Transfer of Patient Care Between EMS Providers and …
2 hours ago • toIn addition a verbal report from EMS providers, the minimum key information required for patient care must be provided in written or electronic form at the time of transfer of patient care. This provides physicians and other health care providers who deliver subsequent care for the patient to receive this information more >> Go To The Portal
The patient transfer of care form is required by the EMS Act and Rules and Regulations. The Department requires the primary care provider to provide a report with the receiving facility at the time of the patient's transfer of care. The report must be given verbally and in a written format.
Full Answer
How should EMS transfer of care documentation be treated?
EMS transfer of care documentation should be treated as part of the health care record and must be professional, accurate, and consistent with information included in the final complete electronic or written EMS patient care report. Hospital systems should preserve written transfer of care documentation in the patient’s permanent medical record.
When is the EMS patient care report available to the receiving facility?
In addition to the information exchanged contemporaneously at the time of transfer of patient care, the complete EMS patient care report must be available to the receiving facility within a clinically relevant period of time.
How should health care facilities respond to patient care transfer reports?
Health care facilities should attempt to receive patient care transfer reports in a timely manner, facilitating the return of EMS units to service.
What is the relationship between Ems and the healthcare team?
All members of the health care team, including EMS providers, nurses, and physicians, must communicate with mutual respect for each other and respect the verbal and written communication from EMS as an important part of the patient’s history.

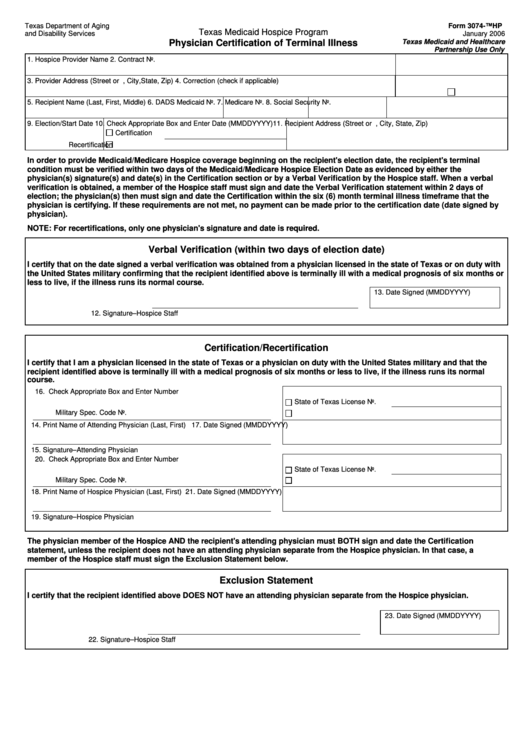
How do you transfer a patient from one hospital to another in Texas?
Any transfer to another medical facility of an individual with an EMC must be initiated either by a written request for transfer from the individual or the legally responsible person acting on the individual's behalf or by a physician order with the appropriate physician or QMP and Physician certification as required ...
How do I write a patient care report in EMS?
EMS providers just need to pull the information together and write it down in a way that paints a picture....Follow these 7 Elements to Paint a Complete PCR PictureDispatch & Response Summary. ... Scene Summary. ... HPI/Physical Exam. ... Interventions. ... Status Change. ... Safety Summary. ... Disposition.
What do you need to report when handing off a patient?
The SBAR ReportSituation—Identify the general problem and any focused priority.Background—Focused history of present issue/injury, prior care and relevant history.Assessment—Key findings and vital signs, including the patient's current state.Recommendation—Identify the patient's immediate needs, if any.
When should patient care report be completed?
Writing the PCR as soon as possible after the call will help make sure it is as accurate as possible. If it is not possible to write the PCR as soon as the call is over, simply taking some notes on the call, and then using those notes later when completing the PCR can ensure accuracy.
How do you write an ePCR?
How to Write an Effective ePCR NarrativeBe concise but detailed. Be descriptive in explaining exactly what happened and include the decision-making process that led to the action. ... Present the facts in clear, objective language. ... Eliminate incorrect grammar and other avoidable mistakes. ... Be consistent and thorough.
When you document information on a patient that you treat and care for this written report is called the?
