FREE 14+ Patient Report Forms in PDF | MS Word
7 hours ago Time = total time spent evaluating, managing, and providing care to a critically ill patient. Does not have to be continuous. Includes direct patient care at bedside as well as time spent reviewing test results, discussing the case with consultants or family members, and documenting in the patient's chart. Time Calculation. Time spent in ... >> Go To The Portal
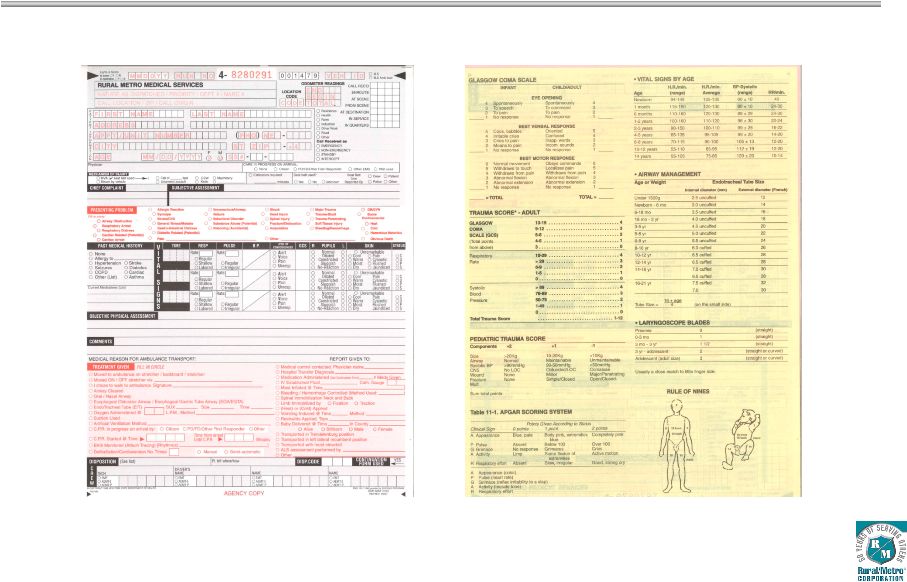
What is a patient care report?
A patient care report is a document written by medical professionals to report about the patient’s wellbeing, care and status. This document consists of the result of the assessment and the evaluation of the patient being done by the EMTs or the EMS.
What is the proper documentation of critical care services?
Documentation must be specific to the patient. In the age of electronic medical records, it is imperative the physician avoid cloned notes. As an example of proper documentation of critical care services, the physician might specify, “I spent 180 minutes of critical care time excluding the procedure time.
What should be included in a critical care note?
Critical care notes do not have specific bulleted items; therefore, it is imperative the documentation contain enough information to distinguish critical care from other E/M services. For example, “The patient is stable but remains critical at this time.
Is there a handoff report template for Critical Care Nurses?
Here is the template that we use: This report sheet is designed specifically for critical care nurses but it would work in any nursing setting. Here are the steps to a great ICU handoff report: This is really all that you need to do to give an amazing report . . . and you need to do it in this order.

How do I write a good ICU report?
0:004:23How to Give ICU Report - YouTubeYouTubeStart of suggested clipEnd of suggested clipSo starting with general information that would include information like the patient's name theirMoreSo starting with general information that would include information like the patient's name their date of birth. Their weight their admitting diagnosis.
How do you write a nursing patient report?
How to write a nursing progress noteGather subjective evidence. After you record the date, time and both you and your patient's name, begin your nursing progress note by requesting information from the patient. ... Record objective information. ... Record your assessment. ... Detail a care plan. ... Include your interventions.
How do I report an ICU nurse?
0:1411:43How to Give a Good Nursing Shift Report (with nursing report sheet ...YouTubeStart of suggested clipEnd of suggested clipEach time you give report during your first year as a nurse. This is not a brain sheet or a sheetMoreEach time you give report during your first year as a nurse. This is not a brain sheet or a sheet for you to work from during your shift.
