Systematic Assessment of Patients With Unexplained …
1 hours ago · A patient in cardiac arrest is treated in multiple different stages. The interventions that have proven to reverse cardiac arrest include early CPR and early defibrillation. The initial step involves identification and basic life-support measures. If public access defibrillation is available, it should be activated and utilized if needed. >> Go To The Portal
How should cardiac arrest care be documented?
Arrest Documentation Quick Reference When documenting cardiac arrest care, the following items should be documented at applicable times and listed intervals. Each attempt at an intervention must be listed individually as successful or unsuccessful. (Except Chest Compressions)
What tests are performed in the evaluation of cardiac arrest?
A quick head-to-toe assessment will help guide treatment. Evaluation While treating a patient in cardiac arrest, little to no blood or imaging testing is necessary. If one can obtain point-of-care testing, a potassium and glucose level may be beneficial.
When should cardiology be consulted in the evaluation of cardiac arrest?
If the medical cardiac arrest is deemed secondary to a primary cardiac etiology, cardiology should be consulted to see what intervention is appropriate. Deterrence and Patient Education
What is a cardiac arrest?
As defined by the American Heart Association and the American College of Cardiology, "(sudden) cardiac arrest is the sudden cessation of cardiac activity so that the victim becomes unresponsive, with no normal breathing and no signs of circulation. If corrective measures are not taken rapidly, this condition progresses to sudden death.
How do you assess for cardiac arrest?
Diagnosis of Cardiac Arrest Imaging Tests – such as chest X-ray, echocardiogram, computed tomography (CT) scan, magnetic resonance imaging (MRI) or a nuclear scan that identifies blood flow problems in the heart. Clinical Laboratory Tests – such as an electrocardiogram (EKG) or coronary catheterization (angiogram)
What should you monitor after cardiac arrest?
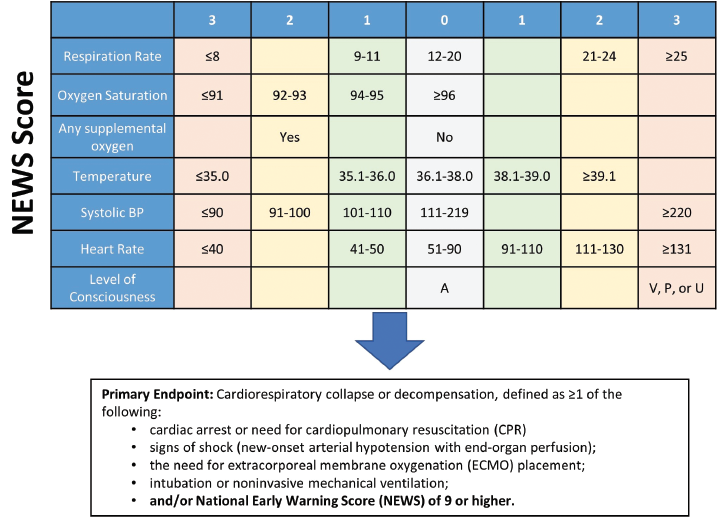
Continuous cardiac monitoring, pulse oximetry, capnography and NIBP (non-invasive blood pressure) monitoring should be initiated. This provides critical information on tissue oxygenation and perfusion and helps guide further resuscitative care.
What are the 5 signs of cardiac arrest?
Call 911 or emergency medical help if you experience any of these signs and symptoms:Chest pain or discomfort.Heart palpitations.Rapid or irregular heartbeats.Unexplained wheezing.Shortness of breath.Fainting or near fainting.Lightheadedness or dizziness.
What are the 4 cardiac arrest rhythms?
Four rhythms produce pulseless cardiac arrest: ventricular fibrillation (VF), rapid ventricular tachycardia (VT), pulseless electrical activity (PEA), and asystole. Survival from these arrest rhythms requires both basic life support (BLS) and advanced cardiovascular life support (ACLS).
What is post cardiac arrest care?
Subsequent objectives of post–cardiac arrest care are to. Control body temperature to optimize survival and neurological recovery. Identify and treat acute coronary syndromes (ACS) Optimize mechanical ventilation to minimize lung injury. Reduce the risk of multiorgan injury and support organ function if required.
How do you assess brain damage after cardiac arrest?
BLOOD BIOMARKERS Measurement of brain-derived markers in the blood is probably the most obvious and potentially straightforward way to quantify brain injury after cardiac arrest. Neuron-specific enolase (NSE) is the only marker included in the current ERC/ESICM algorithm.
What are the 4 main signs of cardiac compromise?
The following signs and symptoms are often associated with cardiac compromise:Pain, pressure, or discomfort in the chest or upper abdomen (epigastrium)Dyspnea.Palpitation.Sudden onset of sweating and nausea or vomiting.Anxiety (feeling of impending doom)Abnormal pulse.Abnormal blood pressure.
