How Common Is Misdiagnosis or Missed Diagnosis?
18 hours ago Oct 18, 2021 · Errors in test results can happen because of flawed equipment or human error. In some cases, a technician who administers the test inappropriately, or a secondary doctor who misreads a scan, resulting in a doctor making an incorrect diagnosis, can be held liable. If the hospital staff makes a mistake, the hospital can be held directly liable. >> Go To The Portal
What happens if a doctor fails to diagnose a patient?
Oct 18, 2021 · Errors in test results can happen because of flawed equipment or human error. In some cases, a technician who administers the test inappropriately, or a secondary doctor who misreads a scan, resulting in a doctor making an incorrect diagnosis, can be held liable. If the hospital staff makes a mistake, the hospital can be held directly liable.
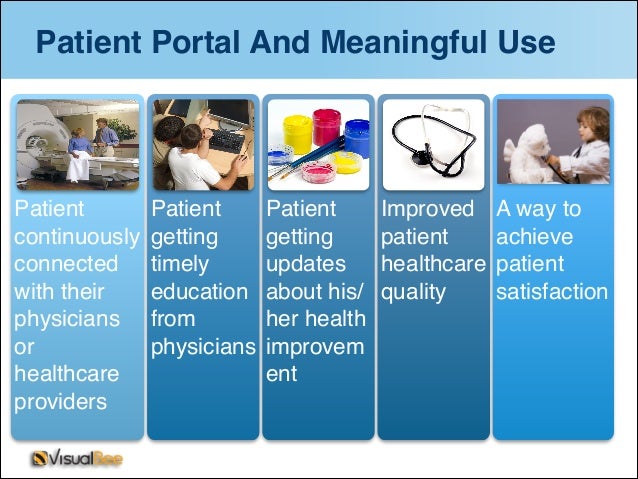
What is a patient portal?
Jun 10, 2008 · Failure to do so will result in the wrong information being copied into future medical records or an inability for your medical team to contact you if needed. Any inaccurate information about your symptoms, diagnosis, or treatment should be corrected.
Can a doctor diagnose a patient with a condition they don’t have?
Apr 01, 2022 · A patient portal is a website for your personal health care. The online tool helps you to keep track of your health care provider visits, test results, billing, prescriptions, and so on. You can also e-mail your provider questions through the portal. Many providers now offer patient portals. For access, you will need to set up an account.
When is misdiagnosis or failure to diagnose a medical condition actionable?
Instead, patients usually must prove three things in order to prevail in a medical malpractice lawsuit based on a wrong diagnosis: A doctor-patient relationship existed. The doctor was negligent -- that is, did not provide treatment in a reasonably skillful and competent manner. The doctor's negligence caused actual injury to the patient.
How do I remove a wrong diagnosis from my medical records?
If you think the information in your medical or billing record is incorrect, you can request a change, or amendment, to your record. The health care provider or health plan must respond to your request. If it created the information, it must amend inaccurate or incomplete information.
What should one do if a doctor puts inaccurate information in your records?
What do I do if something is incorrect or missing?Step 1: Contact your provider. Contact your provider's office and find out what their process is for making a change to your health record. ... Step 2: Write down what you want fixed. ... Step 3: Make a copy of your request. ... Step 4: Send your request.
Can a doctor lie about your diagnosis?
You can sue your doctor for lying, provided certain breaches of duty of care occur. A doctor's duty of care is to be truthful about your diagnosis, treatment options, and prognosis. If a doctor has lied about any of this information, it could be proof of a medical malpractice claim.Jun 26, 2019
How can an electronic medical record be corrected?
Proper Error Correction ProcedureDraw line through entry (thin pen line). Make sure that the inaccurate information is still legible.Initial and date the entry.State the reason for the error (i.e. in the margin or above the note if room).Document the correct information.
What is a valid reason for denying an amendment request?
Reasons for Denial. The provider who received the amendment request had not created the original record. The record was created at another office. There is an exception if the creator is no longer available and the mistake in the record is apparent.
What should a patient do if they discover incorrect information in their medical record quizlet?
When the physician discovers an error, such as a progress note that has been inserted into the wrong record or is missing, it must be added as an addendum or corrected in the specific manner. When making a correction on a computerized document, maintain the original entry in the electronic file.
What are the potential dangers of lying to a doctor?
Lying also has an effect on the liar (eg, feelings of guilt, entitlement, alarming powerfulness, damage to a sense of personal integrity, and loss of credibility). Within medicine, physicians are often tempted to retaliate against patients who lie by withholding treatment.
Can doctors hide information from patients?
“The therapeutic privilege permits physicians to tailor (and even withhold) information when, but only when, its disclosure would so upset a patient that he or she could not rationally engage in a conversation about therapeutic options and consequences”.
Why do doctors withhold information from patients?
The practice of withholding pertinent medical information from patients in the belief that disclosure is medically contraindicated is known as “therapeutic privilege.” It creates a conflict between the physician's obligations to promote patients' welfare and respect for their autonomy by communicating truthfully.
