How to write a patient care report - Safety Training Pros
14 hours ago · Medical records should be made public that include but not include any patient specifics, such as his medical history or treatment for a medical condition. Every doctor uses a patient care report (PCR) to record all care and pertinent patient information, making it the official document of patient health information. >> Go To The Portal
Reports are typically completed by nurses or other licensed personnel. They should then be filed by the healthcare professional who witnessed the incident or by the first staff member who was notified about it. Patient incident reports should be completed no more than 24 to 48 hours after the incident occurred.
What is a patient care report?
A patient care report is a document written by medical professionals to report about the patient’s wellbeing, care and status. This document consists of the result of the assessment and the evaluation of the patient being done by the EMTs or the EMS.
How long does it take to file a patient incident report?
Reports are typically completed by nurses or other licensed personnel. They should then be filed by the healthcare professional who witnessed the incident or by the first staff member who was notified about it. Patient incident reports should be completed no more than 24 to 48 hours after the incident occurred.
Who can write reports in healthcare?
A lot of people believe that only nurses or health care workers can write reports. Most specifically patient care reports or anything that may be related to an incident report that often happens in hospitals or in some health care facilities.
Where do regulations for documentation of client care come from?
Regulations regarding how to properly document client care come from: State Boards of Nursing The American Nurses Association Joint Commission CMS (Medicare and Medicaid) Workplace policies and procedures. A WORD ABOUT FALSE DOCUMENTATION

What is the purpose of a patient care report?
The primary purpose of the Patient Care Report (PCR) is to document all care and pertinent patient information as well as serving as a data collection tool. Article 30, section 3053 of the Public Health Law requires all certified EMS agencies to submit PCR/ePCRs to the Department.
How do you complete a patient care report?
There are seven elements (at a minimum) that we have identified as essential components to documenting a well written and complete narrative.Dispatch & Response Summary. ... Scene Summary. ... HPI/Physical Exam. ... Interventions. ... Status Change. ... Safety Summary. ... Disposition.
What should be included in a patient care report?
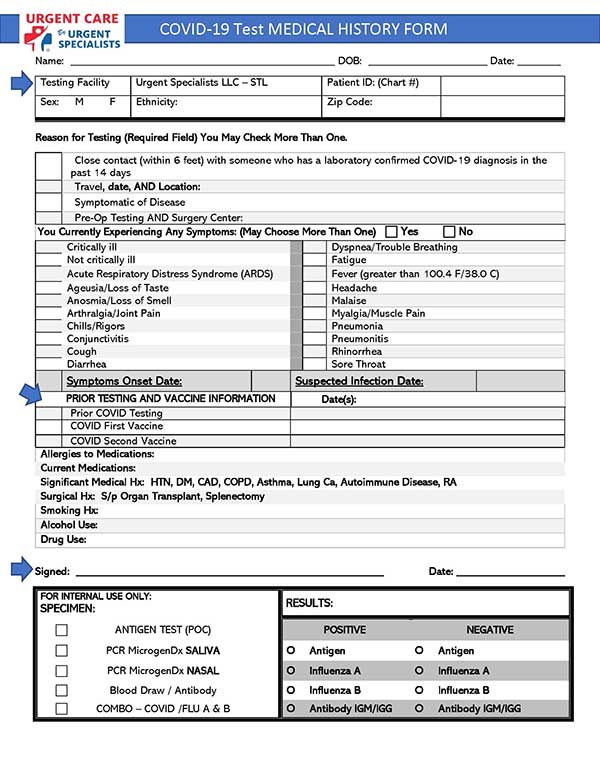
What Patient Care Reports Should IncludePresenting medical condition and narrative.Past medical history.Current medications.Clinical signs and mechanism of injury.Presumptive diagnosis and treatments administered.Patient demographics.Dates and time stamps.Signatures of EMS personnel and patient.More items...•
What is pre hospital care report?
The prehospital care report is used to record patient data. The data can include patient demographics such as name, address, date of birth, age, and gender. Dispatch data, such as the location of the call, times related to the call, rescuers and first responders on the scene may be included.
