synopsis of a patient's hospital stay, from admission to release. It's a communication tool that helps clinicians outside the hospital understand what happened to the patient during hospitalization.
What is the purpose of a discharge summary?
Hospital discharge summaries serve as the primary documents communicating a patient's care plan to the post-hospital care team. Often, the discharge summary is the only form of communication that accompanies the patient to the next setting of care.
What are discharge papers from hospital?
What is a Hospital Discharge Paper? A Discharge Paper is a sample form only for patients who are ready to leave the clinic or hospital. Through this form, there will be a smooth, easy process for both patients and staff. Before discharging patients from the hospital, certain information must be on file.
What information is included in the Nurses discharge note?
A written transition plan or discharge summary is completed and includes diagnosis, active issues, medications, services needed, warning signs, and emergency contact information. The plan is written in the patient's language.
What are discharge reports?
A discharge summary refers to a clinical report prepared by health professionals that outlines the details of the hospitalization of a patient. Lack of discharge details, diagnosis information or patient's health status in discharge summaries can lead to poor treatment plans.
When should a discharge summary be sent?
In addition, discharge summaries often lack important information such as updated discharge medications and follow-up plans. The Joint Commission has identified a standardized, written discharge summary completed within 30 days of hospital discharge as a key transition of care element to improve patient outcomes.
Does a discharge summary require an exam?
A: According to coding guidelines, discharge services should include a final examination when appropriate, so the general consensus is that you do need to perform one.
Do hospitals always give discharge papers?
Typically, when you're discharged from the hospital, a discharge planner or team will meet with you to go over the information you need before you go home. They'll provide a set of hospital discharge papers to you, which will list all the procedures and treatments that you received during your hospital stay.
Is a discharge summary required for observation?
All inpatient encounters require an electronic discharge summary – even if the patient leaves against medical advice or expires. This can be dictated or typed, but must be in electronic format. For observation and same day surgery patients, there are several options.
How do you write a nursing discharge summary?
6 Components of a Hospital Discharge SummaryReason for hospitalization: description of the patient's primary presenting condition; and/or. ... Significant findings: ... Procedures and treatment provided: ... Patient's discharge condition: ... Patient and family instructions (as appropriate): ... Attending physician's signature:
Can a nurse write a discharge summary?
If you are an advanced practice nurse and providing care to a patient, authoring a discharge summary on your own is well within your scope of practice under your state nurse practice act and its rules.
Who is responsible for the discharge summary?
Interpretive Guidelines §484.48 - The HHA must inform the attending physician of the availability of a discharge summary. The discharge summary must be sent to the attending physician upon request and must include the patient's medical and health status at discharge.
Is there a process to follow in doing a patient discharge?
When you leave the hospital after a treatment, you will be issued a patient discharge summary. This is to be written and signed by the attending ph...
When can a patient be discharged?
A hospital will be able to discharge a patient when he or she no longer needs inpatient treatments. They can also discharge you if they are to tran...
Is the patient accompanied by a health worker during a discharge?
The patient will be accompanied by a medical personnel because it is part of the hospital's protocol. Some medical personnel would still assess you...
What is at the end of discharge summary?
At the end of every discharge summary is the signature of the attending physician. It could be electronic or physical. The six (6) components stated already serves a great foundation but it would be more accurate to add more on the list to improve patient safety. This includes:
Why is discharge summary important?
Importance of Discharge Summary 1 It helps improve the discharge process – individuals assigned in the transition of a patient would always look for ways to improve the discharge process. this includes the discharge planning, enlisting of medications and follow-up appointments. 2 It serves as the mode of communication between the hospital care team and aftercare.
What happens when you leave a hospital?
When you leave the hospital after a treatment, you will be issued a patient discharge summary. This is to be written and signed by the attending physician together with the necessary details of the patient during his or her stay.
Why is a discharge summary important?
A discharge summary template plays an important role in maintaining the safety of patients after getting discharged from the hospital. The summary serves as the main document that communicates the care plan of a patient to the post-hospital healthcare team. In most cases, a hospital discharge form is the only document that accompanies a patient ...