When you document information on a patient that you treat and care for. This written report is called the: Patient care report, run report.
How do I give a good handoff report to EMS?
0:185:41Patient Handoff Report Skills | EMT | V28 - YouTubeYouTubeStart of suggested clipEnd of suggested clipHaving an organized or systematic approach to patient handoff reports is a great way to get startedMoreHaving an organized or systematic approach to patient handoff reports is a great way to get started in practice.
What is sbar handoff?
Situation, Background, Assessment, Recommendation (SBAR) is a mnemonic used to structure information sharing to avoid communication failures during handoffs.
What is EMS handoff?
The patient's vital signs are reportedly within normal limits, so she is triaged to a regular room in the emergency department where handoff is given from paramedic to nurse. The physician, who is in another room, is not present for the signout. Ten minutes later, the physician walks into the room to see the patient.
What is a PCR report?
PCR means polymerase chain reaction. It's a test to detect genetic material from a specific organism, such as a virus. The test detects the presence of a virus if you have the virus at the time of the test. The test could also detect fragments of the virus even after you are no longer infected.
What is a PCR document?
The PCR documentation is considered a medical document that becomes part of the patient's permanent medical record. It is also considered a legal document in cases where liability and/or malpractice issues arise. It is the source in which all medical billing claims are based.
What is a PCR in writing?
The PARCC Summative Assessments in Grades 3-11 will measure writing using three prose constructed response (PCR) items. In the classroom writing can take many forms, including both informal and formal.
What is the role of EMS in the transfer of patient care?
During the transfer of patient care, the receiving health care providers should have an opportunity to ask questions to clarify information that is exchanged.
When must an EMS patient care report be available?
In addition to the information exchanged contemporaneously at the time of transfer of patient care, the complete EMS patient care report must be available to the receiving facility within a clinically relevant period of time.
What should an EMS developer do?
Developers of electronic EMS patient care reports and health information exchanges should develop products that efficiently provide real-time digital transfer and preservation of the transfer-of-care documentation into the patient medical record.
What information is required for EMS?
In addition to a verbal report from EMS providers, the minimum key information required for patient care must be provided in written or electronic form at the time of transfer of patient care. This provides physicians and other health care providers who deliver subsequent care for the patient to receive this information more accurately and avoid potential errors inherent with second-hand information. The minimum key information reported at the time of hand-off must include information that is required for optimal care of the patient – examples include vital signs, treatment interventions, and the time of symptom onset for time-sensitive illnesses.
Do hospitals have to keep transfer of care records?
Hospital systems should preserve written transfer of care documentation in the patient’s permanent medical record. Copies of all results of medical tests performed by EMS providers (eg 12-lead ECGs, results of blood chemistry testing, any medical imaging, etc) must be available to the receiving facility with the EMS transfer-of-care documentation.
Should health care facilities receive patient care transfer reports in a timely manner?
Health care facilities should attempt to receive patient care transfer reports in a timely manner, facilitating the return of EMS units to service.
Who assumed patient care at the scene and prepared patient for transport via air medical?
For example, “Patient care was transferred to flight paramedic J. Smith who assumed patient care at the scene and prepared patient for transport via air medical.”
What to include in a document for a patient?
Include documentation of outcomes, treatments provided, interventions and procedures undertaken during transport . Especially note when the patient provides updates about how they feel, better or worse, and the steps you have taken to mitigate any new developments.
What is flow chart in PCR?
The flow chart allows the author of the PCR to record events in the order they occurred and apply a time stamp to those events. This is the common area of the PCR where vital signs are recorded along with numeric values for oxygen saturation, Glascow Coma Scale numbers and the like. Most ePCR programs have an area to record notes about what was taking place at various times in the incident, as well.
Can you transfer care to another person?
There are times when you must transfer care to another individual. Of course, protocol will dictate that you turn over care to another healthcare provided who is equally or higher trained in most cases. Be sure to document who you turned over care to when doing so in the field and what their level of training was.
What is the complaint acknowledgment letter for EMS?
Unless the complaint was filed anonymously, the complainant should receive a complaint acknowledgment letter that includes a tracking number, contact name and phone number.