What are 3 causes of cardiac arrest?
The main causes of cardiac arrest related to the heart are:a heart attack (caused by coronary heart disease)cardiomyopathy and some inherited heart conditions.congenital heart disease.heart valve disease.acute myocarditis (inflammation of the heart muscle).
What is the main assessment indicator of a sudden cardiac arrest in an unresponsive victim?
The signs are: Sudden loss of responsiveness – The person doesn't respond, even if you tap them hard on the shoulders or ask loudly if they're OK. The person doesn't move, speak, blink or otherwise react. No normal breathing – The person isn't breathing or is only gasping for air.
What are the 3 shockable rhythms?
Shockable Rhythms: Ventricular Tachycardia, Ventricular Fibrillation, Supraventricular Tachycardia.
What is PEA ECG?
Pulseless electrical activity (PEA) refers to cardiac arrest in which the electrocardiogram shows a heart rhythm that should produce a pulse, but does not.
What are the 3 lethal heart rhythms?
You will need to be able to recognize the four lethal rhythms. Asystole, Ventricle Tachycardia (VT), Ventricle Fibrillation (VF), and Polymorphic Ventricle Tachycardia (Torsade de pointes).
What is sudden cardiac arrest?
As defined by the American Heart Association and the American College of Cardiology, "(sudden) cardiac arrest is the sudden cessation of cardiac activity so that the victim becomes unresponsive, with no normal breathing and no signs of circulation. If corrective measures are not taken rapidly, this condition progresses to sudden death. Cardiac arrest should be used to signify an event as described above, that is reversed, usually by CPR and/or defibrillation or cardioversion, or cardiac pacing. Sudden cardiac death should not be used to describe events that are not fatal."[1] Each year more than 400,000 Americans succumb to sudden cardiac death.[2] Those suffering from cardiac arrest may or may not have previously diagnosed with heart disease. The cause of cardiac arrest varies by population and age, most commonly occurring in those with a previous diagnosis of heart disease. Most of all cardiac deaths are sudden and usually unexpected, which has proven to be uniformly fatal in the past. However, bystander cardiopulmonary resuscitation (CPR) and advances within emergency medical services (EMS) have proven life-saving interventions. Despite this, approximately 10% of those suffering from cardiac arrest leave the hospital alive, most of which are neurologically impaired.[3]
What are the steps of reverse cardiac arrest?
The interventions that have proven to reverse cardiac arrest include early CPR and early defibrillation. The initial step involves identification and basic life-support measures. If public access defibrillation is available, it should be activated and utilized if needed. Next, advanced life support measures are used, including intravenous or intraosseous medication administration. If return of spontaneous circulation (ROSC) is obtained, the patient will undergo post-resuscitation care with subsequent long-term management.
What is the identification of a cardiac arrest victim?
Identification of a cardiac arrest victim includes assuring a patient is unresponsive, without central pulses and not breathing normally. Once a victim is identified, immediate CPR and activation of the emergency response system should be of priority. More recently, public access defibrillation has added another layer of response.
What is BLS treatment?
Providers can use BLS treatment with the addition of medications and advanced airways, including supraglottic airway devices (King LT, Igel) and endotracheal intubation. Medications used in the cardiac arrest include Epinephrine and Amiodarone. Advanced life support (ALS) providers have the additional benefit of cardiac rhythm interpretation, allowing for quicker defibrillation if indicated. Advanced Cardiac Life Support (ACLS) can teach providers the algorithms used to resuscitate a patient in cardiac arrest.
What is the difference between blunt and penetrating trauma?
Patients usually succumb to their injuries immediately after the event takes place. Most blunt trauma arrest patients are deemed to be futile upon arrival of first responders. Victims of penetrating trauma are more like to survive when compared to blunt traumatic arrests.[14] Penetrating trauma patients are typically treated with bilateral needle decompressions. If ROSC is not obtained and if within a non-futile time frame, patients can undergo a resuscitative thoracotomy. This will allow for direct visualization and, if needed, an intervention of the heart, lungs and large vessels.[14] Another technique that is still under evaluation is resuscitative endovascular balloon occlusion of the aorta (REBOA).[15] This involves the placement of an endovascular balloon within the aorta to control hemorrhage, similar to cross-clamping the aorta, which is a manual technique to control hemorrhage during a resuscitative thoracotomy.
What is the difference between cardiac arrest and syncope?
Syncope is a temporary loss of consciousness that is usually caused by decreased blood flow to the brain. Patients who experience syncope are transiently unresponsive as are all individuals experiencing cardiac arrest. However, patients who are in cardiac arrest will not have a normal breathing pattern or a pulse, differentiating syncope from cardiac arrest. A seizure can also be mistaken for cardiac arrest. Patients having a seizure will be unresponsive and will probably have abnormal respirations. Abnormal rhythmic activity and a presence of a pulse differentiate seizure from cardiac arrest. Overdose, particularly from opiates, can lead to a patient who is unresponsive and not breathing normally. The presence of a pulse will differentiate opiate overdose from cardiac arrest.
