How To Report Errors In Patient Care? - excel-medical.com
12 hours ago · What Is The Process For Reporting Errors In Patient Care? You should inform the patient and family, then. Be sure to notify your care team, too… Hospital safety committees must be notified about this error by consulting documentation. >> Go To The Portal
How do I report a medical error?
All medical errors should be reported to a state's medical complaint board. The process of filing a report and the subsequent proceedings vary significantly by state. In general, the patient will fill out a form identifying all of the relevant parties and describing the mistake that occurred, as well as any harm that resulted from it.
Does reporting errors improve the quality of care?
Most respondents agreed that reporting errors improves the quality of care for future patients (84.3%) and would likely report a hypothetical error resulting in minor (73%) or major (92%) harm to a patient.
How common are medical errors in hospitals?
However, only 17.8% of respondents had reported an actual minor error (resulting in prolonged treatment or discomfort), and only 3.8% had reported an actual major error (resulting in disability or death). Moreover, 16.9% acknowledged not reporting an actual minor error, and 3.8% acknowledged not reporting an actual major error.
What is the medication errors reporting policy in a hospital?
A member of nursing staff. The committee reinforced medication errors reporting policy in the hospital internal wards, after approval of the hospital administrative authorities. The medication errors’ report includeed all errors related to medication (appendix). Voluntary reports from physicians and nurses were collected on standardized forms.
What do you do if you make an error in patient care?
Five Ways to Respond to a Medical MistakeAcknowledge your mistake to the patient or family. ... Discuss the situation with a trusted colleague. ... Seek professional advice. ... Review your successes and accomplishments in medicine. ... Don't forget basic self-care.
Should medical errors be reported to patients?
Large physician organizations, such as the American Medical Association in their general Code of Medical Ethics,15 state that physicians need to inform patients about medical errors so that patients can understand the error and participate in informed decision making about subsequent management of their health care.
Who is responsible for most of medication errors?
In hospital settings, nurses are most at risk for medication negligence as they are ultimately the one responsible for administration. Lack of attention can cause them to mix up medications between patients or cause them to give the wrong dosage.
Who can be a reporter of a patient safety event?
Doctors, nurses and others involved in medical and healthcare settings through prior arrangement with their organization and NASA may submit reports to the PSRS when they are involved in, or observe, an incident or situation in which patient safety may have been compromised. All submissions are voluntary.
Should you report a colleague who makes a medical error?
Here's how. Doctors who observe a colleague's medical mistake have a moral responsibility to disclose it and ensure that it is communicated to the affected patient, according to new guidelines published in NEJM this week.
What is true regarding reporting errors in patient care?
What is true regarding reporting errors in patient care? Errors in patient care need to be immediately reported to the provider. An incident report must be completed. Some states have medical error reporting systems in place.
Are nurses responsible for medication errors?
Nurses have always played a major role in preventing medication errors. Research has shown that nurses are responsible for intercepting between 50% and 80% of potential medication errors before they reach the patient in the prescription, transcription and dispensing stages of the process.
Who are the persons play a critical role in preventing and reporting medication errors?
Pharmacists can have an important role in intercepting and preventing prescribing/ordering errors. One study found that while dispensing errors were 14 percent of the total ADEs, pharmacists intercepted 70 percent of all physician ordering errors.
Who is responsible for ensuring medication errors do not occur?
Clinical leaders and senior managers of a health service organisation implement systems to reduce the occurrence of medication incidents, and improve the safety and quality of medicine use.
Which healthcare worker is responsible for reviewing every incident report?
Reports are typically completed by nurses or other licensed personnel. They should then be filed by the healthcare professional who witnessed the incident or by the first staff member who was notified about it. Patient incident reports should be completed no more than 24 to 48 hours after the incident occurred.
Who can report the adverse events associated with medical devices?
Any person including medical practitioners, clinicians, biomedical/clinical engineers, hospital technology managers, pharmacists, nurses and technicians and third party can report medical device adverse events encountered in the course of their work to IPC.
Who is required to report adverse events to FDA?
FDA has determined that dietary supplement manufacturers, packers, and distributors must report serious adverse events associated with their products using either the paper MedWatch form, Form FDA 3500A or the FDA Safety Reporting Portal.
