How to Communicate with Emergency Services Using a …
11 hours ago Vitals taken, O2 @ 4LPM via nasal canula, manual immobilization, c-collar, backboard, patient’s condition improved following treatment (identify which treatment) S. A MPLE REPORT (S) - PT. states his chief complaint is a substernal chest pain lasting 2 hours. PT. states he was sitting at home watching the game as this pain came on acutely. >> Go To The Portal
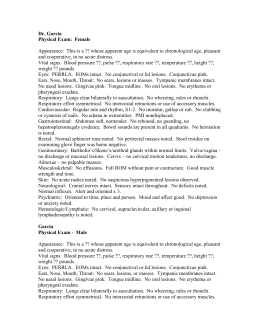
The second component of your SOAP Note includes objective findings and observations of the patient’s current state. Make note of the position you found your patient in, or that you were in, following the MOI. Then, provide details about pertinent findings, or pertinent negatives, found during your patient exam.
Full Answer
How to document a patient assessment (soap)?
How to Document a Patient Assessment (SOAP) 1 Subjective. The subjective section of your documentation should include how... 2 Objective. This section needs to include your objective observations,... 3 Assessment. The assessment section is where you write your thoughts on the salient issues and... 4 Plan. The final section is the plan,...
What are soap report skills and why do you need them?
Strong SOAP report skills can help you communicate accurately and concisely with a healthcare professional so they can decide the best possible way to provide treatment while considering many other patients. Like any other skill taught on wilderness medicine courses, giving a SOAP note needs to be practiced.
What are SOAP notes in nursing?
SOAP notes are ways that nurses organize information about patients for other healthcare professionals. Discover more about what SOAP notes are, learn what the acronym SOAP stands for, and examine a sample scenario. Updated: 11/02/2021 What Are SOAP Notes?
Why is it important to have a soap in a hospital?
It is essential as proof that the patient is being treated regularly and effectively by different people. SOAP is actually an acronym and it stands for: S ubjective – This basically refers to everything the patient has to say about the issue, concern, problem and intervention procedures.
How do you write a soap report?
Tips for Effective SOAP NotesFind the appropriate time to write SOAP notes.Maintain a professional voice.Avoid overly wordy phrasing.Avoid biased overly positive or negative phrasing.Be specific and concise.Avoid overly subjective statement without evidence.Avoid pronoun confusion.Be accurate but nonjudgmental.
What should be included in a SOAP note assessment?
The 4 headings of a SOAP note are Subjective, Objective, Assessment and Plan....This includes:Vital signs.Physical exam findings.Laboratory data.Imaging results.Other diagnostic data.Recognition and review of the documentation of other clinicians.
How do you write a nursing SOAP note?
0:105:59So stands for subjective objective assessment and plan let's take a look at each of the fourMoreSo stands for subjective objective assessment and plan let's take a look at each of the four components. So you can understand this neat and organized way of note-taking.
What is the SOAP note format?
The answer would be Subjective, Objective, Assessment and Plan, respectively. The standardized format of the SOAP note template guides practitioners through assessing, diagnosing, and treating a client based on the information in each of the note's sections.
What are the 4 parts of soap?
The acronym SOAP stands for Subjective, Objective, Assessment, and Plan.
What do you write in the objective of a SOAP note?
Objective means that it is measurable and observable. In this section, you will report anything you and the client did; scores for screenings, evaluations, and assessments; and anything you observed. The O section is for facts and data.
What are SOAP notes nursing?
SOAP notes are a way for nurses to organize information about patients. SOAP stands for subjective, objective, assessment and plan. Nurses make notes for each of these elements in order to provide clear information to other healthcare professionals.
What is a nurse SOAP note?
Nurses and other healthcare providers use the SOAP note as a documentation method to write out notes in the patient's chart. SOAP stands for subjective, objective, assessment, and plan. Let's take a look at each of the four components so you can understand this neat and organized way of note-taking.
What should a nursing note include?
Elements to include in a nursing progress noteDate and time of the report.Patient's name.Doctor and nurse's name.General description of the patient.Reason for the visit.Vital signs and initial health assessment.Results of any tests or bloodwork.Diagnosis and care plan.More items...•
What are 3 guidelines to follow when writing SOAP notes?
However, all SOAP notes should include Subjective, Objective, Assessment, and Plan sections, hence the acronym SOAP.
Where do medications go in a SOAP note?
If the purpose of the SOAP note is to review overall patient progress (e.g., medication reconciliation, medication therapy management), then all current medications (prescription, non-prescription) and non- drug therapy must be listed in the note's S or O section.
Subjective
The subjective section of your documentation should include how the patient is currently feeling and how they’ve been since the last review in their own words.
Objective
The objective section needs to include your objective observations, which are things you can measure, see, hear, feel or smell.
Assessment
The assessment section is where you document your thoughts on the salient issues and the diagnosis (or differential diagnosis), which will be based on the information collected in the previous two sections.
