How To Report Errors In Patient Care? - excel-medical.com
13 hours ago · It is sometimes referred to as disclosure of errors as well as reporting errors when the latter is incorrect. Health care practitioners and patients and family members are sometimes held responsible for errors caused by mistakes reported in health care records. >> Go To The Portal
Full Answer
How do I report a medical error?
All medical errors should be reported to a state's medical complaint board. The process of filing a report and the subsequent proceedings vary significantly by state. In general, the patient will fill out a form identifying all of the relevant parties and describing the mistake that occurred, as well as any harm that resulted from it.
Do you know when to report medical incidents in hospitals?
There are many reasons for unreported medical incidents, but not knowing when to report is one of the most common ones. Unfortunately, many patients and hospital employees do not have a clear idea about which incidents to report. Knowing when to report in hospitals can boost safety standards to a great extent. Let’s consider three situations: 1.
Does reporting errors improve the quality of care?
Most respondents agreed that reporting errors improves the quality of care for future patients (84.3%) and would likely report a hypothetical error resulting in minor (73%) or major (92%) harm to a patient.
What happens after a patient submits a report?
It is important to understand that in some states, after a patient submits a report, the board may never contact the patient or sanction the doctor. This does not mean that the board ignored the report. It probably means that the doctor has a relatively strong professional record and that the board viewed the mistake as an isolated incident.

Who should report medical errors?
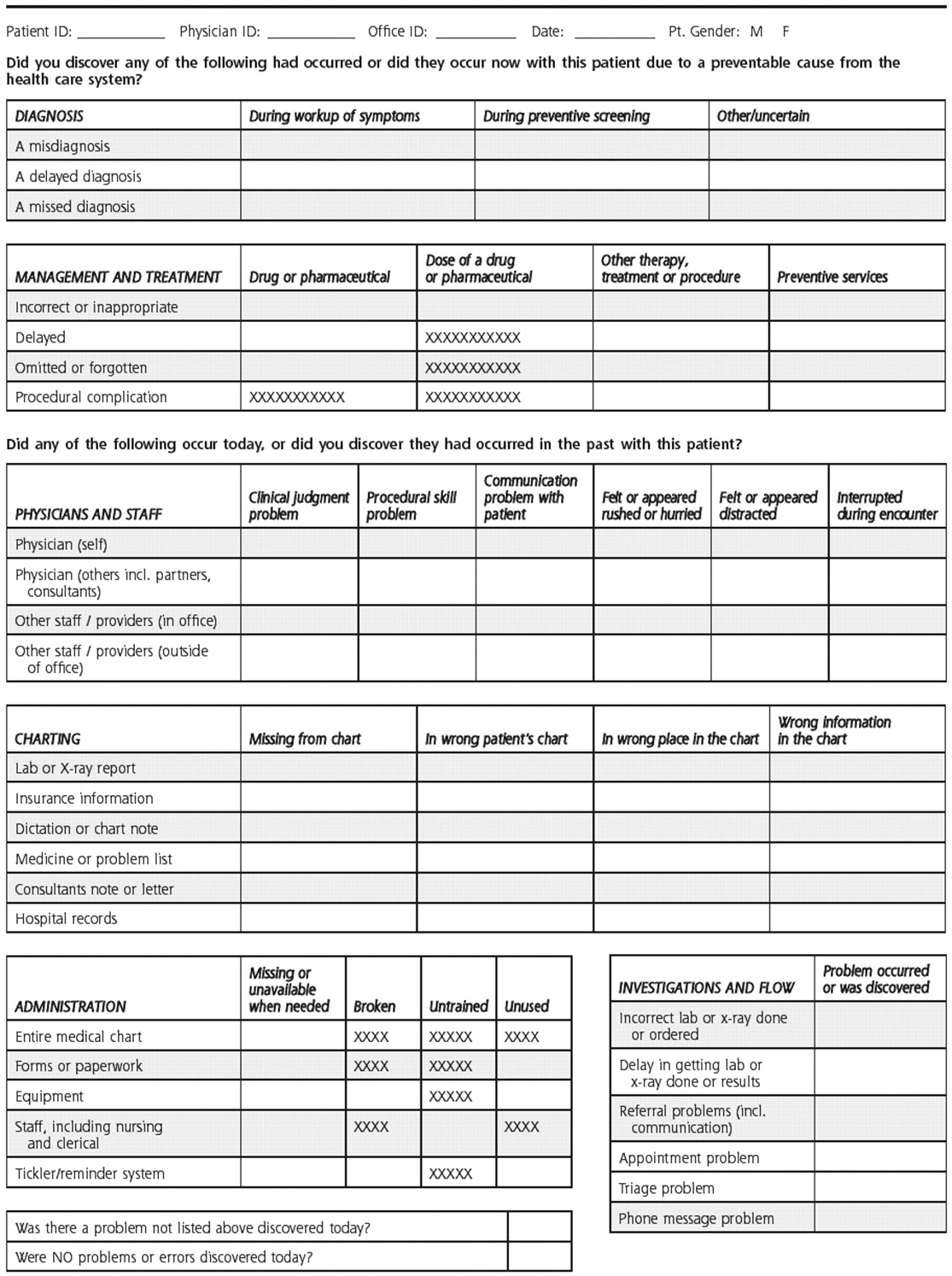
Figure 1. An error report may be transmitted internally to health care agency administrators, managers, physicians, nurses, pharmacists, laboratory technicians, other caregivers, and agency legal counsel.
What do you do if you make an error in patient care?
Five Ways to Respond to a Medical MistakeAcknowledge your mistake to the patient or family. ... Discuss the situation with a trusted colleague. ... Seek professional advice. ... Review your successes and accomplishments in medicine. ... Don't forget basic self-care.
Should medical errors be reported to patients?
Large physician organizations, such as the American Medical Association in their general Code of Medical Ethics,15 state that physicians need to inform patients about medical errors so that patients can understand the error and participate in informed decision making about subsequent management of their health care.
When should a medical error be disclosed?