How do you give a patient a report?
18:5620:45How to Give a Nursing Shift Report - YouTubeYouTubeStart of suggested clipEnd of suggested clipSo you always just want to know who the family is and if you don't always look through the chart ifMoreSo you always just want to know who the family is and if you don't always look through the chart if the nurse doesn't know look through the chart. Because believe it or not to the patient.
What should a nursing report include?
What to cover in your nurse-to-nurse handoff reportThe patient's name and age.The patient's code status.Any isolation precautions.The patient's admitting diagnosis, including the most relevant parts of their history and other diagnoses.Important or abnormal findings for all body systems:More items...•
What is the format for report writing?
Report writing is a formal style of writing elaborately on a topic. The tone of a report and report writing format is always formal. The important section to focus on is the target audience. For example – report writing about a school event, report writing about a business case, etc.
What is SBAR report?
SBAR (Situation, Background, Assessment, Recommendation) is a verbal or written communication tool that helps provide essential, concise information, usually during crucial situations. In some cases, SBAR can even replace an executive summary in a formal report because it provides focused and concise information.
How do you organize a nursing report sheet?
0:1210:04Nurse Brain Sheet | ORGANIZE YOUR NURSING SHIFT | Nursing ReportYouTubeStart of suggested clipEnd of suggested clipOrganization tips for you to be successful during your nursing shift the main one being a reportMoreOrganization tips for you to be successful during your nursing shift the main one being a report sheet and this is what people call their nurse brains.
How do I report a nursing assessment?
The following are comprehensive steps to write a nursing assessment report.Collect Information. ... Focused assessment. ... Analyze the patient's information. ... Comment on your sources of information. ... Decide on the patient issues.
How do you make a report?
Know your audience. Before you begin writing, be sure you understand who the report is for, why they need the information and what you want them to do after reading it. Knowing your audience will help you guide your style and ensure you communicate your information as efficiently as possible. Proofread carefully.How to Write a Report in 7 Steps | Indeed.comhttps://www.indeed.com › career-development › how-to-...https://www.indeed.com › career-development › how-to-...Search for: How do you make a report?
What questions should a nurse consider when receiving a report?
Questions to Ask During Nursing Report:Does that patient have any family?Who is the patient's primary contact if something was to happen?Does the patient have any type of testing that they must be NPO for?Does the patient need assistance eating, showering, or using the bathroom?More items...Questions to Ask During Nurse Shift to Shift Report About Your Patienthttps://www.registerednursern.com › nursing-report-questi...https://www.registerednursern.com › nursing-report-questi...Search for: What questions should a nurse consider when receiving a report?
Who Writes the Patient Medical Report?
Health care providers do the patient medical report. The health care professionals make the documentation for a patient. It includes all the physic...
Who Can Have Access to a Patient Medical Report?
The health care providers have the access to the patient medical report. They keep the medical report as a history of medical records. Also, patien...
Is a Patient Medical Report a Legal Document?
If it is signed by a health care professional, then it is a legal document. It is permissible in any court of law. It is an evidence that the patie...
What is critical care time?
Elements of Critical Care Time. Critical illness or injury = illness or injury that impairs one or more "one or more vital organ systems such that there is a high probability of imminent or life threatening deterioration in the patient’s condition.”. Critical care services = direct medical care for the patient that involves “high complexity ...
What is CPT code 99291?
CPT Code 99291 is used for the first 30-74 minutes of critical care time. CPT Code 99292 is used for additional blocks of time of up to 30 minutes beyond the first 74 minutes of critical care time. Must document either a specific time or, e.g., "in excess of 30 minutes".
Giving Hand-Off Report in the ICU
Luckily, I had an amazing preceptor. During the first few shifts she sat closely behind my shoulder to monitor where my skills and knowledge base were currently at, acting as a resource as needed.
How to Give an ICU Handoff Report
This report sheet is designed specifically for critical care nurses but it would work in any nursing setting. Here are the steps to a great ICU handoff report:
What are you struggling with in nursing school?