Plan
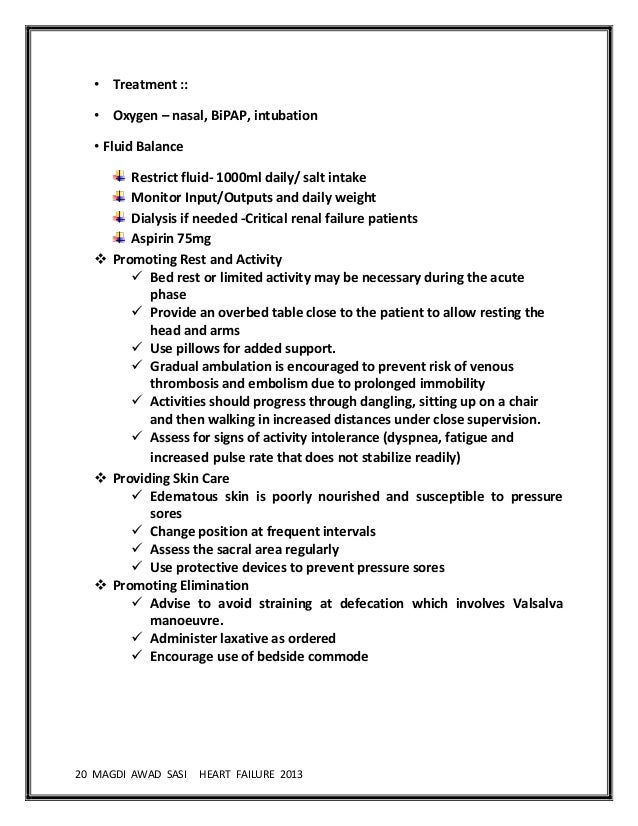
The final section is the plan, which is where you document how you are going to address or further investigate any issues raised during the review.
Why are soap notes still used?
SOAP notes have been around for some time now and because of their efficiency and functionality, they are still being used now. The very first SOAP note template was created and developed by a brilliant doctor named Lawrence Weed way back in the 1960s. It was done at the University of Vermont as an element of the POMR (Problem-Oriented Medical Record). During those times, objective documentation did not exist so physicians had the tendency to make decisions about treating patients without scientific basis.
What is a soap note?
SOAP notes are a type of documentation which, when used, help generate an organized and standard method for documenting any patient data. Any type of health professionals can use a SOAP note template – nurse practitioners, nurses, counselors, physicians, and of course, doctors. Using these kinds of notes allows the main health care provider ...
What is a soap note template?
A SOAP note template comes in a very structured format though it is only one of the numerous formats health or medical professionals can use. A SOAP note template by a nurse practitioner or any other person who works with the patient enters it into the patient’s medical records in order to update them.
What is the purpose of assessment?
The main purpose of the patient’s medical visit is to seek treatment and so the assessment should contain all the symptoms stated by the patient along with the diagnosis of the illness or injury.
What is the oldest method of documentation?
Written and narrative notes are the oldest and most enduring method for documentation so chances are, the majority of health professionals are familiar with them. Though there are different formats for documentation, SOAP notes are the most organized, structured and easy to understand.
What is a soap note?
A SOAP note is a documentation method used by medical practitioners to assess a patient’s condition. It is commonly used by doctors, nurses, pharmacists, therapists, and other healthcare practitioners to gather and share patient information. SOAP notes are designed to improve the quality and continuity of patient care by enhancing communication ...
What is the best software to collect SOAP notes?
Healthcare professionals can use iAuditor, the world’s #1 inspection software, to digitally gather SOAP notes and improve the quality and continuity of patient care. Collect photo evidence for a more informative and descriptive patient record.
What Are SOAP Notes?
Nurses may feel they are given a huge basket of dirty laundry to wash when taking care of patients. They are presented with a lot of different information that needs to be gathered and sorted through before carrying out specific interventions.
What Does SOAP Stand For?
There are four components that form these notes that make up the acronym S-O-A-P:
The Basics
Subjective
- This component of your SOAP note includes information about the event/injury provided by the patient or bystanders, what you see that gives you a sense of the situation, and the summary/story of what happened.
Objective
- The second component of your SOAP Note includes objective findings and observations of the patient’s current state. Make note of the position you found your patient in, or that you were in, following the MOI. Then, provide details about pertinent findings, or pertinent negatives, found during your patient exam.
Assessment
- The third component of your SOAP report is the assessment, which is where you convey the problem listto the healthcare professional. By using your wilderness medicine education you to associate signs/symptoms to possible ailments, you can deduce your patient’s most pressing issues.
Plan
- This is where you outline your beginning treatment plan. You should convey to the caretaker on the phone what treatment you’ve begun taking, as well as possible steps you plan to take. While your wilderness medicine training gives you the tools to create an educated treatment plan, be sure to follow whatever steps the emergency responders on the phone recommend. This will be …
Final Thoughts
- The COVID-19 pandemic has no boundaries, so now’s the time to assess how to transition your wilderness medicine skills from the backcountry to the frontcountryso you can provide much needed support for our medical services. Strong SOAP report skills can help you communicate accurately and concisely with a healthcare professional so they can decide the best possible wa…
What Are The Four Parts of A Soap Note?
Soap Note Example – How to Write & What Format
Use A Template For Your Notes
Popular Posts:
- 1. albany endocrinology patient portal
- 2. getting people to use a patient portal
- 3. centricity patient portal login heart institute
- 4. marine park radiology patient portal
- 5. mt graham regional medical center patient portal
- 6. borgess patient portal registration form
- 7. patient portal ubmc
- 8. long island urgent care patient portal
- 9. virginiaphycians,inc. patient portal
- 10. moga patient portal