Recommendations suggest that the disclosure be made soon after the mistake occurs. 36 Typically, patients do not expect a medical mistake to occur. Hence, the disclosure timing is important to consider, as are general precautions and best practices surrounding disclosure of all bad news.
Should you report a colleague who makes a medical error?
Here's how. Doctors who observe a colleague's medical mistake have a moral responsibility to disclose it and ensure that it is communicated to the affected patient, according to new guidelines published in NEJM this week.
What is true regarding reporting errors in patient care?
What is true regarding reporting errors in patient care? Errors in patient care need to be immediately reported to the provider. An incident report must be completed. Some states have medical error reporting systems in place.
How are medical errors reported?
Medication errors are detected by voluntary reporting, direct observation, and chart review. Organizations need to establish systems for prevention of medication errors through analyzing the cause of errors to identify opportunities for quality improvement and system changes (Morimoto, Seger, Hsieh, & Bates, 2004).
What actions should a nurse take following a medication error?
Taking ownership of the error and doing the right thing by putting the patient first is the only realistic course of action. Take immediate corrective measures. Inform the patient's doctor of the mistake so that action can be taken as soon as possible to counteract the effects of the incorrect medication.
How do you discuss medical errors with patients?
Disclosing medical errors the right wayBegin by stating there has been an error;Describe the course of events, using nontechnical language;State the nature of the mistake, consequences, and corrective action;Express personal regret and apologize;Elicit questions or concerns and address them; and.More items...
What happens when a nurse makes a med error?
Consequences for the nurse For a nurse who makes a medication error, consequences may include disciplinary action by the state board of nursing, job dismissal, mental anguish, and possible civil or criminal charges.
Why were pediatric specialists surveyed?
The pediatric specialists were surveyed as a comparison group to contrast with the generalist faculty physicians. When all variables were analyzed for differences, responses from pediatric specialists were not significantly different from generalist faculty responses, so their responses were included for analysis.
What is the acronym for American Board of Internal Medicine?
ABIM Foundation, American Board of Internal Medicine; ACP-ASIM Foundation, American College of Physicians/American Society of Internal Medicine; European Federation of Internal Medicine, Medical professionalism in the new millennium: a physician charter.
How long after incident should you report a patient?