How to check EMS certification?
go to www.dshs.state.tx.us/emstraumasystems/newcert.shtm. Click on “Public License Search”.
What is DSHS in Texas?
The Texas Department of State Health Services (DSHS), EMS Compliance Unit, investigates complaints made against Emergency Medical Services (EMS) personnel, EMS providers, EMS first responder organizations, EMS education programs, EMS course coordinators, and EMS instructors, that involve possible violations of the Emergency Healthcare Act at Chapter 773 of the Health and Safety Code and Department’s EMS Rules at Chapter 157 of the Texas Administrative Code .
How long does an EMS investigation take?
The amount of time varies for each investigation and is dependent on a myriad of factors including the complexity of a case and circumstances that may be out of the control of the investigator or the EMS personnel, provider, and or other EMS entities under investigation.
Where to file complaints regarding billing in Texas?
Billing issues (rates/collection procedures). These complaints should be referred to the Te xas Attorney General’s Office Consumer Complaints Division.
Who can report HIPAA violations?
Public Health Information Violations/HIPAA- These issues can be reported to US Department of Health and Human Services Office of Civil Rights (OCR).
How to contact DSHS?
The DSHS Complaint Form is available to either download ( PDF) or requesting a copy to be sent by calling 512-834-6765.
Hands On
This is the part of your Patient Care Report where you record in words the treatments provided to your patient.
Why Is Transportation by any other Means Contraindicated?
Documenting treatments goes a long way to answering the vital medical necessity question; “Why is transportation by any other means contraindicated for this patient?
Outcomes
When explaining treatments the logical progression is to then explain the outcome of that treatment, be it positive or negative.
Another Piece of the Puzzle
There you have it. Another piece to the PCR puzzle has been provided to you. Over the past ten weeks we have been dissecting important elements that must be recorded as part of the PCR you write and turn into the billing office for billing of the claim for payment.
Not a Client?
We’re just waiting for you to contact us. Visit our website and click on the “Get Started” button. Submit your contact information to us and we’ll be in touch to talk with you about the many ambulance billing features we offer to benefit you as a potential client!
Thanks for joining us!
Today marks the first in our Documentation 101 blog series. Using the next several blog postings, we’ll be attempting to put together a few coaching blogs to help all of you become better EMS documenters.
Maybe you need some basic writing help?
There’s nothing wrong in admitting that you need help. You can even better yourself, personally, by learning to communicate in writing more effectively. There are tons of self-help tools on the Internet to assist you with writing and grammar skills.
To the Rescue!
We’re not finished. As part of this documentation series, we’ll include some specific steps to make you a better documenter. Make your goal to be the best documenter that your department has and you’re well on your way to PCR writing success.
Not a client?
No problem there. Check out our website right now and complete the “Get Started” section so we can connect. We’d love to talk to you about the many features and how they can benefit your EMS Department!
What Is a Patient Care Report?
We often hear of care reports based on by medical teams or by medical authorities. Yet, we are not sure how this differs from the kind of report that is given to us by the same people. So this is the time to make it as clear as possible.
How to Write a Patient Care Report?
Where do you even begin when you write a patient care report? A lot of EMS or EMTs do know how to write one since they are trained to do so.
What is a patient care report?
A patient care report is a document made mostly by the EMS or EMTs. This documented report is done after getting the call. This consists of the information necessary for the assessment and evaluation of a patient’s care.
What should not be written in a patient care report?
What should be avoided in a patient care report is making up the information that is not true to the patient. This is why you have to be very careful and very meticulous when writing these kinds of reports. Every detail counts.
Who is in charge of reading the patient care report?
The person or the people who will be reading the report are mostly medical authorities. When you are going to be passing this kind of report, make sure that you have all the information correctly. One wrong information can cause a lot of issues and problems.
Popular Posts:
- 1. rutgers caps patient portal
- 2. mass general brigham login
- 3. candlewood women's health patient portal
- 4. blood report of leukemia patient
- 5. memorial hermann my patient portal
- 6. brmc bluefield wv patient portal
- 7. baptist hospital san antonio patient portal
- 8. patient portal leo toupin
- 9. aarp medicare plan patient portal
- 10. sghs patient portal