Chapter 6 Insurance In The Medical Office From Patient …
9 hours ago document patient uses to report charges and payments to insurance company. Consumer-driven health plan. plan must meet a high deductible before the health plan can make a payment. High deductible plan. type of insurance plan to verify patient's deducible,the coverage benefits and coinsurance or other financial info. >> Go To The Portal
Full Answer
What is another name for a patient Bill statement?
another name for a patient bill statement patient account that receives periodic charges open-book account document that tracks accounts by the date of last payment age analysis patient billing where accounts are split in groups with staggered statement mailing dates cycle billing money owed to other businesses by the practice
What are the different types of charges in a patient account?
- Charges for patient services - Patient co payments made at the time of service -Insurance payments received in the mail -Patient payments received in the mail -Adjustments (account write-offs and contractual allowances)
How does patient billing work in a medical practice?
patient billing where accounts are split in groups with staggered statement mailing dates cycle billing money owed to other businesses by the practice accounts payable (A/P) document signed by the patient and practice representative when a payment agreement is met, consisting of four or more payments
How will the claim be processed and paid to the provider?
If the claim is processed towards payment from payer then a check will be issued or EFT (Electronic Fund Transfer) will be done to the provider from payer along with the EOB. Claim will be paid to provider only if the patient has signed the assignment of benefits (AOB) documents.
What does patient billing information include?
This includes the name of the provider, the name of the physician, the name of the patient, the procedures performed, the codes for the diagnosis and procedure, and other pertinent medical information. This information is vital in the creation of the claim.
Which types of patient information will you need to obtain to file an insurance claim?
What patient information will you need to obtain to file and insurance claim. Insured's complete name, Insured's current employer, Patient's date of birth.
What can you do to ensure a patient pays the fees due at the time of service?
How to Collect Patient Payments at the Time of ServiceWrite an Upfront Payment Policy. ... Inform Patients of Payment Expectations. ... Check Patients' Insurance Eligibility in Advance. ... Secure a Good POS system. ... Train Front Desk Staff. ... Benefits of Collecting Payments Upfront.
What is patient responsibility on EOB?
In the insurance claim process, the “Patient Responsibility” portion of your EOB represents the “bottom line” financial responsibility of the patient in the claim process.
What is a HCFA form?
The HCFA form is what non-institutional practitioners use to bill insurance companies for services provided. The HCFA form comprises medical billing codes and the patient's demographic and insurance information. To file an HCFA form, fill in all 33 boxes and run your form through a claim scrubber to identify errors.
What is on a CMS-1500 form?
The CMS-1500 form is the standard claim form used by a non-institutional provider or supplier to bill Medicare carriers and durable medical equipment regional carriers (DMERCs) when a provider qualifies for a waiver from the Administrative Simplification Compliance Act (ASCA) requirement for electronic submission of ...