What is PCR in medical billing?
The PCR documentation is considered a medical document that becomes part of the patient's permanent medical record. It is also considered a legal document in cases where liability and/or malpractice issues arise. It is the source in which all medical billing claims are based.
What is a PCR in writing?
The PARCC Summative Assessments in Grades 3-11 will measure writing using three prose constructed response (PCR) items. In the classroom writing can take many forms, including both informal and formal.
When you document information on a patient that you treat and care for this written report is called the?
When you document information on a patient that you treat and care for. This written report is called the: Patient care report, run report. You are asked to give testimony in court about the care you gave to a patient.
What can you record on a PCR?
This includes the agency name, unit number, date, times, run or call number, crew members' names, licensure levels, and numbers. Remember -- the times that you record must match the dispatcher's times.
Why is it important for a health care provider to maintain accurate patient records?
Complete and accurate medical recordkeeping can help ensure that your patients get the right care at the right time. At the end of the day, that's what really matters. Good documentation is important to protect you the provider. Good documentation can help you avoid liability and keep out of fraud and abuse trouble.
Who assumes the ultimate responsibility for patient care?
EMT Word Knowledge IABdirectorA physician who assumes the ultimate responsibility for the patient care aspects of an EMS system is the Medical _____________.paramedicThe level of EMS training that allows relatively invasive field care such as endotracheal and initiation of IV lines48 more rows
What is EMS documentation?
First and foremost, EMS documentation serves a vital clinical purpose. It is the record of your assessment and care of patients. It becomes part of the patient's medical record, both at the receiving facility and within your EMS organization.
What is the purpose of the narrative section of the patient care report?
Detailed explanation of medical necessity: Your narrative should be detailed and provide a clear explanation for why the patient needed to be transported by ambulance. Include what the medical reasons were that prevented the patient from being transported by any other means.
How long after incident should you report a patient?
Patient incident reports should be completed no more than 24 to 48 hours after the incident occurred. You may even want to file the report by the end of your shift to ensure you remember all the incident’s important details. RELATED: Near Miss Reporting: Why It’s Important.
How long does it take to file a patient incident report?
Patient incident reports should be completed no more than 24 to 48 hours after the incident occurred.
Why is it important to review patient incidents?
Reviewing incidents helps administrators know what risk factors need to be corrected within their facilities , reducing the chance of similar incidents in the future.
Why choose a platform that is web-enabled for quick reporting?
You’ll never miss important details of a patient incident because you can file your report right at the scene. A platform with HIPAA-compliant forms built in makes your workflow more efficient and productive, ensuring patient incidents are dealt with properly.
Why do we use resolved patient incident reports?
Using resolved patient incident reports to train new staff helps prepare them for real situations that could occur in the facility. Similarly, current staff can review old reports to learn from their own or others’ mistakes and keep more incidents from occurring. Legal evidence.
What to include in an incident report?
Every facility has different needs, but your incident report form could include: 1 Date, time and location of the incident 2 Name and address of the facility where the incident occurred 3 Names of the patient and any other affected individuals 4 Names and roles of witnesses 5 Incident type and details, written in a chronological format 6 Details and total cost of injury and/or damage 7 Name of doctor who was notified 8 Suggestions for corrective action
Why is it important to document an incident?
Even if an incident seems minor or didn’t result in any harm, it is still important to document it. Whether a patient has an allergic reaction to a medication or a visitor trips over an electrical cord, these incidents provide insight into how your facility can provide a better, safer environment.
What to Include on a Patient Care Report (ePCR)
Accurate patient data is arguably the most valuable tool a medic has at his or her disposal. It not only informs immediate treatment decisions, but it shows what is – and isn’t – working. It plays a pivotal role in efficient patient hand-off at the ED, and it dictates the type of care he or she will receive in the minutes and hours after.
ePCRs: Patient Care Reports for the 21 st Century
Over the last 30 years, EMS agencies and hospitals alike have recognized the value of going digital with patient records, coining the term “electronic patient care reports” (ePCRs).