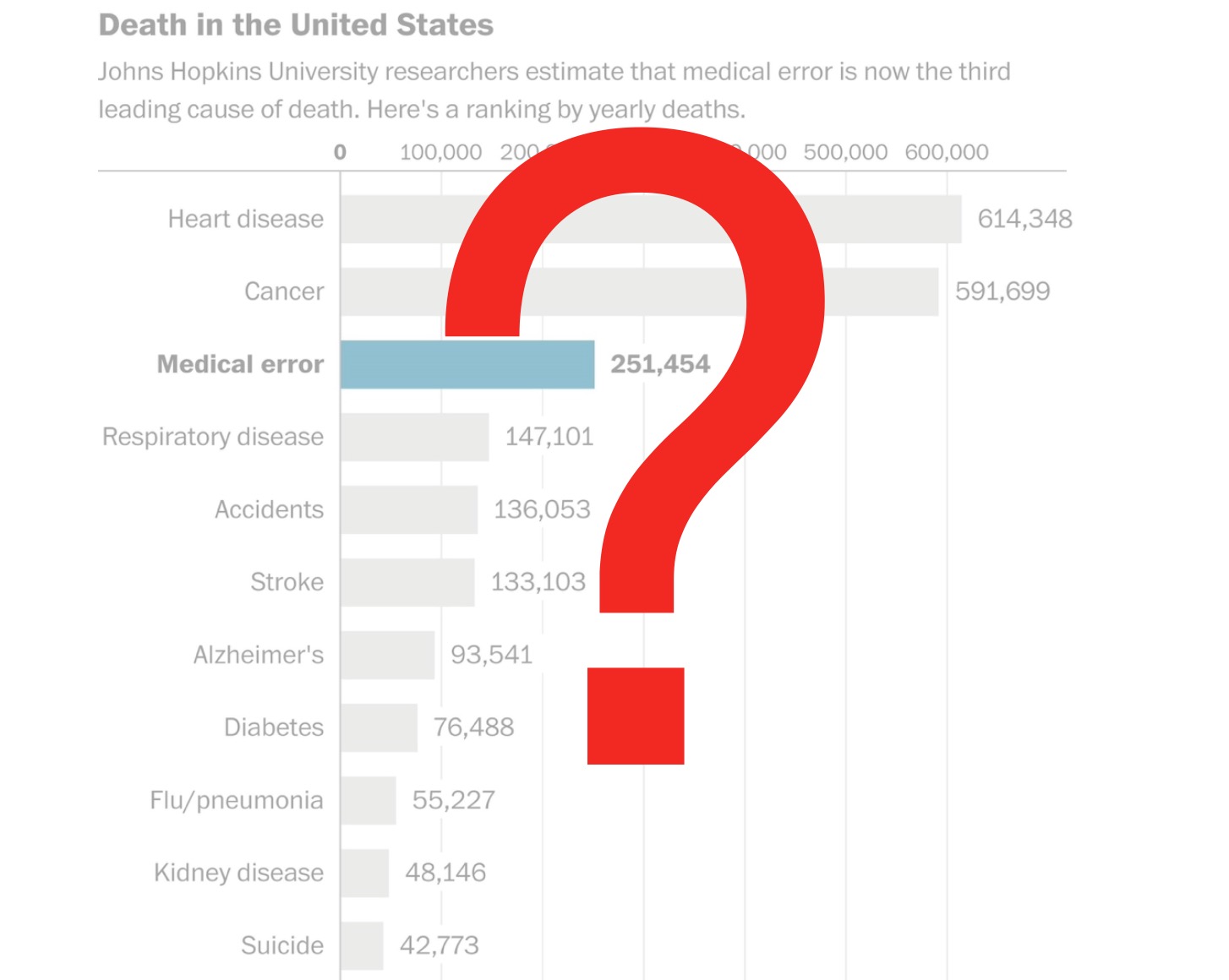
How many people die from hospital errors in 2019?
Posted by Ann Snook on July 24th, 2019. Each year in the United States, as many as 440,000 people die from hospital errors including injuries, accidents and infections. Many of those deaths could have been prevented if medical facilities used better documentation of incidents. Complete, timely patient incident reports provide valuable information ...
How long after incident should you report a patient?
Patient incident reports should be completed no more than 24 to 48 hours after the incident occurred. You may even want to file the report by the end of your shift to ensure you remember all the incident’s important details. RELATED: Near Miss Reporting: Why It’s Important.
Why is it important to review patient incidents?
Reviewing incidents helps administrators know what risk factors need to be corrected within their facilities , reducing the chance of similar incidents in the future.
Why do we use resolved patient incident reports?
Using resolved patient incident reports to train new staff helps prepare them for real situations that could occur in the facility. Similarly, current staff can review old reports to learn from their own or others’ mistakes and keep more incidents from occurring. Legal evidence.
What to include in an incident report?
Every facility has different needs, but your incident report form could include: 1 Date, time and location of the incident 2 Name and address of the facility where the incident occurred 3 Names of the patient and any other affected individuals 4 Names and roles of witnesses 5 Incident type and details, written in a chronological format 6 Details and total cost of injury and/or damage 7 Name of doctor who was notified 8 Suggestions for corrective action
How long does it take to file a patient incident report?
Patient incident reports should be completed no more than 24 to 48 hours after the incident occurred.
Why is it important to document an incident?
