Portal systemic encephalopathy - Cancer Therapy Advisor
8 hours ago Portal systemic encephalopathy is a neuropsychiatric disorder that occurs secondary to chronic liver disease. It is a chronic and disabling disorder that must be treated concurrently with liver disease. In chronic liver disease, the regenerative capacity … >> Go To The Portal
What is portal systemic encephalopathy?
Portal systemic encephalopathy is a neuropsychiatric disorder that occurs secondary to chronic liver disease. It is a chronic and disabling disorder that must be treated concurrently with liver disease. In chronic liver disease, the regenerative capacity …
What is encephalopathy?
Hepatic encephalopathy is suspected in non-cirrhotic cases of encephalopathy because the symptoms are accompanied by hyperammonaemia. However, the cause of the large portal-systemic shunt formation observed in these cases is not clear, as cirrhosis and portal hypertension are absent. The frequency o …
What is the pathophysiology of non-cirrhotic encephalopathy?
Hepatic encephalopathy, also referred to as portal systemic encephalopathy (PSE), is a complex neuropsychiatric disorder resulting from chronic parenchymal liver disease with liver cell failure, often in conjunction with portal systemic shunts, either naturally occurring or surgically created.
What causes hepatic encephalopathy in liver disease?
Jul 05, 2020 · Hepatic Encephalopathy (Portal-Systemic Encephalopathy) Article Details Hepatic encephalopathy is a neuropsychiatric syndrome caused by liver disease. It most often results from high gut protein or acute metabolic stress (eg, GI bleeding, infection, electrolyte abnormality) in a patient with portal-systemic shunting.

What causes portal systemic encephalopathy?
Portosystemic encephalopathy is a neuropsychiatric syndrome that can develop in patients with liver disease. It most often results from high gut protein or acute metabolic stress (eg, gastrointestinal bleeding, infection, electrolyte abnormality) in a patient with portosystemic shunting.
What happens when you have hepatic encephalopathy?
Hepatic encephalopathy is a nervous system disorder brought on by severe liver disease. When the liver doesn't work properly, toxins build up in the blood. These toxins can travel to the brain and affect brain function. People with hepatic encephalopathy may seem confused.Apr 16, 2020
What is portal systemic shunting?
Overview: A portosystemic shunt (PSS) is an abnormal connection between the portal vascular system and systemic circulation. Blood from the abdominal organs which should be drained by the portal vein into the liver is instead shunted to the systemic circulation by the PSS.
What is the management for hepatic encephalopathy?
Liver transplantation is the definitive treatment for patients with acute liver failure and hepatic encephalopathy. In patients with chronic hepatic encephalopathy, lactulose and rifaxamin remain a mainstay of therapy.
What triggers hepatic encephalopathy?
An episode of hepatic encephalopathy is often triggered by certain conditions such as infection, gastrointestinal bleeding, constipation, certain drugs, surgery or an alcohol binge. Episodes of hepatic encephalopathy can develop rapidly and without warning, often necessitating hospitalization.
What are the four stages of hepatic encephalopathy?
The most commonly used staging scale of Hepatic Encephalopathy is called the West Haven Grading System:Grade 0: Minimal HE. ... Grade 1: Mild HE. ... Grade 2: Moderate HE. ... Grade 3: Severe HE. ... Grade 4: Coma.Mar 9, 2020
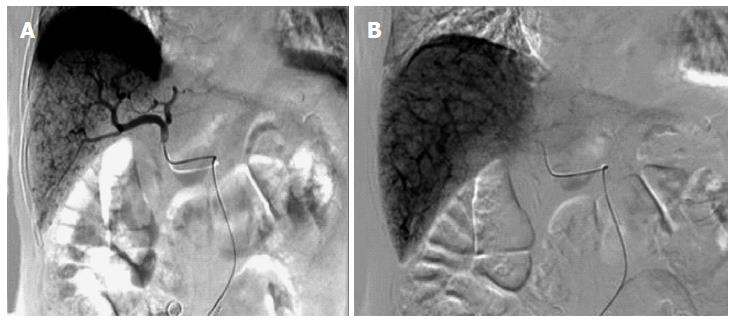
What is TIP procedure?