NURSING.com is the BEST place to learn nursing. With over 2,000+ clear, concise, and visual lessons, there is something for you!
Why is critical care documentation important?
Critical Care services (99291-99292) are time-based, and improper documentation of time is a frequent reason that payers deny payment for these services. Educating providers to document time appropriately will help to maximize reimbursement and reduce additional documentation requests (ADRs).
Why is document time important in critical care?
Educating providers to document time appropriately will help to maximize reimbursement and reduce additional documentation requests (ADRs). The American Medical Association (AMA) defines critical care as the direct delivery by a physician (s) or other qualified healthcare professional of medical care for a critically ill or critically injured ...
What should documentation focus on?
Therefore, documentation should focus on what transpired from the last time the patient was seen until the present; listing all circumstances that emerged that effect the current plan of care.
What is the CPT requirement for reporting?
CPT® guidelines require that the report ing provider must devote his or her full attention to the patient during the time specified as critical care, and therefore cannot provide services to any other patient during the same time. Documentation must be specific to the patient.
Can a provider document start and stop times?
As an alternative to documenting total critical care time, the provider may document start and stop times. When doing so, the provider must be careful not to count critical care time for any services not directly related to care of the critical patient.
What is a Patient Medical Report?
A patient medical report is a comprehensive document that contains the medical history and the details of a patient when they are in the hospital. It can also be given as a person consults a doctor or a health care provider. It is a proof of the treatment that a patient gets and of the condition that the patient has.
What You Should Include in a Patient Medical Report
A patient medical report has some important elements that you should not forget. Include all these things and you can learn how to write a patient medical report.
Importance of a Patient Medical Report
The reason why a patient medical report is always given is because it is important. Here, you can know some of the importance of a patient medical report:
How to Write a Good Patient Medical Report
A doctor is a doctor. They are not writers. They can be caught in a difficulty on how to write a patient medical report. If this is the case, turn to this article and use these steps in making a patient medical report.
Who Writes the Patient Medical Report?
Health care providers do the patient medical report. The health care professionals make the documentation for a patient. It includes all the physicians, nurses, and doctors of medicine. It also includes the psychiatrists, pharmacists, midwives and other employees in the allied health.
Who Can Have Access to a Patient Medical Report?
The health care providers have the access to the patient medical report. They keep the medical report as a history of medical records. Also, patients’ access to the patient medical report is a must. It is their right to see their medical report. It is against the law not to show them their medical report.
Is a Patient Medical Report a Legal Document?
If it is signed by a health care professional, then it is a legal document. It is permissible in any court of law. It is an evidence that the patient is under your care. Thus, it can be used in court as an essential proof. So, keep a patient medical report because you may need it in the future.
What Is a Patient Care Report?
We often hear of care reports based on by medical teams or by medical authorities. Yet, we are not sure how this differs from the kind of report that is given to us by the same people. So this is the time to make it as clear as possible.
How to Write a Patient Care Report?
Where do you even begin when you write a patient care report? A lot of EMS or EMTs do know how to write one since they are trained to do so.
What is a patient care report?
A patient care report is a document made mostly by the EMS or EMTs. This documented report is done after getting the call. This consists of the information necessary for the assessment and evaluation of a patient’s care.
What should not be written in a patient care report?
What should be avoided in a patient care report is making up the information that is not true to the patient. This is why you have to be very careful and very meticulous when writing these kinds of reports. Every detail counts.
Who is in charge of reading the patient care report?
The person or the people who will be reading the report are mostly medical authorities. When you are going to be passing this kind of report, make sure that you have all the information correctly. One wrong information can cause a lot of issues and problems.
What is reporting in nursing?
In medical circles, reporting refers to the act of transferring relevant information. In most cases, this information refers to the patient information that is transferred from one nurse to another during the change of shift. There are numerous occasions that require reporting.
What is a nursing report sheet?
