What to Include on a Patient Care Report (ePCR) - ESO
23 hours ago · Assessment: observations, primary impression, presumptive diagnosis; Rx (Treatment): medications and fluids administered; Transport: Information about where and how patient was transported, condition during transport, communication with receiving facility, and details of handoff at ED >> Go To The Portal
Rather, the report should include observations of the patient’s response, such as an ability to change movement patterns or posture, physical changes or adaptations during treatment, degrees of stability, etc. Here’s an example: The patient demonstrated poor upward rotation of the scapula with right shoulder flexion.
- Signs and symptoms.
- Allergies.
- Medications.
- Pertinent medical history.
- Last ins and outs.
- Events.
What information should be included in a patient assessment?
In your patient can plan, include date about the patient. Data gathered as part of the patient assessment can be categorized as either objective or subjective: Objective – Facts that are not influenced by personal feelings or interpretations. Subjective – A perception or characteristic of the patient that is based on the evaluator’s observations.
What should a patient’s a report include?
A report might detail the patient’s family background, romantic relationships and educational or developmental history, she says, but lack a section that explores other formative experiences, including those that involve race, sexuality or socioeconomic status.
What should be included in the assessment section of a report?
Seeing only this in the assessment section should make you cringe. Rather, the report should include observations of the patient’s response, such as an ability to change movement patterns or posture, physical changes or adaptations during treatment, degrees of stability, etc. Here’s an example:
How do you write a nursing assessment report?
The following are comprehensive steps to write a nursing assessment report. 1. Collect Information Assemble the information from all sources, including health assessment, discussions with the patient and their family, clinical observations, report sheet, chart notes and review, and conversations with the health care team.
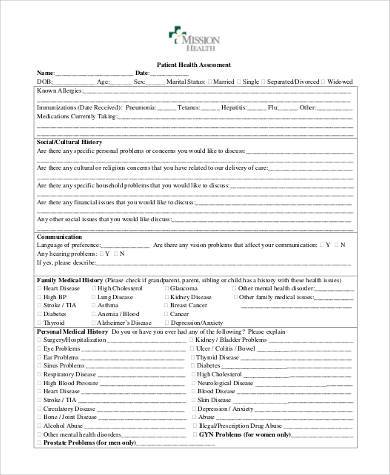
What is included in a patient assessment?
A comprehensive health assessment gives nurses insight into a patient's physical status through observation, the measurement of vital signs and self-reported symptoms. It includes a medical history, a general survey and a complete physical examination.
What are the five components of patient assessment?
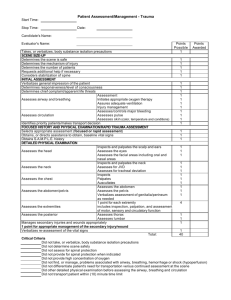
emergency call; determining scene safety, taking BSI precautions, noting the mechanism of injury or patient's nature of illness, determining the number of patients, and deciding what, if any additional resources are needed including Advanced Life Support.
How do you write a good patient assessment?
Assessment & PlanWrite an effective problem statement.Write out a detailed list of problems. From history, physical exam, vitals, labs, radiology, any studies or procedures done, microbiology write out a list of problems or impressions.Combine problems.
What is included in a nursing assessment?
An RN uses a systematic, dynamic way to collect and analyze data about a client, the first step in delivering nursing care. Assessment includes not only physiological data, but also psychological, sociocultural, spiritual, economic, and life-style factors as well.
What are the 8 general principles for patient assessment?
Overview of Picker's Eight Principles of Patient Centered CareRespect for patients' values, preferences and expressed needs. ... Coordination and integration of care. ... Information and education. ... Physical comfort. ... Emotional support and alleviation of fear and anxiety. ... Involvement of family and friends. ... Continuity and transition.More items...•
What is the first part of the patient assessment?
Patient assessment starts before you arrive at the patient's side with a scene size-up. The first step is always to assess the possible risks and take appropriate precautions. The importance of assessing scene safety cannot be overestimated.
How do you write an assessment statement?
Five tips for writing a good assessmentMake it applicable. Think of the most realistic way of assessing the learner's ability. ... There shouldn't be any surprises. ... Test knowledge of the subject matter, not reading comprehension. ... Don't go above and beyond. ... Give learners the best chance of succeeding.
