A Step-by-Step Guide to Implementing a New Patient Portal
6 hours ago 7 Steps to Implement a New Patient Portal Solution 1. Research different solutions. It’s never wise to select the first tool you come across no matter how promising it may... 2. Look for the right features. When researching potential solutions, look for … >> Go To The Portal
7 Steps to Implement a New Patient Portal Solution.
- 1. Research different solutions. It’s never wise to select the first tool you come across no matter how promising it may appear. Do your research, ...
- 2. Look for the right features. When researching potential solutions, look for the features and benefits that are most important for your practice and ...
- 3. Get buy-in from key stakeholders. Before you move forward with implementing new patient portal technology, getting buy-in from all key stakeholders ...
- 4. Evaluate and enhance existing workflows. Leading patient portals should differentiate themselves by providing proficiencies to your practice ...
- Research different solutions. ...
- Look for the right features. ...
- Get buy-in from key stakeholders. ...
- Evaluate and enhance existing workflows. ...
- Develop an onboarding plan. ...
- Successful go-live. ...
- Seek out painless portal migration.
How to get your patients to use your patient portal?
7 Steps to Implement a New Patient Portal Solution 1. Research different solutions. It’s never wise to select the first tool you come across no matter how promising it may... 2. Look for the right features. When researching potential solutions, look for …
How to create an account in our patient portal?
Download PDF. Why implement a patient portal? For practices with a website, a portal could be the next logical step. It can improve practice efficiency by allowing patients to go online to schedule appointments, preregister, pay bills, review information from their charts, and receive educational materials—all activities that otherwise would be done over the phone or in person …
How do I enroll in the patient portal?
Mar 21, 2022 · First, figure out what challenges you need your patient portal to solve. To do this, survey your staff to see what hurdles they experience with patient care and communication to see if a patient portal will help alleviate some of those …
How to access your patient portal?
Get your comprehensive guide to successfully choosing and implementing a patient portal and ensuring patient adoption. Learn the 4 key steps to successfully implementing a patient portal. This eBook will show you how to: Prepare a solid plan; Select and implement the right solution; Market and build adoption; Determine if you have the right resources for implementation
What must be done when creating a patient portal?