The report sheets enable the nurses to record clear information regarding details including the diagnosis, history, allergies, consults, vital signs, lab results, and other such health-related data. Due to their excellent recording system, nursing report sheets are used by physicians, doctors, nurses and other healthcare staff all over the world. ...
Why is a mental health nursing report important?
It allows nurses and doctors to continue treating and providing care to their patients even when during shift interchange.
Why is it important to have an ICU nurse report?
Due to this, it is very important that nurses are able to gather the required information. To help with this situation, ICU Nursing Reports were brought into action. ICU Nursing Reports are used to obtain a list of essential details regarding the patient who has been admitted to the ICU.
Why do nurses use advance notes?
Advance notes to prompt nurses about the duties that they need to perform in the next shift. Moreover, nursing report sheets play a huge role in favor of the nurse’s life as well. Due to the vast expanse of the information present, a lot of nurses consider the reports to be akin to a secondary brain.
What is the purpose of the General Information section in a nursing report?
This section is responsible for generating all the details regarding the patient such as Date of Birth, Gender etc. of the patient.
What is flow sheet in nursing?
A6. In simple terms, a flow sheet is a single or dual-page form, tasked with the job of gathering all important aspects of a patient’s condition. Similar to the other nursing reports, the flow sheet is tasked with gathering patient information.
What Is Patient Incident Report?
Incidents are potentially dangerous incidents that have the potential to put patients or staff members at risk. Medical events are anything that can happen in the healthcare industry and can be caused by anything from equipment failure to injuries to poor patient care. Medical events can occur for a variety of reasons.
What Is the Purpose of the Patient Incident Report?
Patient incident reports provide information to facility officials about what happened to the patient. The information provided in the reports provides light on the steps that must be performed in order to deliver excellent patient care while also maintaining the smooth operation of your facility.
What to Include in a Patient Incident Report?
A patient incident report should include the bare minimum of information regarding the occurrence, such as who was involved, what happened, where it happened, when it happened, and how it happened. You should also include ideas on how to deal with the problem in order to lessen the likelihood of further instances occurring.
What Are the Benefits of Patient Safety Reporting?
Setting the relevant key performance indicators in your organization gets easier as a result of healthcare data analysis and analysis. You can receive the following significant advantages from filing a complaint:
Types of Incident Report
Even if an occurrence appears to be insignificant or has not resulted in any harm, it is still crucial to record it. Whether a patient has an allergic response to a drug or a visitor slips over an electrical cord, these occurrences provide valuable insight into how your facility can create a better, more secure environment for its visitors.
How to Create an Efficient Patient Incident Report
One thorough incident report should address all of the fundamental questions — who, what, where, when, and how — and provide full answers. The majority of hospitals adhere to a predetermined reporting format that is tailored to their own organizational requirements. An incident report, on the other hand, must include the following information:
FAQs
It is possible to acquire information on patient safety occurrences through the use of incident-reporting systems (IRSs). Even if they come with a significant financial cost, however, little is known regarding their usefulness.
Criteria
Brief reports are suitable for the presentation of research that extends previously published research, including the reporting of additional controls and confirmatory results in other settings, as well as negative results. Authors must clearly acknowledge any work upon which they are building, both published and unpublished.
Preparing your manuscript
The information below details the section headings that you should include in your manuscript and what information should be within each section.
Abstract
The abstract should briefly summarize the aim, findings or purpose of the article. Please minimize the use of abbreviations and do not cite references in the abstract.
Declarations
All manuscripts must contain the following sections under the heading 'Declarations':
Figures, tables and additional files
See General formatting guidelines for information on how to format figures, tables and additional files.
Popular Posts:
- 1. my centura patient portal
- 2. banner del webb hospital patient portal
- 3. dr padma ram patient portal
- 4. lauren broadway patient portal
- 5. pcifm patient portal forgot username
- 6. nextmd login
- 7. rmi flint patient portal
- 8. desert psychiatric patient portal
- 9. east uhs patient portal
- 10. after receiving your report which patient should you assess first