What is the leading cause of sudden cardiac death?
Occlusive (ischemic) coronary disease is the leading cause of cardiac arrest and sudden cardiac death.[4] An initial peak of sudden death occurs from birth to 6 months of age, from sudden infant death syndrome. Incidence is typically very low until reaching a second peak between ages 45 to 75. Interestingly, the most common cause of cardiac death seen in adolescent and young adults mirrors that of middle-aged and older adults.[5] Within the United States, up to 70% of all sudden cardiac death is due to underlying coronary heart disease. [2]
What does sudden cardiac arrest mean?
Sudden Cardiac Arrest means your heart has stopped pumping blood. Sudden Cardiac Arrest is caused by an electrical problem in the heart
How long does it take to defibrillate a cardiac arrest?
Defibrillation within 6 minutes is critical to survive Sudden Cardiac Arrest; however, the average response time to an emergency call is 6 to 12 minutes. Only 5% of people will survive a Sudden Cardiac Arrest.
What does EF mean in heart?
A heart that pumps poorly, as measured by a low ejection fraction (EF)
Is sudden cardiac arrest the same as heart attack?
Sudden Cardiac Arrest and heart attack are not the same thing:
Can a clogged artery cause sudden cardiac arrest?
Even if you had a clogged artery fixed with angioplasty, bypass surgery or other procedure, you can still be at risk for Sudden Cardiac Arrest
About Cardiac Arrest
Cardiac arrest is the abrupt loss of heart function in a person who may or may not have been diagnosed with heart disease. It can come on suddenly or in the wake of other symptoms. Cardiac arrest is often fatal if appropriate steps aren’t taken immediately.
Support That Empowers
Recovery becomes so much more manageable when you have the right kind of emotional support. Our online community of survivors and caregivers is here to keep you going no matter the obstacles. We’ve been there, and we won’t let you go it alone.
Hands-Only CPR
Hands-Only CPR can be as effective as CPR with breaths. Learn how to save a life in 60 seconds.
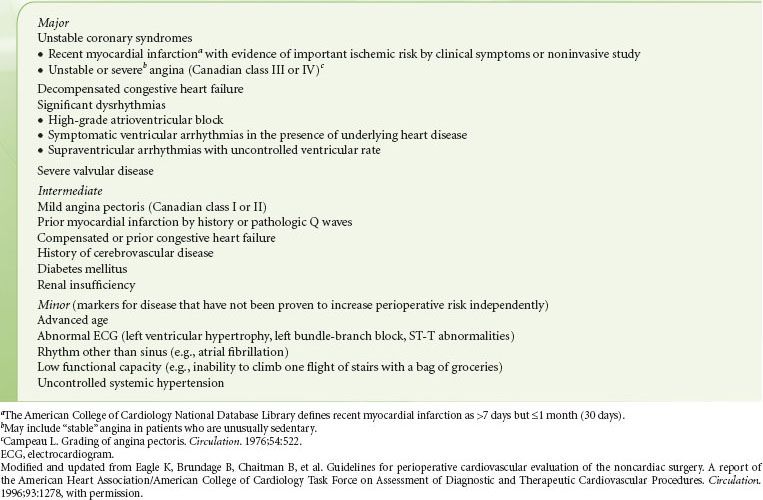
What are the three cardiac risk markers?
A thorough exam, along with non-invasive testing can provide information on three cardiac risk markers: LV dysfunction, myocardial ischemia, and heart valve abnormalities, all of which, are significant determinants of adverse postoperative outcome. [3]
When evaluating a hypertensive patient in the preoperative setting, it is imperative to assess not only the?
When evaluating a hypertensive patient in the preoperative setting, it is imperative to assess not only the patient’s current blood pressure but their baseline pressure before surgery. This can be accomplished by obtaining a thorough history as well as looking through medical records for information on their anti-hypertensive regimen as well as the adequacy of blood pressure control. The assessment should also search for evidence of chronic or acute end-organ damage. [3]
How many patients undergo non-cardiac surgery?