Patient incident reports should be completed no more than 24 to 48 hours after the incident occurred. You may even want to file the report by the end of your shift to ensure you remember all the incident’s important details. RELATED: Near Miss Reporting: Why It’s Important.
Who completes a medical report?
Reports are typically completed by nurses or other licensed personnel. They should then be filed by the healthcare professional who witnessed the incident or by the first staff member who was notified about it.
Why is it important to review patient incidents?
Reviewing incidents helps administrators know what risk factors need to be corrected within their facilities , reducing the chance of similar incidents in the future.
Why is 62 percent of incidents not reportable?
Staff did not consider 62 per cent of incidents as reportable, due to unclear incident reporting requirements. Because of this, the first step to incident management in any healthcare facility is writing strong, clear reporting requirements. Then, staff can submit reports that help correct problems of all types.
Why do we use resolved patient incident reports?
Using resolved patient incident reports to train new staff helps prepare them for real situations that could occur in the facility. Similarly, current staff can review old reports to learn from their own or others’ mistakes and keep more incidents from occurring. Legal evidence.
What to include in an incident report?
Every facility has different needs, but your incident report form could include: 1 Date, time and location of the incident 2 Name and address of the facility where the incident occurred 3 Names of the patient and any other affected individuals 4 Names and roles of witnesses 5 Incident type and details, written in a chronological format 6 Details and total cost of injury and/or damage 7 Name of doctor who was notified 8 Suggestions for corrective action
How long does it take to file a patient incident report?
Patient incident reports should be completed no more than 24 to 48 hours after the incident occurred.
Why is it important to report health care errors?
It is important that problems be properly reported so that regulatory boards can reduce the likelihood of future errors by creating solutions to common treatment mishaps ...
Where do you report medical errors?
All medical errors should be reported to a state's medical complaint board. The process of filing a report and the subsequent proceedings vary significantly by state. In general, the patient will fill out a form identifying all of the relevant parties and describing the mistake that occurred, as well as any harm that resulted from it. The contact information for the medical complaint boards of all 50 states can be found at Consumers' Checkbook.
How Much Information Do I Need to File a Report?
So, when a patient believes that a mistake was made, a report should include as many details and as much firsthand information as possible, but medical jargon isn't necessary.
When Should I Contact an Attorney?
If a patient wishes to hire an attorney to pursue a medical malpractice action, it's best to contact an attorney as soon as possible. Upon request, the attorney will likely assist the patient in filing the report with the state medical complaint board in order to ensure that the patient does not make any statements that could be detrimental to a future lawsuit.
What is the purpose of a medical malpractice lawsuit?
On the other hand, the purpose of a lawsuit for medical malpractice is to get compensation for harm caused by a mistake by a doctor or hospital. Such a lawsuit must be filed in court, and patients should usually consult an attorney before initiating the process.
What is the purpose of filing a medical complaint?
The purpose of filing a report with a state's medical complaint board is to provide the professional medical community with information that a doctor or hospital is not meeting the standards of the profession. But a patient might also want to notify the general public of the mistake so other potential patients can avoid the doctor or hospital.
What happens if a hospital is not performing up to the medical standard?
If your doctor or hospital is not performing up to the medical standard, you can report it to a regulatory board. If the negligence lead to an injury, you may have a legal claim. By Andrew Suszek.
Who is responsible for disclosure of errors in nursing?
For minor errors, disclosure may fall to the staff nurse but for more serious ones, it will be the responsibility of the nursing supervisor, department manager or director, nursing executive, executive administration, the physician, or any combination thereof. It depends on what the problem was, who made the error, ...
Who should disclose the error?
For minor errors, disclosure may fall to the staff nurse but for more serious ones, it will be the responsibility of the nursing supervisor, department manager or director, nursing executive, executive administration, the physician, or any combination thereof. It depends on what the problem was, who made the error, and the extent of the loss or damage. A disclosure team may be formed including associated staff and management along with risk management personnel and/or the organization’s legal counsel, at least in the planning stage. Typically, the more devastating the damage, the more team members involved.
What is disclosure of adverse events?