Who should correct an error in a patient's chart?
Make sure your staff is aware of your practice's policy regarding amendment of medical records. If a staff member finds an error, he or she should point out the error to a physician, but never correct it. Keep your medical records the minimum amount of time required by law, which varies by state.Feb 1, 2005
How do you correct documentation errors?
In BriefDon't obliterate the mistaken entry. ... Make the correction in a way that preserves the original entry. ... Identify the reason for the correction. ... Follow facility policy when adding late information. ... Never alter words or numbers after you've written them. ... Correct mistakes promptly.
What is the status of a medical record if the patient has passed away?
When a patient dies, their legal representatives, legal heirs, or close relatives have the right to access their medical records – upon written request. This allows them to know the cause of death or the specificities of their treatment.Jan 28, 2021
Where Does a Locked Diagnosis Still Appear? How Do I Send Records?
A hidden or “locked” diagnosis does not appear in the patient portal for any user, nor does it appear on reports like the Patient Visit Summary. However, it does appear in two places.
Configure Default Hidden Diagnoses
Your practice can configure any diagnosis to be hidden or “locked” by default for all patients. You can also apply the change retroactively for all historical diagnoses.
What is failure to diagnose?
Most often, failure to diagnose cases involve disputes related to the applicable standard of care and whether the doctor's failure to diagnose caused the plaintiff's injury. Whether the doctor lived up to the standard of care will likely require an expert opinion.
Why does misdiagnosis happen?
Another reason that misdiagnosis happens is a faulty lab result or test.
What is unusual illness?
Unusual illnesses or illnesses that are distinctive to a particular population are more likely to be missed. For example, a homeless person who comes to the emergency room asking for pain medication may be taken less seriously than an ordinary person who comes in wearing clean clothes and complaining of stomach pains.
Is misdiagnosis a medical malpractice?
Misdiagnosis on its own is not necessarily medical malpractice, and not all diagnostic errors give rise to a successful lawsuit. Even highly experienced and competent doctors make diagnostic errors. Instead, the misdiagnosis or failure to diagnose must result in improper medical care, delayed treatment, or no treatment, ...
Can a hospital be held liable for negligence?
Many doctors are not employees of the hospital, and in general a hospital cannot be held vicariously liable for a non-employee's negligence. However, when a patient goes to the emergency room, the hospital cannot tell the patient what a doctor's employment status is. Therefore, hospitals may be held liable for an emergency room doctor's medical ...
What is the responsibility of a medical provider?
Your Provider's Responsibility. By law, you have the right to correct errors in your medical records. The Health Insurance Portability and Accountability Act (HIPAA) ensures that your medical records are private. Another important part of this law allows you to request amendments to your medical record if you find errors. 1 .
Who is Trisha Torrey?
Trisha Torrey is a patient empowerment and advocacy consultant. She has written several books about patient advocacy and how to best navigate the healthcare system. By law, you have the right to correct errors in your medical records.
Does Verywell Health use peer reviewed sources?
Verywell Health uses only high-quality sources, including peer-reviewed studies, to support the facts within our articles. Read our editorial process to learn more about how we fact-check and keep our content accurate, reliable, and trustworthy. U.S. Department of Health & Human Services. Your medical records.
What are typographical errors?
Types of errors can include: Typographical spelling errors may or may not require correction. For example, if mesenteric is incorrectly spelled "mesentiric," you might not go through the trouble of having it corrected because there won't be any impact on your health or medical care. Errors in the spelling of your name do require correction ...
What happens if your address is incorrect?
Failure to do so will result in the wrong information being copied into future medical records or an inability for your medical team to contact you if needed.
How long does it take for a hospital to respond to a request for an extension?
The provider or facility must act on your request within 60 days but they may request an extension of up to 30 additional days if they provide a reason to you in writing.
How to access a patient portal?
With a patient portal: 1 You can access your secure personal health information and be in touch with your provider's office 24 hours a day. You do not need to wait for office hours or returned phone calls to have basic issues resolved. 2 You can access all of your personal health information from all of your providers in one place. If you have a team of providers, or see specialists regularly, they can all post results and reminders in a portal. Providers can see what other treatments and advice you are getting. This can lead to better care and better management of your medicines. 3 E-mail reminders and alerts help you to remember things like annual checkups and flu shots.
What are the benefits of a patient portal?
Expand Section. With a patient portal: You can access your secure personal health information and be in touch with your provider's office 24 hours a day . You do not need to wait for office hours or returned phone calls to have basic issues resolved. You can access all of your personal health information from all ...
How much does an e-visit cost?
For minor issues, such as a small wound or rash, you can get diagnosis and treatment options online. This saves you a trip to the provider's office. E-visits cost around $30.
How to prove a doctor is negligent?