Even if an incident seems minor or didn’t result in any harm, it is still important to document it. Whether a patient has an allergic reaction to a medication or a visitor trips over an electrical cord, these incidents provide insight into how your facility can provide a better, safer environment.
What is a medication error?
Medication error is defined as any preventable event that may cause or lead to inappropriate medication use or patient harm while the medication is under the control of the health care professional, patient, or consumer (National Coordinating Council for Medical Reporting and Prevention, (NCCMERP), 2012)
How to improve patient safety services?
The study aims to improve patient safety services through the following objectives: 1) Determine the baseline rates of medication errors in the hospital; 2) Recognize the major types of medication error; 3) Reduce risks of medication errors through application of prevention strategies. 2. Methodology.
What is root cause analysis?
In addition, a root cause analysis (qualitative analysis) was conducted for better understanding of contributing causes and root factors. Accordingly, a corrective intervention that consisted of a targeted training program for nurses and physicians was developed and conducted during the following two months.
Why is it important to report health care errors?
It is important that problems be properly reported so that regulatory boards can reduce the likelihood of future errors by creating solutions to common treatment mishaps ...
What happens if a hospital is not performing up to the medical standard?
If your doctor or hospital is not performing up to the medical standard, you can report it to a regulatory board. If the negligence lead to an injury, you may have a legal claim. By Andrew Suszek.
What is the purpose of a medical malpractice lawsuit?
On the other hand, the purpose of a lawsuit for medical malpractice is to get compensation for harm caused by a mistake by a doctor or hospital. Such a lawsuit must be filed in court, and patients should usually consult an attorney before initiating the process.
What is the purpose of filing a medical complaint?
The purpose of filing a report with a state's medical complaint board is to provide the professional medical community with information that a doctor or hospital is not meeting the standards of the profession. But a patient might also want to notify the general public of the mistake so other potential patients can avoid the doctor or hospital.
Where can I find the medical complaint board?
The contact information for the medical complaint boards of all 50 states can be found at Consumers' Checkbook. It is important to understand that in some states, after a patient submits a report, the board may never contact the patient or sanction the doctor. This does not mean that the board ignored the report.
Can a patient sue for medical malpractice?
Once the offer is accepted, the patient will no longer be able to sue for medical malpractice over the incident, since the signing of a release of rights would be part of the deal.
Can a medical malpractice lawsuit be filed?
No. It is critical to understand that filing a report does not initiate a medical malpractice lawsuit, nor does it automatically help to establish medical negligence in any case you do eventually file. A report filed with the state board can only affect the ability of the doctor or hospital to continue practicing medicine.
How many medical errors remain unreported?
When an event results in an injury to a person or damage to property, incident reporting becomes a must. Unfortunately, for every medical error, almost 100 errors remain unreported. There are many reasons for unreported medical incidents, but not knowing when to report is one of the most common ones. Unfortunately, many patients and hospital ...
Why is reporting important in healthcare?
Reporting can also make healthcare operations more economically effective. By gathering and analyzing incident data daily, hospitals’ can keep themselves out of legal troubles. A comprehensive medical error study compared 17 Southeastern Asian countries’ medical and examined how poor reporting increases the financial burden on healthcare facilities.
What is an incident in healthcare?
An incident is an unfavourable event that affects patient or staff safety. The typical healthcare incidents are related to physical injuries, medical errors, equipment failure, administration, patient care, or others. In short, anything that endangers a patient’s or staff’s safety is called an incident in the medical system.
Why is incident reporting important?
Improving patient safety is the ultimate goal of incident reporting. From enhancing safety standards to reducing medical errors, incident reporting helps create a sustainable environment for your patients. Eventually, when your hospital offers high-quality patient care, it will build a brand of goodwill.
What is clinical risk management?
Clinical risk management, a subset of healthcare risk management, uses incident reports as essential data points. Risk management aims to ensure the hospital administrators know their institution performance and identify addressable issues that increase their exposure.
What are near miss incidents?
#2 Near Miss Incidents 1 A nurse notices the bedrail is not up when the patient is asleep and fixes it 2 A checklist call caught an incorrect medicine dispensation before administration. 3 A patient attempts to leave the facility before discharge, but the security guard stopped him and brought him back to the ward.
How much of healthcare is wasted?
Even the World Health Organisation (WHO) has estimated that 20-40% of global healthcare spending goes waste due to poor quality of care. This poor healthcare quality leads to the death of more than 138 million patients every year. Patient safety in hospitals is in danger due to human errors and unsafe procedures.
Popular Posts:
- 1. chiton medical center patient portal
- 2. who to choose for patient portal
- 3. medical providers report that over ___ of all patient visits
- 4. barnes patient portal
- 5. patient fall incident report
- 6. primary care associates wichita patient portal
- 7. springcharts patient portal
- 8. blake patient portal
- 9. the patient aging report is used to ________. quizlet
- 10. bay area cardiology patient portal