How do you collect payments from patients?
Nine tips for collecting patient balances1 Educate patients about the cost of virtual services. ... 2 Decide whether the practice will require upfront collections. ... 3 Make it easy for patients to pay. ... 4 Offer a payment plan. ... 5 Continue post-visit collections calls … ... 6 Employ enough billers or consider outsourcing.More items...•
What is another name for the office charge slip?
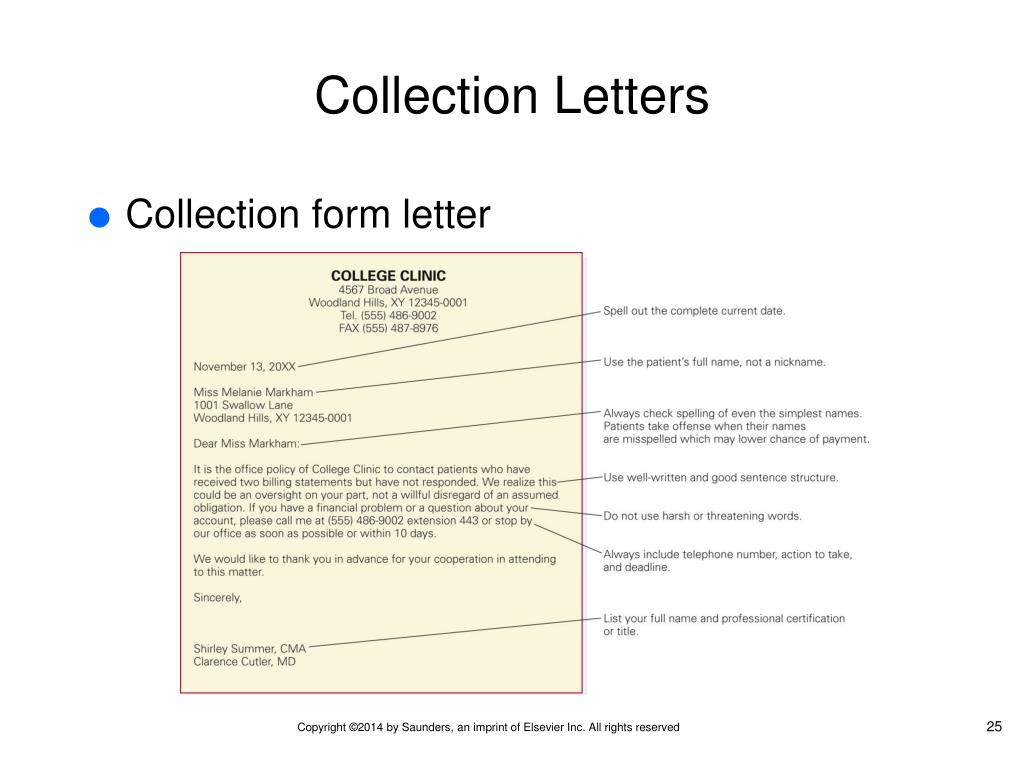
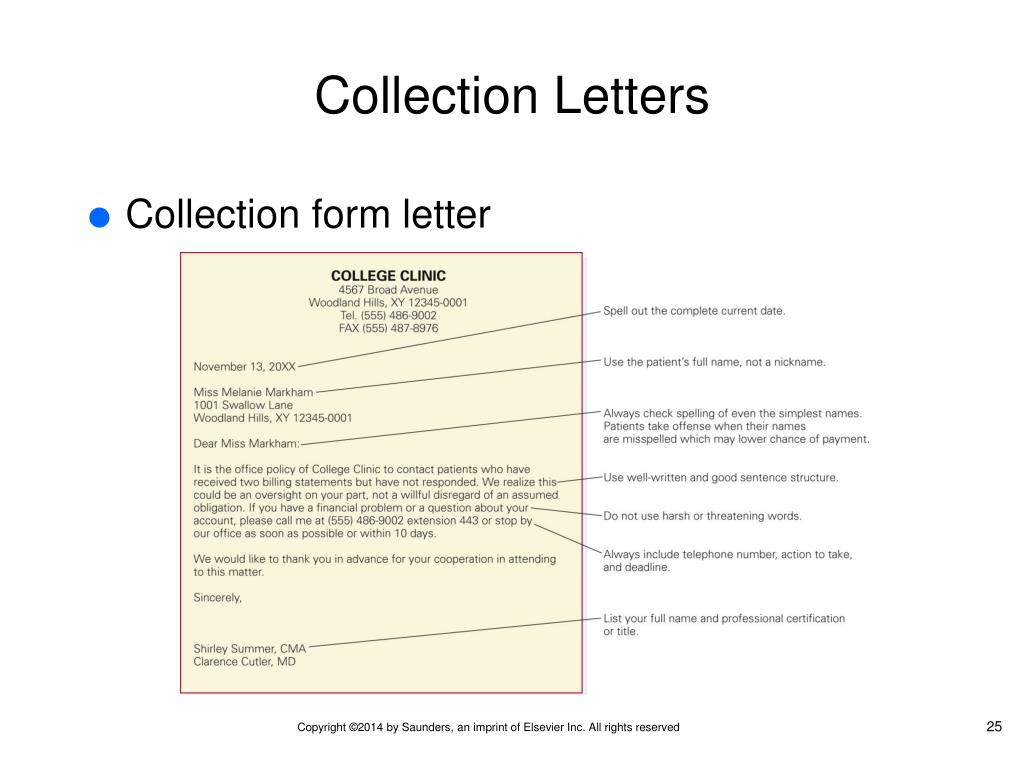
Section 5: Billing and Collections Also called a charge slip or superbill, it is generated for each patient visit and serves to communicate information about the number and type of services provided and who provided them to the system that generates bills.
How do you get a patient to pay their co pays?
6 tips for collecting co-pays and deductibles from patientsAssign the responsibility to office staff.Consider the patient experience.Avoid open-ended questions.Ask for immediate payment.Offer payment options.Maintain open communication.
What is another name for EOB?
An explanation of benefits is a statement from your health plan that lists the services you've had and how much your plan paid toward them. The EOB also shows what charges are not covered by your health plan.
What is the difference between COB and EOB in medical billing?
COB stands for “ close of business.” It refers to the end of a business day and the close of the financial markets in New York City, which define U.S. business hours. COB can be used interchangeably with end of business (EOB), end of day (EOD), end of play (EOP), close of play (COP), and close of business (COB).
What is patient responsibility in medical billing?
Defining Patient Responsibility: Patient responsibility is the portion of a medical bill that the patient is required to pay rather than their insurance provider. For example, patients with no health insurance are responsible for 100% of their medical bills.
What happens if a primary insurance payment is not posted correctly?
If the primary insurance payment is not posted correctly, it is possible for the secondary and tertiary payers may get billed out incorrectly. Inaccurate posting and billing the balances for patient that do not owe actually.
What is payment posting?
Payment posting not only consists of posting the payments to the particular patient accounts, but also involves posting the adjustments, denials and accurately billing the balance to patient. Any underpayment /denials are informed to Analyst.
When is Channagangaiah payment posting?
January 23, 2020. September 9, 2020. Channagangaiah. Payment posting also called as cash posting. After the adjudication of the claim from the payer, the claim will be either paid or denied and a document known as EOB/ EOR (Explanation of Benefits/Explanation of Review), will be sent to the healthcare provider and insured.
Popular Posts:
- 1. raleigh neurology raleigh nc, patient portal
- 2. upmc mercy electronic patient records portal
- 3. how do i sign up for the aultman medical group patient portal
- 4. forsyth peds patient portal
- 5. seaport patient portal
- 6. patient report accuracy
- 7. bu patient login
- 8. patient portal dr donna bacon
- 9. patient portal veranda
- 10. planned parenthood league of massachusetts patient portal