The law does not hold doctors legally responsible for all diagnostic errors. Instead, patients usually must prove three things in order to prevail in a medical malpractice lawsuit based on a wrong diagnosis: 1 A doctor-patient relationship existed. 2 The doctor was negligent -- that is, did not provide treatment in a reasonably skillful and competent manner. 3 The doctor's negligence caused actual injury to the patient.
What is a doctor-patient relationship?
A doctor-patient relationship existed. The doctor was negligent -- that is, did not provide treatment in a reasonably skillful and competent manner. The doctor's negligence caused actual injury to the patient. Most medical malpractice cases hinge on either the second or third element (or both) -- was the doctor negligent and did ...
Is a doctor legally responsible for a diagnosis?
The law does not hold doctors legally responsible for all diagnostic errors. Instead, patients usually must prove three things in order to prevail in a medical malpractice lawsuit based on a wrong diagnosis: A doctor-patient relationship existed.
What is differential diagnosis?
Differential diagnosis is a systemic method used by doctors to identify a disease or condition in a patient. Based upon a preliminary evaluation of the patient, the doctor makes a list of diagnoses in order of probability. The physician then tests the strength of each diagnosis by making further medical observations of the patient, ...
Can a doctor diagnose a patient with a condition that the patient does not have?
In the rare case that a doctor diagnoses a patient with a condition or illness that the patient does not have, the patient may also be able to prove harm in the form of anxiety, stress, medical problems, and expenses due to unnecessary treatment. Start here to find personal injury lawyers near you.
What is medical malpractice?
In a medical malpractice case based on diagnostic error, the patient must prove that a doctor in a similar specialty, under similar circumstances, would not have misdiagnosed the patient's illness or condition. In a practical sense, this means proving one of two things: The doctor did not include the correct diagnosis on ...
Why does a doctor fail to diagnose a condition?
Sometimes a doctor fails to correctly diagnosis a condition because they relied on inaccurate results from laboratory tests, radiology films, or other types of tests. This can happen in one of two ways: The diagnostic equipment was faulty.
What is the purpose of a test?
Tests. Tests can help you identify what is causing your symptoms or rule out the most dangerous possible causes. There are a lot of moving parts and people who order tests, take samples, and analyze results. Errors during this process are a common cause of missed or delayed diagnosis. Questions to ask include: 1.
How long does it take for a syringe to feel better?
If you are told that the treatment plan or the new medicine should help you feel better in two weeks, then pay attention to how you feel in two weeks plus a few days. If you feel better, continue to follow the instructions or finish the prescription as directed. 5.
Can you use antiperspirant before a mammogram?
Some ask you to temporarily alter a personal habit. For example, before you have a mammogram, they ask you to avoid using antiperspirant. It’s such a little thing that it doesn’t seem important. But the aluminum in most antiperspirants can look like calcifications that would lead to more tests for breast cancer.
What is a biopsy of the skin?
Biopsies are tests that take a sample of tissue from your skin or your internal organs to identify possible infections, autoimmune disorders, or cancer. For example, your dermatologist may biopsy your skin to check for psoriasis or infection or skin cancer.
Does biotin interfere with blood work?
Biotin (B7), a vitamin present in most multivitamins and products for improving hair, nails, and skin, may interfere with many blood tests. It can cause false high and low scores and lead to treatment for the wrong condition or no treatment at all.
What does closing the loop mean?
Closing the loop means to complete the testing process correctly, so that everyone who needs to know what the tests show has the information to act on. Each person who handles your test samples and results has a process to follow to make certain that the information gets to the doctor and ultimately to the patient.
Can you be treated for a health condition no one knows you have?
You can’t be treated for a health condition no one knows you have. It is surprisingly common for healthcare professionals –– and the systems and organizations that are supposed to serve them –– to fail at following up on essential test results.
What does it mean when your cholesterol is high?
For example, your cholesterol count may be deemed low, normal, or high. A high cholesterol result can suggest a risk for heart disease in the future.
Can RA be diagnosed without a blood test?
Only 85 percent of RA patients ever test positive for that factor, and many patients don’t. Furthermore, some people without RA can have a positive rheumatoid factor.
What does it mean when a test is false positive?
What if the test result is wrong? That’s what happened to Sarah Boyle. A false positive means that you might get treated for a condition you don’t have. A false negative means that your medical condition will go untreated until your symptoms worsen.
What is post analytical phase?
The post-analytic phase includes communication of the results among the testing center, the medical practice, and the patient; as well as the doctor’s review and interpretation of the results. Errors can occur if your race, gender or age is different than what was used for the specific test’s reference range.

Popular Posts:
- 1. rsc bay.myhealth patient portal
- 2. total care family practice patient portal
- 3. arlington internal medicine patient portal
- 4. patient portal usage statistics 2019
- 5. patient portal dr. giallanza
- 6. umpqua health patient portal
- 7. mt airy family practice patient portal
- 8. elderly burns patient, is it needed to report as a possible abuse
- 9. healthfusion patient portal
- 10. women's care saratoga springs ny patient portal