How do you document an assessment?
An assessment report should accomplish the following:Outline the student learning or program outcomes or goals assessed during the assessment cycle timeframe.Identify and describe the specific assessment method(s) and tools used to gather evidence for the outcomes or goals.Identify the specific source(s) of the data.More items...
How do you write a nursing assessment summary?
The following are comprehensive steps to write a nursing assessment report.Collect Information. ... Focused assessment. ... Analyze the patient's information. ... Comment on your sources of information. ... Decide on the patient issues.
What are the 4 types of nursing assessment?
4 types of nursing assessments:Initial assessment. Also called a triage, the initial assessment's purpose is to determine the origin and nature of the problem and to use that information to prepare for the next assessment stages. ... Focused assessment. ... Time-lapsed assessment. ... Emergency assessment.
What four primary actions make up patient assessment?
WHEN YOU PERFORM a physical assessment, you'll use four techniques: inspection, palpation, percussion, and auscultation. Use them in sequence—unless you're performing an abdominal assessment. Palpation and percussion can alter bowel sounds, so you'd inspect, auscultate, percuss, then palpate an abdomen.
Subjective
The subjective section of your documentation should include how the patient is currently feeling and how they’ve been since the last review in their own words.
Objective
The objective section needs to include your objective observations, which are things you can measure, see, hear, feel or smell.
Assessment
The assessment section is where you document your thoughts on the salient issues and the diagnosis (or differential diagnosis), which will be based on the information collected in the previous two sections.
Plan
The final section is the plan, which is where you document how you are going to address or further investigate any issues raised during the review.
What to include in a patient assessment?
What to Include. In your patient can plan, include date about the patient. Data gathered as part of the patient assessment can be categorized as either objective or subjective: Objective – Facts that are not influenced by personal feelings or interpretations. Examples: laboratory results, weight, vital signs.
What are some examples of subjective information?
Examples: body condition score, pain scale rating, temperament. In addition to objective and subjective information, be sure to include the following pieces of information: ...
What are the steps of psychiatric assessment?
Questions may be related to –. Attention and focus. Orientation to time and place. Reasoning. Judgment. Memory. This may include asking questions like asking the names of the body parts, naming objects, repeat simple phrases.
What are some areas of assessment where the nurse can put in more efforts to be able to do a good assessment
There are certain areas of assessment where the nurse can put in more efforts to be able to do a good assessment like –. Checking basic physical health which involves whole-body examination. Making proper respiratory assessment. At least the rules of assessing the circulatory system of the patient.
What is the objective of assessment in nursing?
The main objective of the assessment is to determine the way of observing the progress of the patient and detecting the issues that may result in adverse events.
What is medical judgment?
Medical judgment is used to determine which assessment technique should be used and to what extent a patient needs physical examination. Primary assessment- checking the airway, breathing, etc. are components of Patient assessment. These assessments are taken for almost all patients.
How well a nurse would be able to give treatment and health care plan?
How well a nurse would be able to give treatment and health care plan is dependant on how well the assessment is made. If the assessment is made accurately, then the nurse would be able to chart an accurate and comprehensive, and problem-specific plan which will bring out better results.
What is an emergency assessment?
Emergency assessment- another type of assessment is the emergency assessment that is required when there is an emergency that requires immediate attention. It can be done by any nurse or medical practitioner who is present at that time. Emergency assessment is made only to ascertain the immediate problem at hand.
What is the basic respiratory assessment?
Also, there are assessments for different types of patients, one assessment cannot satisfy the health conditions of different patients.
What are the components of a nursing assessment?
A nursing assessment has two components, namely, a systematic collection of subjective data and objective evaluation of data. The first element deals with the information provided by the patient in response to a series of questions asked by the nurse.
Why is it important to write a nursing assessment report?
As a critical component of the nursing process, it is good to learn how to write a nursing assessment report, especially for student nurses. The evaluation is the first step in the planning and provision of patient care. It is used to identify patient care requirements and integrates the knowledge of ordinary and abnormal physiology.
What is EKG evaluation?
