Bedside Report’s Effects on Patient Satisfaction - NardyTom
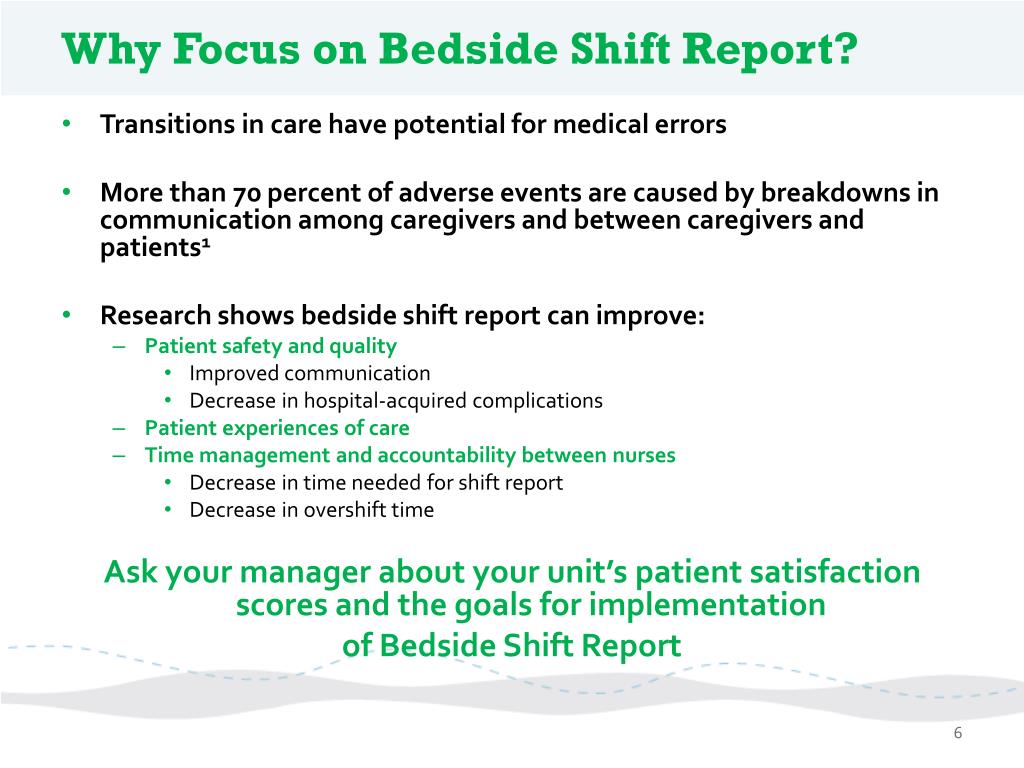
17 hours ago · The collected evidence indicates that bedside report is critical for increasing the satisfaction of patients, improving communication between nurses, and avoiding potential medication errors. This project can be effectively implemented, if the hospital is not understaffed. >> Go To The Portal
Bedside shift reporting process improves patient safety and satisfaction. “The results in terms of patient satisfaction were almost immediate. Scores have reached the highest level in the department’s history, mirroring experiences of other ED bedside report models across the country,” Pearce says.
Full Answer
Why is bedside reporting important?
- “…improves time, and overall patient safety”
- “… we were able to address a neuro status that had changed from report to the bedside”
- “I like it and we may want to expand and do NIH at bedside at BSR”
- “…it is nice to have eyes on all my patients and we can check orders are done.”
Does bedside report reduce falls?
Bedside shift reports are viewed as an opportunity to reduce errors and important to ensure communication between nurses and communication. Models of bedside report incorporating the patient into the triad have been shown to increase patient engagement and enhance caregiver support and education.
Why is bedside shift report?
Shift report, when completed at the patient bedside, allows the nurse to visualize and assess the patient and the environment, as well as communicate with and involve the patient in the plan of care. Bedside shift report (BSR) enables accurate and timely communication between nurses, includes the patient in care, and is paramount to the delivery of safe, high quality care.
How are hospitals improving patient satisfaction?