4 Steps to Successful Patient Portal Adoption, IntegrationOutline clinic or hospital needs, goals.Select a patient portal vendor.Create provider buy-in.Market the patient portal to end-users.Jun 6, 2017
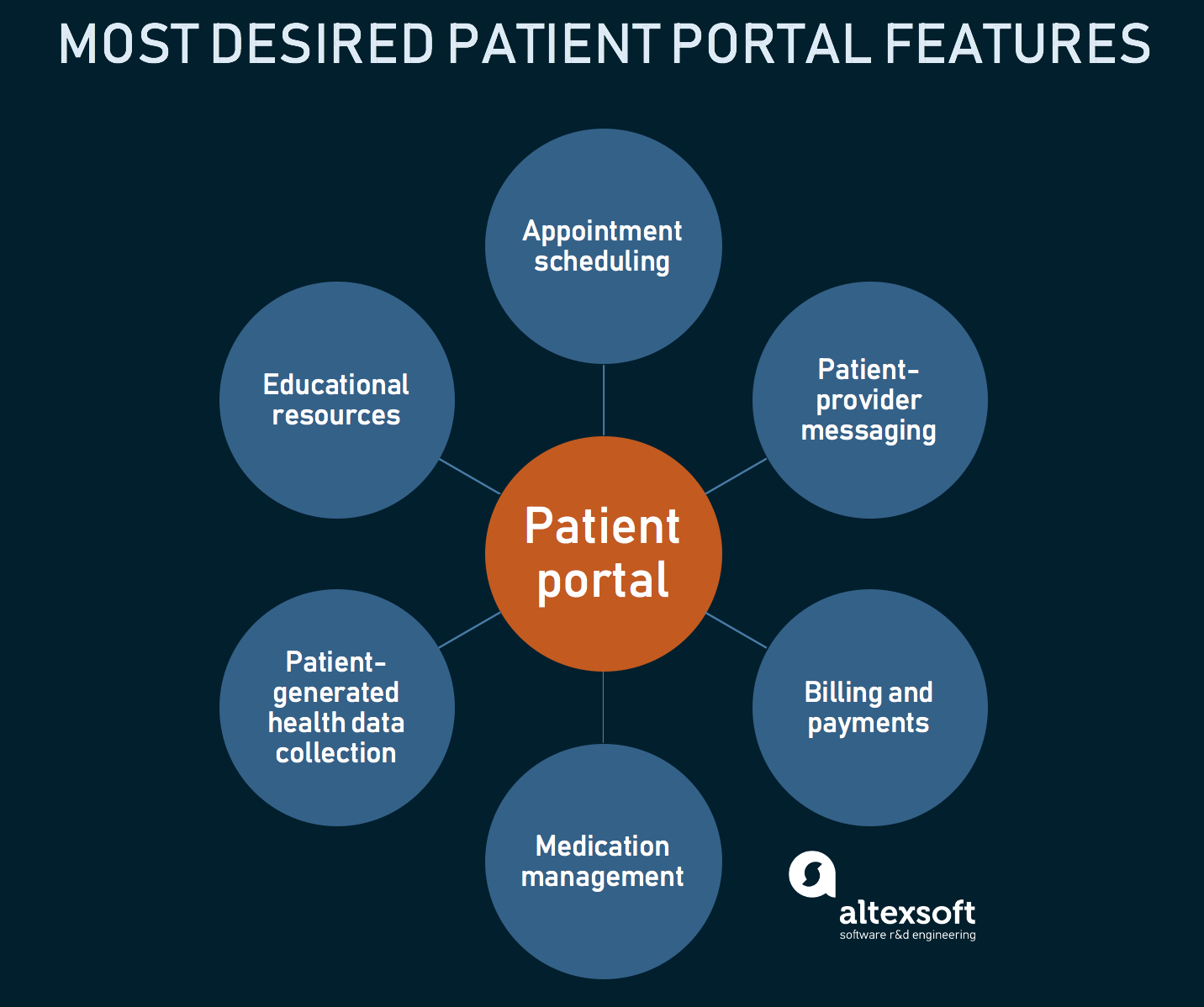
What elements should be incorporated into a patient portal?
A robust patient portal should include the following features:Clinical summaries.Secure (HIPAA-compliant) messaging.Online bill pay.New patient registration.Ability to update demographic information.Prescription renewals and contact lens ordering.Appointment requests.Appointment reminders.More items...
What is the nurse's role in implementation of patient portals in healthcare?
Nurses see the portal as an additional service for patients, because it offers them the possibility for asking questions at any time and place suitable for the patient. Some nurses experience an increase in work load, because patients ask more non-urgent questions that otherwise would not be asked.Jun 15, 2012
How do you optimize patient portals for patient engagement?
Make enrollment open to all patients. Have staff manage portal workflow and communication before engaging providers directly. Aim to establish efficient workflows and policies, and avoid burdening providers with troubleshooting during initial rollout. The whole staff should be involved in promoting the patient portal.
What are the benefits and challenges of using patient portals?
What are the Top Pros and Cons of Adopting Patient Portals?Pro: Better communication with chronically ill patients.Con: Healthcare data security concerns.Pro: More complete and accurate patient information.Con: Difficult patient buy-in.Pro: Increased patient ownership of their own care.Feb 17, 2016
What is the purpose of the nhin?
The nationwide health information network (NHIN) is a set of standards, services and policies that enable secure health information exchange over the Internet. The network will provide the foundation for the exchange of health information across diverse entities, within communities and across the country.Dec 29, 2010
What is a patient portal How will the patient portal enhance the quality of care?
Background. Engaging patients in the delivery of health care has the potential to improve health outcomes and patient satisfaction. Patient portals may enhance patient engagement by enabling patients to access their electronic medical records (EMRs) and facilitating secure patient-provider communication.
Is a patient portal an EHR?
Electronic health record (EHR) patient portals provide a means by which patients can access their health information, including diagnostic test results. Little is known about portal usage by emergency department (ED) patients.