Disclosing an adverse event is a difficult and fearful event for healthcare providers. Nonetheless, disclosure of errors is required per professional, legal and regulatory standards. For example, if a patient falls during an assisted transfer and breaks a hip, disclosure is required. If a nurse gives expressed breast milk to the wrong NICU baby, disclosure must be made to both mothers. Some events, such as “never events” defined by the Centers for Medicare & Medicaid Services, also require reporting to regulatory bodies as well as disclosing them to the patient and/or family. Never events include hospital-acquired conditions such as ventilator-associated pneumonia.
What is the key to a disclosure meeting?
Communication is key. There must be communication between all parties involved, including the doctors, associated care staff, department managers, executive management, risk management, and possibly attorneys, before the disclosure meeting. Anticipate the questions that might be asked and prepare answers.
How to answer a loved one's question?
Be understanding and empathetic with their feelings. Remember, this is their loved one. Stay calm, be receptive to their questions and answer them as honestly, yet as defensively empathetic as possible. If you’ve done your pre-planning well, you will already have a script ready for their questions.
Why is it important to keep things in perspective when an error occurs?
When an error occurs, it’s important to keep things in perspective. Human beings deliver medical services, so errors are inevitable. Be it major or minor, healthcare providers will likely make a mistake somewhere in their career, whether they know it or not. The main question is whether damage or loss occurs as a result. Because of our humanity, we must remain objective about our propensity to commit error and refrain from letting emotions carry us away. Noting mistakes and reporting them is the responsibility of all healthcare providers and fear should not prevent disclosure.
When an error occurs, is it important to keep things in perspective?
When an error occurs. When an error occurs, it’s important to keep things in perspective. Human beings deliver medical services, so errors are inevitable. Be it major or minor, healthcare providers will likely make a mistake somewhere in their career, whether they know it or not. The main question is whether damage or loss occurs as a result.
How to complain about poor care in a hospital?
How can I complain about poor medical care I received in a hospital? While you are in the hospital: If possible, first bring your complaints to your doctor and nurses. Be as specific as you can and ask how your complaint can be resolved. You can also ask to speak to a hospital social worker who can help solve problems and identify resources.
How to find out what other patients have to say about their recent hospital stays?
To find out what other patients had to say about their recent hospital stays, visit the Hospital Compare Web site. You'll find answers from patients about how well doctors and nurses communicated, how well patients' pain was controlled, and how patients rated their hospital.
What to do if you are discharged before you're ready?
If you are discharged before you're ready: This is a big concern for many patients because insurers balk at long hospital stay s. Talk to the hospital discharge planner (often a social worker) if you don't think you're medically ready to leave the hospital. The discharge planner will take your concerns to the doctor who makes this decision.
What do social workers do when patients leave the hospital?
Social workers also organize services and paperwork when patients leave the hospital. If you are covered by Medicare, you can file a complaint about your care with your State's Quality Improvement Organization (QIO) . These groups act on behalf of Medicare to address complaints about care provided to people covered by Medicare.
How long does it take to appeal a hospital discharge?
You should get a form from the hospital titled "An Important Message from Medicare," which explains how to appeal a hospital discharge decision. Appeals are free and generally resolved in 2 to 3 days. The hospital cannot discharge you until the appeal is completed.
What do you do if you get an infection in the hospital?
If you get an infection while you are in the hospital or have problems getting the right medication, you can file a complaint with the Joint Commission . This group certifies many U.S. hospitals' safety and security practices and looks into complaints about patients' rights. It does not oversee medical care or how the hospital may bill you.
Is it easy to be assertive in a health care setting?
Even with this information, it's not easy to be as assertive in a health care setting as it is in an auto repair shop or restaurant. But it's a smart move that can help you get the quality care that you deserve.
What would happen if a facility did not report you?
Depending on your response, your facility would set up a disciplinary course of action for you. That would involve either re-educating, counseling, or if you feel that it should not be reported or that you should not be held accountable, possibly termination. Everyone makes mistakes.
Is it legal to lie to patients about medication errors?
So, no. It is not legal for hospitals to lie to patients about medication errors. It is not legal for health care professionals to lie and withhold medical information from patients.
Do patients have a right to know the truth?