Implement These Solutions
- Meet Expectations. Understand what patients expect of their visit; some patients are looking for information, while others need assurance or a specific action.
- Devote Quality Time. Patient satisfaction rates are directly related to the length of one-on-one time physicians spend with a patient during each visit.
- Improve Appearances. ...
- Raise Perceptions. ...

What should be included in a bedside report?
Now, during a bedside report, patients may include information not previously shared, ask questions, and thank the nurses for spending the time to discuss what's going on.
How do I write a good bedside report?
Here's what they had to say:Give a Bedside Report. “Check pertinent things together such as skin, neuro, pulses, etc. ... Be Specific, Concise and Clear. “Stay on point with the 'need to know' information. ... When in Doubt, Ask for Clarification. ... Record Everything. ... Be Positive!
What is the importance of bedside report?
Bedside shift reports are viewed as an opportunity to reduce errors and important to ensure communication between nurses and communication. Models of bedside report incorporating the patient into the triad have been shown to increase patient engagement and enhance caregiver support and education.
Do patients like bedside report?
The evidence based research reviewed unanimously concludes that conducting bedside reporting leads to increased patient safety, patient satisfaction, and nurse satisfaction.
What is a bedside report?
By definition, a BSR is the change-of-shift report between the offgoing nurse and the oncoming nurse that takes place at the bedside. This makes patients a part of the process in the delivery of care.
How do you give a good report?
1:2020:45How to Give a Nursing Shift Report - YouTubeYouTubeStart of suggested clipEnd of suggested clipAnd what I do with my report should sheet. At the end of the day I always tread it so tip alwaysMoreAnd what I do with my report should sheet. At the end of the day I always tread it so tip always shred your report sheet whenever you're done giving a report you don't want to stick it in your locker.
Does bedside reporting increased patient safety?
Research concluded that conducting bedside reporting leads to increased patient safety, patient satisfaction, nurse satisfaction, prevented adverse events, and allowed nurses to visualize patients during the shift change. In addition, medication errors decreased by 80% and falls by 100%.
What is bedside report nursing?
Nurse bedside shift report, or handoff, has been defined in the literature as a process of exchanging vital patient information, responsibility, and accountability between the off-going and oncoming nurses in an effort to ensure safe continuity of care and the delivery of best clinical practices.2-6 There are different ...
How do I improve my bedside handover?
Yet a simple strategy to improve communication is to bring the report to the patient's bedside. This facilitates earlier connection between the oncoming nurse and the patient and presents an opportunity for the patient to ask questions and clarify information with both nurses.
What are the benefits of bedside handover?
A real safety benefit of bedside handover is the fact that visualising the patient may prompt nurses to recall important information that should be handed over and it may also trigger oncoming staff to ask additional questions. Further, patients have the opportunity to clarify content.
Why bedside handovers can be better for patients?
Bedside handover may improve patient participation, which may result in better experience (McMurray et al., 2011) giving the patient a feeling of accessible care and patient satisfaction (Mako et al., 2016) and patients can contribute information during the process which will improve quality of care and patient safety ...
What makes a good nurse report?
It should include the patient's medical history, current medication, allergies, pain levels and pain management plan, and discharge instructions. Providing these sorts of details about your patient in your end of shift report decreases the risk of an oncoming nurse putting the patient in danger.
Abstract
Concerns that bedside presentation (BsP) rounds could make patients uncomfortable led many residency programs to move daily rounds outside the patients’ room (OsPR). We performed a prospective quasi-experimental controlled study measuring the effect of these two approaches on patient satisfaction.
Introduction
Time dedicated to ward rounds (between 3 and 12 minutes per patient) varies according to the clinical setting [ 1 ]. In any case, these rounds constitute an important part of the healthcare team workday [ 2 ].
Methods
This is a prospective quasi-experimental controlled study conducted at a 96-bed university based general medical rehabilitation ward comprising 8 units of 12 patients each with a mean of 2.4 patients/room.
Results
Ninety consecutive patients for the pilot phase were included between May and June 2012 and 180 consecutive patients for the controlled study were included between December 2012 and March 2013. All of them gave their signed informed consent to participate in the study.