Transjugular intrahepatic portosystemic shunt (TIPS) is a procedure that involves inserting a stent (tube) to connect the portal veins to adjacent blood vessels that have lower pressure. This relieves the pressure of blood flowing through the diseased liver and can help stop bleeding and fluid back up.
What are portal systems?
Portal system is a system of blood vessels that begins and ends in capillaries. Hepatic portal carries nutrients from digestion to the liver to store and metabolize, after a meal.Mar 7, 2016
Why would someone need a liver shunt?
A portacaval shunt is a major surgical procedure that's used to create a new connection between blood vessels in your liver. Your doctor will recommend this procedure if you have severe liver problems.
What are encephalopathy and management for patients with encephalopathy?
Most patients can be effectively managed by treatment with lactulose and rifaximin and good education. Liver transplantation should be considered for those who have recurrent hepatic encephalopathy and/or significant liver synthetic dysfunction, as this intervention is curative.Dec 13, 2019
Which combination of therapy is most effective in controlling signs of hepatic encephalopathy?
Combined Intravenous Sodium Phenylbutyrate and Benzoate (Ammonul, Ucyclyd Pharma) In urea-cycle disorders, combination therapy results in a 79% reduction in plasma ammonia, and 84–98% improved survival with late onset disease, though poor in neonates and high peak ammonia values [37].Jun 8, 2011
How do you assess a patient with hepatic encephalopathy?
Diagnosis of minimal hepatic encephalopathy PHES is composed of five tests: number connection test-A, number connection test-B, serial dotting test, line tracing test, and digit symbol test. An alternative is using these neuropsychological tests individually.Jul 15, 2016
ESSENTIALS OF DIAGNOSIS
Diagnosis can often be made during physical examination by checking for fetor hepaticus and asterixis, and evaluating mental status using serial 7’s and the “A” deletion test.
GENERAL CONSIDERATIONS
Hepatic encephalopathy, also referred to as portal systemic encephalopathy (PSE), is a complex neuropsychiatric disorder resulting from chronic parenchymal liver disease with liver cell failure, often in conjunction with portal systemic shunts, either naturally occurring or surgically created.
PATHOGENESIS
Table 45–1 summarizes putative toxins that have been implicated in the pathogenesis of hepatic encephalopathy. Although the precise pathogenesis of hepatic encephalopathy is unknown, accumulation of nitrogenous products derived from the gut can have adverse effects on brain function and is believed to play a major role.
Classification of hepatic encephalopathy
Two broad categories of hepatic encephalopathy are#N#-Covert (Covert hepatic encephalopathy) and#N#-Overt (Overt hepatic encephalopath y
Causes
Portal-systemic encephalopathy may occur in fulminant hepatitis caused by viruses, drugs, or toxins.
Signs and symptoms
The degree of encephalopathy can be graded from 1 to 4, depending on these features, and this is useful in assessing response to therapy
Clinical Examination findings
The examination usually shows a flapping tremor (asterixis), inability to perform simple mental arithmetic tasks or to draw objects such as a star (constructional apraxia; and, as the condition progresses, hyper-reflexia and bilateral extensor plantar responses.
Pathophysiology of hepatic encephalopathy
Hepatic encephalopathy is thought to be due to a disturbance of brain function provoked by circulating neurotoxins that are normally metabolized by the liver.
Precipitating Factors for hepatic encephalopathy
In patients with chronic liver disease, acute episodes of encephalopathy are usually precipitated by reversible causes.
Treatment
The principles are to treat or remove precipitating causes and to suppress the production of neurotoxins by bacteria in the bowel.
What is the diagnosis of encephalopathy?