I'm sorry I should of said I am a nursing student. I know ethically you should tell the patient, I need to know exact legislation that says you have to legally report it to the patient.
When To Write Incident Reports in Hospitals?
When an event results in an injury to a person or damage to property, incident reporting becomes a must. Unfortunately, for every medical error, almost 100 errors remain unreported. There are many reasons for unreported medical incidents, but not knowing when to report is one of the most common ones.
Who Prepares Incident Reports in Healthcare Facilities?
At QUASR, we believe all staff (and patients, too) should be able to report incidents or potential incidents they have witnessed. But in practice, it is a bit different. Some hospitals have designated persons who are authorized to file the reports. In some other hospitals, the staff usually updates their supervisor about an incident, then can file the report.
What is an incident in healthcare?
An incident is an unfavourable event that affects patient or staff safety. The typical healthcare incidents are related to physical injuries, medical errors, equipment failure, administration, patient care, or others. In short, anything that endangers a patient’s or staff’s safety is called an incident in the medical system.
Why is incident reporting important?
Improving patient safety is the ultimate goal of incident reporting. From enhancing safety standards to reducing medical errors, incident reporting helps create a sustainable environment for your patients. Eventually, when your hospital offers high-quality patient care, it will build a brand of goodwill.
What is clinical risk management?
Clinical risk management, a subset of healthcare risk management, uses incident reports as essential data points. Risk management aims to ensure the hospital administrators know their institution performance and identify addressable issues that increase their exposure.
What are near miss incidents?
#2 Near Miss Incidents 1 A nurse notices the bedrail is not up when the patient is asleep and fixes it 2 A checklist call caught an incorrect medicine dispensation before administration. 3 A patient attempts to leave the facility before discharge, but the security guard stopped him and brought him back to the ward.
How much of healthcare is wasted?
Even the World Health Organisation (WHO) has estimated that 20-40% of global healthcare spending goes waste due to poor quality of care. This poor healthcare quality leads to the death of more than 138 million patients every year. Patient safety in hospitals is in danger due to human errors and unsafe procedures.
When did Harvard start responding to medical errors?
In 2006, Harvard’s teaching hospitals adopted a policy on responding to medical errors. About 500 of the hospitals’ senior leaders underwent training, then trained doctors and nurses at their facilities to coach peers in disclosing medical errors to patients and families and then apologizing for the mistake.
Why is it important to learn from any adverse medical incident?
It is important to learn from any adverse medical incident and improve, Mayer stresses. Making a serious medical error can be devastating for clinicians, too, and has even led to physician suicides, he says. “This isn’t a shame and blame game. These people [who have made unintentional mistakes] need hugs more than anything.”
Why do CRPs help nurses?
CRPs also aim to alleviate the guilt and shame that physicians and nurses often feel after making a medical error. Keeping mistakes quiet is a human impulse, and trainees may be especially concerned about how disclosure might affect their evaluations, Gallagher says. “Educators need to really work on ensuring that they have a nonpunitive culture so that trainees know that what is expected of them is this openness, and that their evaluations won’t suffer as a result of [reporting an error],” Gallagher says.
When did Boothman and the UMHS risk management team start?
Similar scenarios have played out multiple times since 2001, when Boothman and the UMHS risk management team pioneered a model for handling medical errors and improving patient safety that is built on openness with patients and families and includes:
Who is the vice president of quality and safety at MedStar Health?
Boothman and Da vid B. Mayer, MD, are among those whose work influenced the CANDOR Toolkit. Mayer helped to develop the CRP at the UIH years ago. Now vice president of quality and safety at MedStar Health, Mayer established a patient safety immersion camp for medical students and residents operated by MedStar’s Institute for Quality and Safety in several cities.
Is medical error a leading cause of death?
Then, a milestone 2000 Institute of Medicine report, To Err Is Human: Building a Safer Health System, called medical errors a major cause of preventable deaths and recommended that hospitals focus on improving patient safety. Today, the medical community recognizes medical errors as a leading cause of death and disability.
Does Truog say "I'm sorry"?
“In the case of an error, yes, an apology is always called for,” Truog says; if the cause is unclear, clinicians might say, “I’m sorry this has happened to you.”