Discussion
This pragmatic study showed that when assigned to conduct rounds as usual, healthcare teams perform a vast majority of visits in the hallway and only few visits at the patient’s bedside. Yet, when requested to conduct bedside rounds, they change their usual clinical practice and the number of visits at the patient’s bedside significantly increases.
Conclusion
Bedside visits are an essential part of inpatient care that contributes to increased patient satisfaction with better family involvement, care coordination and transition of care. However, bedside visits can also be associated with worse scores on certain items such as trust in nurses and hospital recommendation.
Acknowledgments
We would like to thank each hospital ward that participated in our trial and are grateful for their confidence in our project team.
Moving Shift Report to the Bedside: An Evidence-Based Quality Improvement Project
Edward R. McAllen, Jr., DNP, MBA, BSN, BA, RN Kimberly Stephens, DNP, MSN, RN, DNP Brenda Swanson-Biearman, DNP, MPH, RN Kimberly Kerr, MSN, RN Kimberly Whiteman, DNP, MSN, RN, CCRN-K
Abstract
A Midwestern, 532-bed, acute care, tertiary, Magnet® designated teaching hospital identified concerns about fall rates and patient and nurse satisfaction scores. Research has shown that the implementation of bedside report has increased patient safety and patient and nurse satisfaction.
Background
A team of nursing administrators, directors, staff nurses, and a patient representative was assembled to review the literature and make recommendations for practice changes. A Midwestern, 532-bed, acute care, tertiary, Magnet® designated teaching hospital identified that fall rates were above the national average.
Literature Review
The team completed a literature review based upon the following PICO question: Does the implementation of BSR as compared to standard shift report at the nurses’ station increase patient safety and patient and nurse satisfaction? The practice of shift report at the bedside is not a new concept and is well documented in the literature.
Methods
The team completed a gap analysis to determine evidence-based best practices for shift report as compared to the current practice. Written approval to conduct the quality improvement project was obtained from the university and hospital institutional review boards (IRB).
Measures
Audits A BSR audit tool was implemented to assure compliance to the BSR process, including verifying that report was completed at the bedside; introducing the oncoming nurse; scripting in ISBARQ; updating the white board; and reviewing care.
Data Analysis
The software SPSS (IBM Inc., Chicago, IL, USA) version 22 was utilized to complete the data evaluation process. The analysis of patient satisfaction results was measured using independent samples t- test (two-tailed) to determine statistical significance of the data.
Why is bedside reporting important?
Communication can save lives and the evidence does demonstrate that bedside reporting is an effective communication tool to increase patient communication, patient safety, decrease med errors, and improve patient outcomes. Bed side reporting is a method of communication that each nurse should embrace and take advantage of, as it makes the nurse more accountable, responsible, and it increases the nurse and patient’s knowledge. Communication is the key to a healthy working environment.
Why is communication important in healthcare?
Communication with a patient and or family improves the overall experience and often will make a difference in where they will choice to have their health care needs in the future. Patient satisfaction is always a leading initiative for healthcare facilities in order to ensure that they are chosen over other healthcare facilities in the same region [9]. One study conducted by Kimberly Radtke [9], found patient like meeting their nurses and being involved in their plan of care. Radtke [9] writes bedside reporting “decreases the perception the healthcare team members are ‘hiding something’” and “patients feel like they are in ‘safe hands’”. One participant, a patient, from another evidence based study, stated “you want it to be right in front of you”. You want the nurses and or healthcare team to discuss and communicate in front of you, not behind doors, where the patient has no input into their own care and plan for the discharge. That gives the patient a little bit more comfort [10]. Patients want to be involved in their care plans because in times of feeling vulnerable they feel they have a say in their treatment. Taylor [5] discusses that more research should be done on patient involvement in the report process and how it affects their call light usage and anxiety levels. Patients in the 21st century are able to access their information based on their hospitalization from the internet [11]. Educated patients want a more collaborative approach in their care in order to be kept informed on their current condition and treatment plans [11].