It is used to identify patient care requirements and integrates the knowledge of ordinary and abnormal physiology. At times, the nursing assessment may be quite broad in scope. So, parts of the evaluation, such as the EKG’s and vitals, can be delegated to certified nursing techs or assistants.
What is a care plan?
The care plan establishes the needs of a patient and identifies how the requirements can be met by the skilled nursing facility or the healthcare system. The health assessment information also gives the health care team a better understanding of the needs of the overall patient population.
What is a health assessment?
This assessment seeks to identify the patient’s problem. A health assessment is usually a structured screening and evaluation tool deployed in primary health care practices to help the patient and the medical professional to develop a care plan. The care plan establishes the needs of a patient and identifies how ...
What is psychological exam?
A psychological exam also consists of a physical health assessment to rule out structural anomalies or damage. A focused assessment can include a cultural examination.
What is the purpose of initial assessment?
The initial assessment serves to establish the examination boundaries and duties necessary to plan and provide personalized care to a patient.
What is a good rule of thumb for forensic evaluation?
A good rule of thumb, Wright says, is to consider whether the report’s underlying assessment would meet a forensic standard. “We tend to have very high standards for forensic evaluations because they have to be defensible in court,” he says. ■ But don’t hide behind the test results.
Is it easy to write a psychological assessment report?
Developing and honing psychological assessment report writing skills is not easy, says Hadas Pade, PsyD, an assistant professor at Alliant International University’s California School of Professional Psychology in San Francisco, who co-leads workshops on writing meaningful reports.
Who is responsible for writing the medical assessment and plan?
The treatment plan must lay out the route the patient is to take on their own to care for the issue diagnosed. The clinician is responsible for writing the medical assessment and plan as well as directing the patient toward appropriate treatment.
What do medical students need to know?
Medical students must learn to write medical assessment and appropriate treatment plans. This is a skill they will use throughout their medical careers. The assessment must be concise and define the issue. The treatment plan must lay out the route the patient is to take on their own to care for the issue diagnosed.
When to include assessment in a document?
You’ll find yourself writing a lot of assessments throughout your career. Most commonly, you’ll include an assessment when completing daily notes, documenting progress notes, or writing an evaluation. But no matter the occasion, the assessment component can become the most time-consuming portion of your documentation.
What is physical therapy assessment?
A great therapy assessment accomplishes two things: It highlights the necessity for skilled therapy. It identifies areas to address in future treatments.
How to evaluate a PT?
Try following this simple outline for an evaluation assessment: 1 Restate the diagnosis 2 Remark on the patient’s rehab potential 3 Identify their key impairments 4 State why skilled PT is necessary
What are the symptoms of R hip OA?
Key impairments include: decreased ROM and strength of the left lower extremity, poor balance and compensatory gait patterning, increased swelling, and pain with functional activities such as squatting, walking, and climbing stairs. Skilled PT is required to address these key impairments and to provide and progress with an appropriate home exercise program. This evaluation is of moderate complexity due to the changing nature of the patient’s presentation as well as the comorbidities and medical factors included in this evaluation.
How long does it take to write a note for a therapist?
Without these resources, writing each note can take up to 10 minutes per patient, per day.
Do you need to write a paragraph for a skilled assessment?
You don’t need to write a paragraph for this type of documentation, but being too brief could diminish important aspects of your skilled assessment. Focus on the key elements you worked on in the session. If you targeted balance training, your assessment should reflect why.
Is assessment the most time consuming part of documentation?
But no matter the occasion, the assessment component can become the most time-consuming portion of your documentation. Learning how to write efficient, effective notes early on will save you precious time. To start, let’s look at some example therapy assessments.
Collect Information
Focused Assessment
Analyze The Patient’S Information
Comment on Your Sources of Information
Decide on The Patient Issues
Popular Posts:
- 1. tri-valley patient portal
- 2. ui family health patient patient portal
- 3. mercy patient health portal, pa
- 4. new hope patient portal
- 5. how do you report someone taking illegal drugs to a patient in the hospital
- 6. crysralpm.com patient portal
- 7. pacificamedicine patient portal
- 8. heart and vasular center of northern arizona patient portal
- 9. womens health trumbull ct patient portal
- 10. pricing strategy for patient portal