About Patient Care Reports
Digital patient care reports are slowly but surely changing the way patient information is recorded on a call, but they do not change interactions with patients. Instead of jotting down notes on a paper form, medics quickly and easily record the same information using a tablet and a digital form.
What Patient Care Reports Should Include
Just like the paper version of patient care reports, ePCRs are meant to be complete and contain all pertinent information to help deliver proper patient treatment and track performance metrics.
Obstacles to Efficiently Creating Electronic Patient Care Reports
As the adoption of ePCRs has ramped up in the last three decades, technology has evolved along with it. However, technology includes its own set of challenges. Onboarding an entire EMS agency to a new records system takes a coordinated effort and can require a substantial investment in time and money.
Comparing Documentation Methods: SOAP vs. CHART vs. IMRaD
Accurate, complete, and rich documentation in patient care reports can improve patient outcomes, provide accurate claims processing, further quality assurance, and even defend against malpractice. Offering guidance on what elements to include in narratives can result in more complete run reports.
New ePCRs Improve Patient Care While Improving Analytics and Reporting
Today’s top ePCR software tools offer direct improvement to patient care by streamlining communication and reducing the chance for human error. For example, customized forms in the system can be progressive, meaning a medic cannot move on to the next field without recording data for all required fields first.
What documentation should be included in a patient encounter?
The documentation of each patient encounter should include: Reason for the encounter and relevant patient history, physical examination findings and prior diagnostic test results; Assessment, clinical impression or diagnosis; A plan for care; and. A date and legible identity of the observer.
Why is it bad to sign a document after a couple of days?
Signatures beyond a couple of days increase the likelihood that a claim will be denied because necessary documentation will not be accepted as being present due to a signature and date too removed from the time the care was provided. This could be disastrous and costly in an audit.
How long does it take to get a signature on a chart?
Most importantly, have a policy in place that that holds you and other providers in your office to a standard time period, perhaps 36 hours, to have a signature on the chart. These two policies will help ensure there are no compliance or billing issues caused by the lack of a timely signature.
How often should you document vitals?
Patients in acute care settings tend to be quite sick. If you are ordered to document vital signs every four hours, it’s important to take the vitals—and document the results—on time.
What is the purpose of documentation?
Remember, the purpose of documentation is to communicate with other members of the health care team. (If you are the only person who can read your handwriting, your documentation won’t communicate anything to anybody!)
Do Medicare clients need to bathe?
Home health clients on Medicare must be homebound—and must need help with bathing— to receive the services of a home health aide. Your documentation should show that your client meets these requirements. However, if your client has already bathed when you arrive, document the reason and tell your supervisor right away.
What Is a Patient Care Report?
We often hear of care reports based on by medical teams or by medical authorities. Yet, we are not sure how this differs from the kind of report that is given to us by the same people. So this is the time to make it as clear as possible.
How to Write a Patient Care Report?
Where do you even begin when you write a patient care report? A lot of EMS or EMTs do know how to write one since they are trained to do so.
What is a patient care report?
A patient care report is a document made mostly by the EMS or EMTs. This documented report is done after getting the call. This consists of the information necessary for the assessment and evaluation of a patient’s care.
What should not be written in a patient care report?
What should be avoided in a patient care report is making up the information that is not true to the patient. This is why you have to be very careful and very meticulous when writing these kinds of reports. Every detail counts.
Who is in charge of reading the patient care report?
The person or the people who will be reading the report are mostly medical authorities. When you are going to be passing this kind of report, make sure that you have all the information correctly. One wrong information can cause a lot of issues and problems.
Popular Posts:
- 1. st joseph hospital eureka patient portal
- 2. childrens medical group patient portal
- 3. physicians regional medical group patient portal
- 4. trinity health minot nd patient portal
- 5. patient records to portal fee
- 6. mason city clinic patient portal server error
- 7. patient portal software cost cheapest
- 8. advanced obstetrics and gynecology patient portal
- 9. jenkins obgyn patient portal
- 10. baptist primary care portal