Many patients undergoing major noncardiac as well as vascular surgery are at risk for a major adverse cardiac event (MACE). In the United States, 27 million patients undergo non-cardiac surgery annually, 50,000 of which suffer a postoperative myocardial infarction (MI). It's estimated that cardiovascular complications are responsible for roughly one-half of all the mortality experienced by patients undergoing noncardiac surgery and occur in 1% to 5% of patients undergoing vascular surgery.[1] To minimize perioperative complications and reduce morbidity and mortality, a thorough preoperative evaluation of patients with heart disease with appropriate risk stratification is necessary.[2] The American College of Cardiology (ACC) and the American Heart Association (AHH) have collaborated to develop a set of clinical practice guidelines using scientific evidence to standardize the preoperative cardiac evaluation of patients undergoing non-cardiac surgery. Recommendations have their basis on a known history of or risk factors for cardiac disease, the patient’s functional status, as well as the urgency of the procedure. The resulting individualized cardiac risk assessment reduces the risk of MACE, as it determines the need for further optimization of the patient with diagnostic testing, medical therapy, and even coronary interventions. [3]
How many people have heart failure in the US?
The prevalence of heart failure (HF) in the United States is currently 5.7 million and continues to increase. Heart failure is an important predictor of a major adverse cardiac event and has a higher 30-day postoperative mortality rate (9.2 to 9.3%) when compared to those with CAD (2.9%).[7] The risk elevates when HF is decompensated or is worsening. Perioperative mortality increases to 13% when patients have an exacerbation of HF within 4 weeks of intended surgery. Using the New York Heart Association (NYHA) categories to assess the severity of heart failure can be useful in determining if a patient requires an echocardiogram (Class III and IV) preoperatively to assess left ventricular function, or further evaluation by a cardiologist. Optimization of fluid status and improvement of symptoms prior to surgery can improve outcomes. [6]
How long should you postpone a balloon angioplasty?
To maximize DAPT, the 2016 ACC/AHA guidelines recommend patients treated with balloon angioplasty, a bare metal stent, or a drug-eluting stent, should postpone elective noncardiac surgery for 14 days, 30 days and 3 - 12 months , respectively. [9][7]
What is physical examination?
The physical examination focuses on the cardiovascular and pulmonary systems and includes auscultation of the heart and lungs, inspection of arterial pulses and veins, abdominal palpation and examination of the extremities for edema and vascular integrity.
Can asymptomatic patients undergo invasive hemodynamic monitoring?
Asymptomatic patients can proceed with low to intermediate risk surgery, and invasive hemodynamic monitoring is a consideration. If the surgery is high risk, the patient should undergo evaluation for the possibility of an aortic valve replacement (AVR), or if ineligible for AVR, can proceed with invasive hemodynamic monitoring. [3]
How many cardiac arrests are there in the US each year?
There are an estimated 435,000 out-of-hospital cardiac arrests each year, according to the American Heart Association’s Heart Disease and Stroke update 2014. Thus it is important to review adult and pediatric advanced cardiac life support algorithms, which have changed as of the American Heart Association’s 2015 update. The most recent guidelines are not a significant change from those released in 2010 in relation to basic life support (BLS) and the use of automated external defibrillators (AED); however, key changes are important to note, including employment of a “pit crew” approach, quality of chest compressions, use of mechanical compression devices, changes to medications utilized, and implementation of therapeutic hypothermia in return of spontaneous circulation (ROSC).
What are the determinants of outcome follow- ing cardiac arrest?
For in- stance, the 2 most important determinants of outcome follow- ing cardiac arrest are early defibrillation and quality of CPR. 1 By- stander-initiated CPR, as well as a shock delivered in <5 minutes, have been shown to significantly improve a patient’s survival following cardiac arrest .1,2 Yet, historical information can play a huge role in patient outcomes: 1
How many breaths per minute for advanced airway?
It is also important to avoid hyperventilation as this can lead to reduced cardiac output1. No advanced airway: 30:2 (adult) or 15:2 (pediatric) compression-to-ventilation ratio. Advanced airway: continuous compressions and 1 breath every 6 seconds (10 breaths/minute)
Is cardiac arrest in the field similar to a cardiac arrest in the hospital?
A cardiac arrest in the field should be organized similar to a cardiac arrest in the hospital (number of personnel may vary by system):
What are the sounds of the heart when you are auscultating?
There are different heart sounds you may hear when auscultating. Normal heart sounds include hearing S1 and S2 or “lub dub.” S1 is when the AV valves close and systole begins with contraction of the ventricles. S2 represents the closing of the semilunar valves (aortic valve and pulmonary valve).
What are the extra heart sounds?
There are extra heart sounds you may hear such as S3 and S4. S3 is usually heard after the S2. S4 is heard right before S1. You may also hear murmurs which I describe as a “whooshing sound.” When it comes to auscultation and interpreting different heart sounds, you must watch visuals and practice as well.
What does it mean when a patient is restless?
If your patient appears restless or drowsy, it may be a sign of hypoxia.
How to check for capillary refill?
When checking for capillary refill, pressure is placed on the fingernail or toenail until it becomes pale. Once it becomes pale, the pressure is removed, and you look for when the nailbed becomes pink again. Normal capillary refill should be 2-3 seconds.