Benefits of a Patient Portal
Staff will spend less time on data entry. When you consider that registration information must be provided by every patient, you quickly realize the enormous amount of time your office staff spends entering that data into your computer system.
Portals and EHR Meaningful Use
With 2014 just around the corner, practices that are moving on to Stage 2 of the federal meaningful use (MU) incentive program must prepare to meet the new re-quirements.
Get Prepared for a Portal
Start early. It takes considerable time to introduce your patients to the features available through your portal—and even longer to get them into the habit of using it regularly. “We knew that we had to embrace this new technology as part of the MU requirements and did not want to wait until the last minute to begin implementation,” said Ms.
Going Live
When your patient portal goes live, should you roll out multiple features all at once or implement one component at a time?
Usability Is Critical
Patient portals must be user friendly to sustain continued patient use. If your practice’s portal is not intuitive or if it is too cumbersome to move through the options, you’ll find your patients will avoid using it. “Our portal is provided by one of several third-party vendors that work directly with our EHR vendor,” said Ms. Woodke.
What is the stage 1 requirement for a patient?
Stage 1. Required Provide patients with clinical summaries for each office visit within 3 business days. This is required for more than 50% of all office visits during the reporting period. Required Provide patients with an electronic copy of their health information upon request.
What is Stage 2 of CMS EHR?
One of the most talked about changes with Stage 2 of the CMS EHR Incentive Program, is the requirement that your patients interact with their health information and communicate with you or your practice electronically. (See Appendix A for the patient engagement requirements.) This requires additional technology to enable the secure sharing of health information and the associated tracking to generate the Meaningful Use reporting. Along with that, you will need to find a way to share the message with your patients that you want to interact electronically and have the ability to do so.
How to get the most value from an EHR?
To get the most value from an EHR, practices will need to invest time in training and preparation. Some customization of the system will likely be needed based on how the practice functions and the individual work styles of the various providers.
How long does it take for a nurse to respond to a patient?
The practice established standards for response times of within 4 hours for more urgent questions to 2 days for prescription refills
Step 1: Improve documentation and coding
The most recent all-payer data available (which are admittedly old, being from 2002 and 2003) 3 show the average family physician coding established patient visits in the following distribution:
Step 2: Hire more nurses or medical assistants
Six to 12 months of coding improvement should get revenue to the point where you can afford to hire enough nurses to raise the nurse-to-doctor ratio to between 1.5 and 1.75.
Step 3: Implement advanced-access scheduling
This step, which requires being able to see patients the day they call for an appointment, could be taken at any time, but I suggest that you wait six months after the extra nurses are hired to give physicians and staff some breathing room before taking it on. There is little direct cost to making the transition other than physician and staff time.
Step 4: Increase the number of patients you see per day
The typical family physician sees 20 to 25 patients per day. Increasing this by five per day could bring in an additional $85,000 annually, and increasing by 10 per day could bring in $170,000, assuming optimal coding distribution and Medicare payment rates.
Step 5: (Optional) Expand hours
If your practice includes two or more physicians who can share the load, you might want to consider keeping your office open some evenings (until 7 p.m., say) and Saturday mornings.
Step 6: Buy and implement an EHR
About six months after increasing the number of patients physicians see per day, you should have the cash flow to take on this expensive step. The hardware and software can cost up to $25,000 per physician, the maintenance is not cheap, and the new system will cut productivity until everyone is fully trained and used to it.
Step 7: Start doing systematic, population-based care
Once you have a high-functioning team and you've used your EHR system long enough to be comfortable with it, you're ready to start providing a level of care that few family medicine practices can attain today – building chronic disease patient registries, implementing some version of the chronic care model and developing proactive, population-level strategies for preventive care.

Popular Posts:
- 1. rita kimball patient portal
- 2. seton family of doctors internal medicine patient portal
- 3. patient portal pcc
- 4. st mary's livonia patient portal
- 5. sunrise medical patient portal
- 6. patient portal analyst progressive
- 7. einstein hospital patient portal philadelphia
- 8. patient portal elmhurst hospital
- 9. ihs patient portal
- 10. orthoneuro patient portal