What does it mean when a patient is discharged from the hospital?
When a patient is discharged from the hospital, it signifies that there is improvement in his/her health and is fully or almost back to normal. But have you ever wondered how doctors and other members of the medical care team make sure that the medical care given to patients is properly recorded? They do this by using a discharge summary template. Here’s how you can create it.
What is discharge form?
In most cases, a hospital discharge form is the only document that accompanies a patient to the next stage of medical care. Well-written discharge summaries are typically considered important when promoting safety when a patient transitions between care settings, especially during the initial post-hospital period.
What is significant findings?
Significant findings. These refer to the doctor’s primary diagnoses. The procedures done and the treatment provided. This refers to a description of the events that occurred during hospital stay or a description of medical, surgical, allied health consults or other specialties that patient has experienced.
What is discharge summary?
August 20, 2018. A discharge summary plays a crucial role in keeping patients safe after leaving a hospital. As an Advances in Patient Safety report notes, "Hospital discharge summaries serve as the primary documents communicating a patient's care plan to the post-hospital care team. Often, the discharge summary is the only form ...
How many components are in a discharge summary?
As a For the Record report points out, The Joint Commission mandates all discharge summaries must contain six high-level components , which are also noted as requirements in the National Quality Forum's Safe Practices for Better Healthcare.
What is discharge summary?
A discharge summary is a kind of document which has all the necessary details about the health condition of a patient and their time in a hospital. All the information are written concisely. Any forms of ambiguity are avoided for understanding. If you are looking for creating a discharge summary, make sure you include the following points. Sometimes, every physician gives a different discharge summary. It should consist of the following points: 1 Patients’ information, such as their name, address, gender, date of birth, contact number, and, emails. 2 Details of the physician, such name, their position, and their contact numbers are included in the discharge summary. 3 Admission and discharge information, such as the date of admission, the signs, and symptoms of the illness, hospital name, discharge date, 4 Medical care in the hospital includes the list of medication given in the hospital 5 The continuing plan of medication consists of the followup checkups and medication required for the patient.
Why is discharge summary important?
A discharge summary is useful to auditors, other physicians, nurses, lawyers, and other members of the healthcare team since it lets them know the medical interventions done for the patient and how they can proceed with their own care plans for the patient. To facilitate hospital recovery audits.
What is recovery audit?
A recovery audit is done by government-contracted recovery auditors. They investigate thousands of discharge summary templates each day and spot discrepancies on the payments provided, the patient claims, and the treatment provided to the patient.
Do all hospitals have to have a discharge summary?
In the United States, there is no single dis charge summary form created but most healthcare institutions follow the same guidelines in their discharge summary templates. Listed below are the most important items that should be included in a discharge summary.
Do physicians have to store patient history?
This way, physicians and hospital clerks do not have to store and lug around an individual’s entire patient history every time a physician requests for it. This document, however, is not created solely for the benefit of the hospital. These reasons will be discussed in the next few paragraphs.
Do physicians write discharge summaries?
Physicians are required to write discharge summaries for all their patients whether they recover from their illnesses or not. Aside from being a mandatory sample policy, we have listed below the numerous other uses of discharge summaries that every member of the healthcare team should know.
Demographics
- Patient details
Important information to include regarding the patient includes: 1. Patient name: full name of the patient (also the patient’s preferred name if relevant) 2. Date of birth 3. Unique identification number 4. Patient address: the usual place of residence of the patient 5. Patient telephone num…
Future Management
Medications
Allergies and Adverse Reactions
Person Completing Record
Other Sections That May Be Included
References
Popular Posts:
- 1. vca patient portal login
- 2. how do i share my patient portal info with a spouse
- 3. chalian and leak patient "portal"
- 4. winooski family health patient portal
- 5. what symptoms is the patient asked to report during exercise electrocardiography quizlet
- 6. crystal pm patient portal
- 7. promedica billing
- 8. epowerdoc patient health portal
- 9. bonsecours patient portal
- 10. kearney clinic patient portal