Diagnosis and Treatment . What to Expect . "Encephalopathy" means damage or disease that affects the brain. It happens when there’s been a change in the way your brainworks or a change in your body that affects your brain. Those changes lead to an altered mental state, leaving you confused and not acting like you usually do.
What is nonconvulsive status epilepticus?
Nonconvulsive status epilepticus. This happens when you have seizuresover and over in your brain, though they may not cause any physical symptoms. Types of encephalopathy that are irreversible include: Chronic traumatic encephalopathy. This condition is caused by repeated head injuries, which damage the brain.
What is the cause of Hashimoto's disease?
Hashimoto’s encephalopathy. This type is linked to a thyroidcondition called Hashimoto’s disease. The cause isn’t clear, but it may be that your immune systemattacks your brain and changes the way it works. Metabolic encephalopathy.
What happens when blood sugar is too high?
For example, if blood sugargets too high in diabetes, it can lead to confusion and even a coma.
What is the condition that causes brain damage?
Chronic traumatic encephalopathy. This condition is caused by repeated head injuries, which damage the brain. Today, it’s best known for its ties to high-impact sports like football and boxing. Hypoxic-ischemic encephalopathy. It happens when your brain doesn’t get enough oxygen, which leads to brain damage.
What happens if you don't get enough oxygen?
It happens when your brain doesn’t get enough oxygen, which leads to brain damage. It can happen after cardiac arrest, carbon monoxide poisoning, drug overdose, or near-drowning. Symptoms. The symptoms you have depend on the type and cause of your encephalopathy, but some of the most common ones are: Confusion.
What to do if you have seizures?
Seizures. If you notice any of these symptoms in yourself or someone else, you should call your doctor or go to the emergency room. Diagnosis and Treatment. To diagnose the disorder, your doctor will give you a physical examand ask you about your medical history, especially any medications you’re taking.
How Can I Confirm The Diagnosis?
- The diagnosis of HE is usually a clinical one. Knowledge of the presence of chronic liver disease is helpful. HE is thought to occur in the setting of advanced liver disease and portal hypertension because gut-derived toxins (including ammonia) either are not metabolized by the injured liver o…
What Is The Right Therapy For The Patient with Hepatic Encephalopathy?
- Therapy of overt HE has two important components: (1) treatment of the acute event and (2) prevention of recurrence. Once a diagnosis of overt HE is confirmed, precipitating factors must be identified and treated. Patients on diuretics with hypovolemia may require gentle intravenous hydration despite the presence of fluid overload (edema and ascites). Electrolyte abnormalities …
What Is The Most Effective Initial Therapy?
- 1. Exclude other medical conditions that may mimic HE. 2. Identify and correct precipitating factors. 3. Aggressive medical therapy – Lactulose 30 cc (2 tablespoons) every hour until there is a bowel movement and/or clinical improvement. Then begin 30 cc (2 tablespoons) twice daily, with dose adjustments to maintain 3 to 4 watery bowel movements daily. Enemas (300 cc lactul…
Listing of these, Including Any Guidelines For Monitoring Side Effects.
- Neomycin if rifaximin cannot be obtained.
- Zinc sulfate if HE continues to recur despite aggressive medical therapy.
How Should I Monitor The Patient with Hepatic Encephalopathy?
- Patients with acute HE must be monitored closely until symptoms have resolved. If patients are somnolent or comatose, they may require mechanical ventilation to protect the airway. Patients who are less compromised may be hospitalized in the general inpatient unit. Once patients return to baseline mentation, they should be monitored with frequent outpatient assessments. Patient…
What's The Evidence?
- Ferenci, P, Lockwood, A, Mullen, K. “Hepatic encephalopathy–definition, nomenclature, diagnosis, and quantification: final report of the working party at the 11th World Congress of Gastroenterology, Vienna, 1998”. Hepatology. vol. 35. 1998. pp. 716-21. (Excellent review of HE.) Bass, NM, Mullen, KD, Sanyal, A. “Rifaximin treatment in hepatic encephalopathy”. N Engl J Med. …